Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3844
Peer-review started: June 19, 2019
First decision: September 23, 2019
Revised: October 4, 2019
Accepted: October 15, 2019
Article in press: October 15, 2019
Published online: November 26, 2019
Processing time: 165 Days and 17.4 Hours
Situs inversus totalis (SIT) is a rare congenital condition that is characterized by a complete mirror image of the typical arrangement of the thoracic and abdominal viscera. Performing thoracoscopic segmentectomy for a patient with lung cancer and SIT is an extremely skilled and challenging surgical procedure.
A 41-year old woman with a medical history of dextrocardia since childhood was admitted to our hospital with a mixed ground-glass opacity (mGGO) in her left lung field, discovered by computed tomography during her health checkup. In order to facilitate surgical orientation, three-dimensional computed tomography bronchography and angiography (3D-CTBA) was preoperatively carried out. The result of 3D-CTBA was consistent with the diagnosis of SIT and an mGGO in the posterior segment of the left upper lobe (LS2). Surgery was conducted in accordance with preoperative 3D-CTBA and designed surgical procedure, combined with intraoperative navigation. Final pathological examination revealed in situ adenocarcinoma. The patient’s postoperative condition was uneventful and no complications were observed.
We present the first case of lung cancer in a patient with SIT who successfully underwent thoracoscopic segmentectomy assisted by 3D-CTBA. This is a new technique that covers precise confirmation and dissection of targeted structures and intersegmental demarcation, and can help achieve a meticulous anatomical segmentectomy.
Core tip: Situs inversus totalis (SIT) is a rare congenital condition that is characterized by a complete transposition of major visceral organs. Surgical techniques in SIT patients are challenging as a result of their mirrored anatomy. A thorough understanding of segmental anatomy is thus important to avoid intraoperative accidental injuries. The three-dimensional computed tomography bronchography and angiography combined with image reconstruction with OsiriX software was found to be useful for image training before and during the surgery.
- Citation: Wu YJ, Bao Y, Wang YL. Thoracoscopic segmentectomy assisted by three-dimensional computed tomography bronchography and angiography for lung cancer in a patient living with situs inversus totalis: A case report. World J Clin Cases 2019; 7(22): 3844-3850
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3844.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3844
Situs inversus totalis (SIT) is a rare congenital condition that occurs in an estimated 1 in 10000 people[1]. This abnormality affects all major structures within the thorax and abdomen, where major visceral organs are completely mirrored to their opposite anatomic positions. In addition, anatomical variations are more frequent than in the general population. SIT with lung cancer has rarely been reported. Herein, we present the rare case of a patient with SIT who successfully underwent thoracoscopic segmentectomy for lung cancer. Thoracoscopic segmentectomy for patients who are complicated by SIT requires particular attention from the surgeon, heralding a sizeable surgical challenge and the need for more sophisticated operations.
There are still technical pitfalls that must be overcome to achieve a meticulous and safe segmentectomy. Different imaging technology and construction software have been developed as powerful tools for the surgeons to determine anatomical structure[2-4]. Computed tomography angiography (CTA) has been established as a non-invasive, high-quality imaging tool for the evaluation of vascular structure[2]. The drawbacks of CTA in the application in the lungs are lack of stereoscopic vision, complexity of bronchial reconstruction, and exposure to ionizing radiation[2-3]. To facilitate surgical orientation and improve manipulating accuracy, we made use of three-dimensional computed tomography bronchography and angiography (3D-CTBA) to analyze anatomical variations, detect the exact location of the lung nodule, and ensure sufficient surgical margin[5-7]. To the best of our knowledge, this is the first report of thoracoscopic segmentectomy assisted by 3D-CTBA for lung cancer in a patient with SIT.
A 41-year-old woman was hospitalized for a mixed ground-glass opacity (mGGO) in the left lung field.
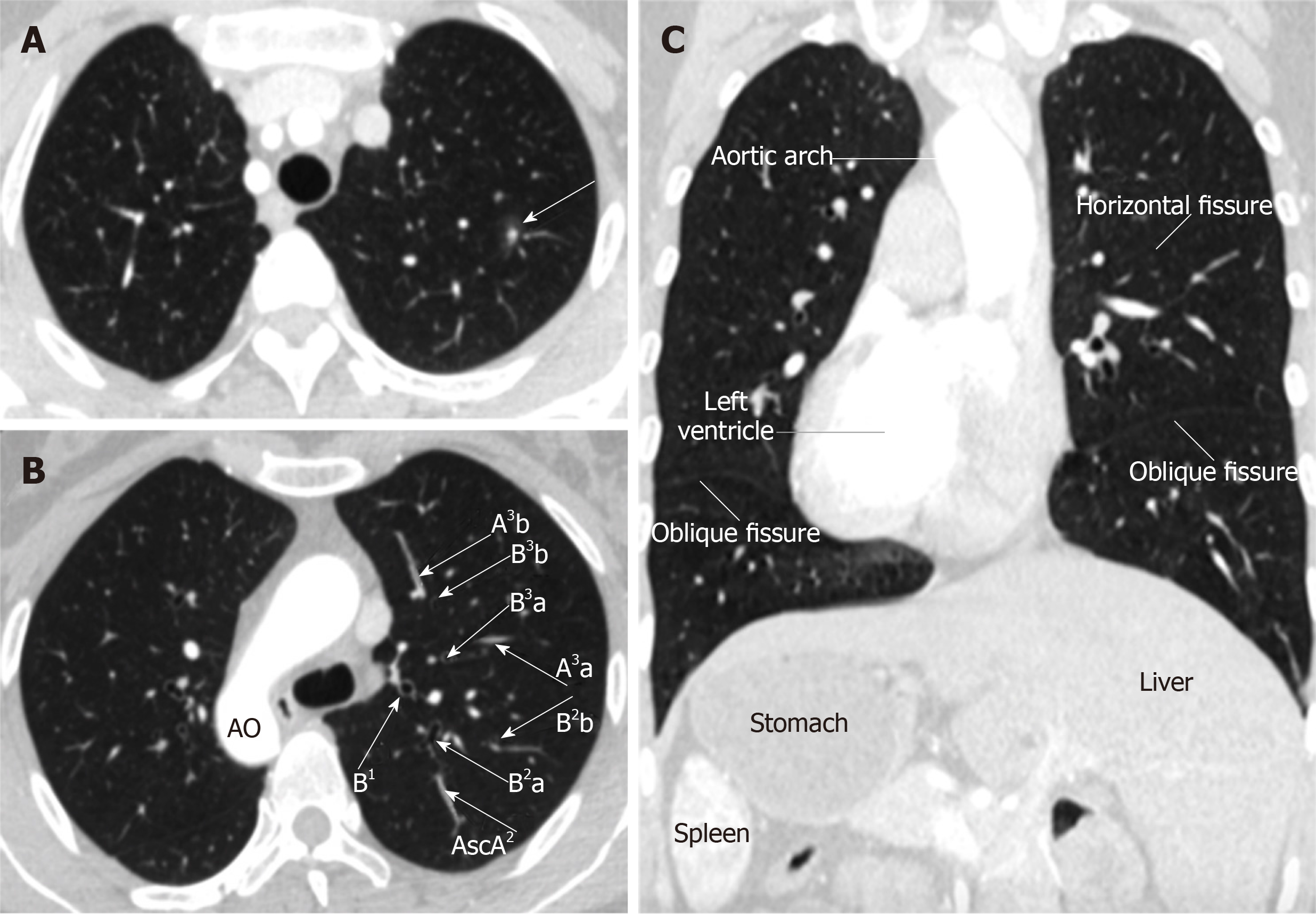
The woman was admitted to our hospital on October 31, 2018 with an mGGO found by computed tomography during her routine health checkup (Figure 1). She had no recent history of fever, muscle ache, cough, chest pain, hoarseness, dyspnea, or blood sputum.
The patient had, since childhood, a previous medical history of dextrocardia. However, she was free of Kartagener syndrome.
The patient had no history of smoking or drug abuse. Her mother died of lung adenocarcinoma while her father died of gastric cancer.
On admission, her body temperature was 36.3 °C , pulse rate was 74 beats/min, respiration rate was 18 breaths/min, and blood pressure was 130/80 mmHg. Laboratory findings showed the serum tumor markers were within normal limits. The patient’s physical examination and results of blood examination revealed no abnormal findings.
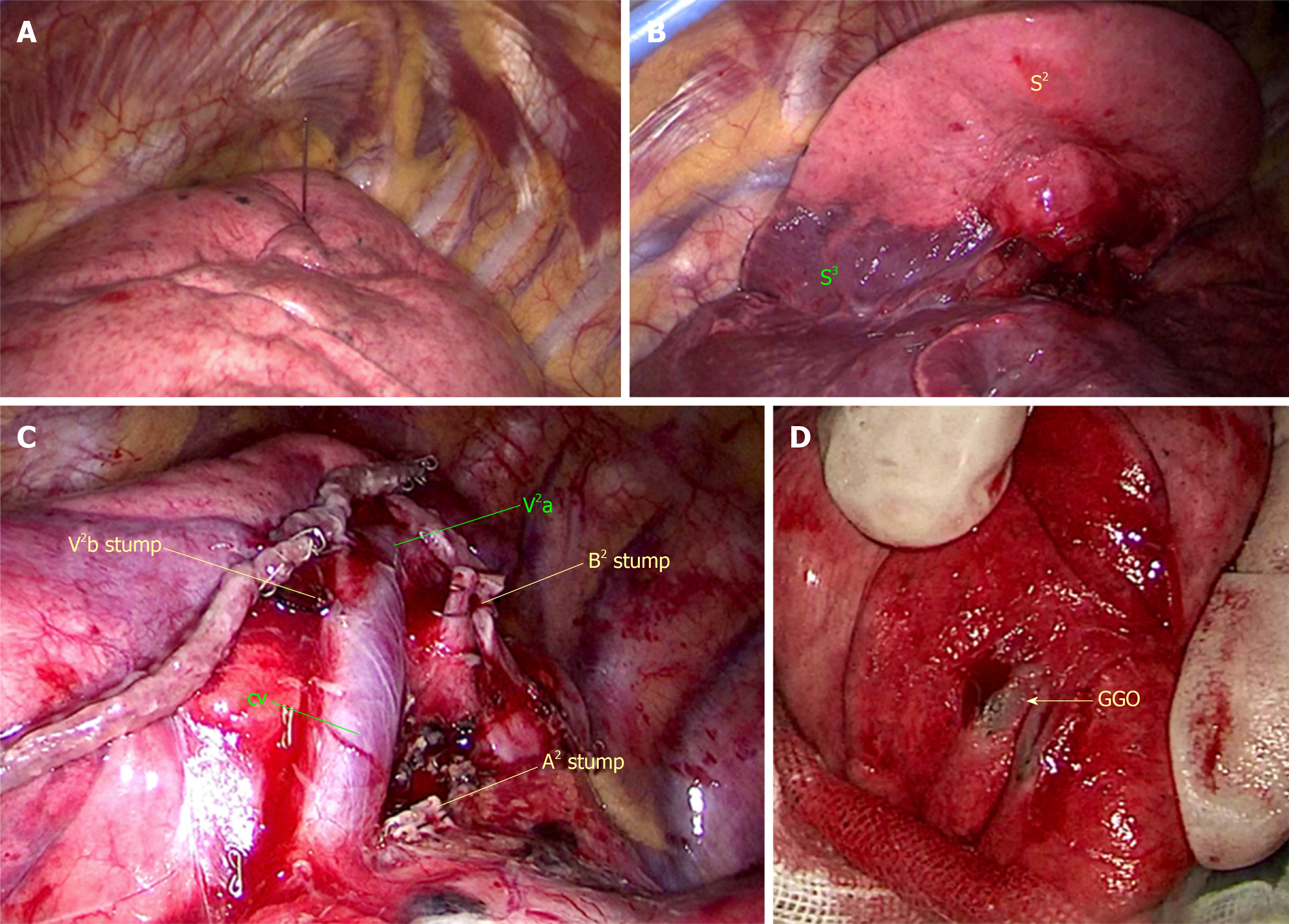
Contrast-enhanced CT of the chest and abdomen was performed using a multidetector CT (MDCT) unit (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany), which not only demonstrated an mGGO in the posterior segment of the left upper lobe (LS2) with no apparent lymph node and/or distant metastases, but also suggested a complete mirror image of the typical arrangement of the visceral organs (Figure 1). The mGGO, measuring 1.2 cm in diameter, consisted of a solid component, approximately 0.6 cm. The mGGO was located using a preoperative CT-guided hookwire (Figure 2).
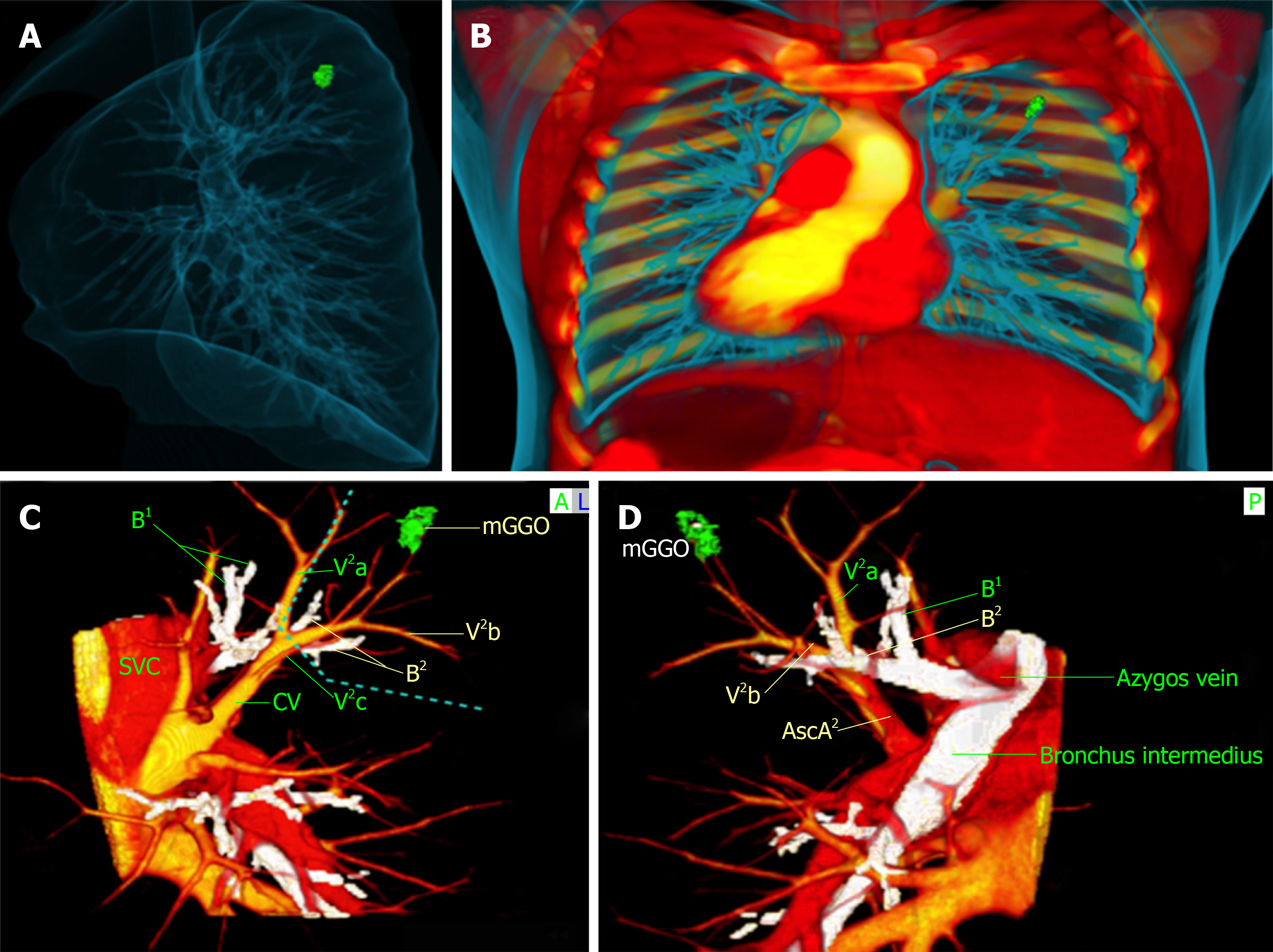
MDCT images were recorded as digital imaging and communications in medicine (DICOM) data on a server. DICOM data were obtained and saved at a slice thickness of 1.0 mm before being transmitted to a computer and reconstructed with OsiriX software installed on a Macintosh platform (Apple, Cupertino, Calif), which acted as a multi-functional workstation for preoperative planning and intraoperative navigation. The procedure for 3D-CTBA reconstruction of the targeted structure involved using a volume-rendering method, according to the CT values of air and the definition of the thoracic surgeons. The mGGO, bronchi, pulmonary arteries, and veins were separated from each other and marked out in different colors. The result of 3D-CTBA was consistent with the diagnosis of SIT and an mGGO in the LS2. We further analyzed the structure of the targeted segment, ascertained the location of the mGGO lesion, ensured the surgical margin, and finally gained a full understanding of the regional complexity (Figure 3).
The final diagnosis of the presented case was primary lung cancer and SIT.
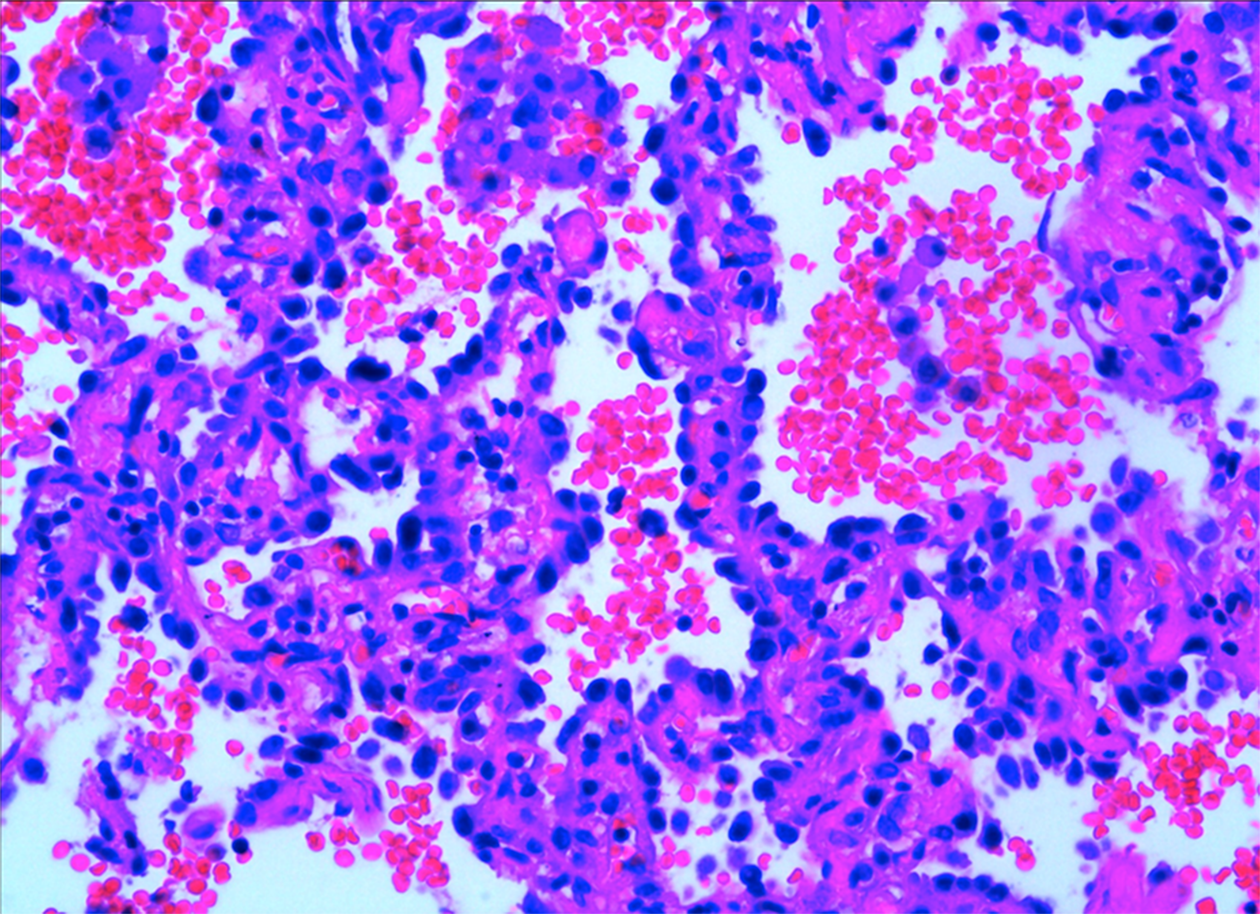
Surgery was conducted according to the preoperative 3D-CTBA and designed surgical procedure, combined with intraoperative navigation. Fast-frozen pathology indicated in situ adenocarcinoma. Based on findings from the 3D-CTBA, we performed a thoracoscopic segmentectomy of the LS2 (Figure 2). The mediastinal pleura was incised above the posterior hilum of the lung while the bronchus root of the left upper lobe was exposed. We dissected the central part of the oblique fissure to expose the interlobar artery, posterior ascending branch artery (A2), and central vein (CV). In sequence, we then cut off A2 and the posterior segmental bronchus (B2) with a stapler. Afterwards, we separated along the CV to the distal end, exposed branches V2a, V2b, and V2c, and dissociated the internal vein of the posterior segment (V2b) by ligation cutting. Finally, we defined the intersectional boundaries between S1, S3, and S2 using an improved inflation-deflation method (Figure 2B) and then removed LS2. The Nos. 11, 12, and 13 lymph nodes were sampled. Since lymph nodes were negative for pathology, a complete mediastinal lymph node dissection was omitted. The operation took one hour and 36 min, with blood loss of 50 mL. Based on results of immunostaining, including TTF-1, napsin A, p40, and p63, final pathological examination revealed in situ adenocarcinoma (Figure 4). Only regular follow-up was required after surgery; the patient did not need chemotherapy or radiotherapy.
The final pathologic stage was pTisN0M0 at stage 0 (Union for International Cancer Control, 8th edition). There were no intraoperative or postoperative complications such as air leak, pneumonia, or atelectasis, and the patient was discharged from hospital on postoperative day 5. No recurrence or mortality was observed during the follow-up period of 6 months.
The increased popularity of health checkups as well as advances in imaging techniques have resulted in a rise of early detection rate of lung cancer and have elicited multiple questions concerning appropriate treatment for these patients[8-10]. Thoracoscopic segmentectomy for early lung cancer can maximally retain healthy lung tissue, which is beneficial for protecting postoperative lung function, improving quality of life, and reducing complications[9-10]. Since the anatomical structure of the segment is relatively complex, it is difficult to pinpoint pulmonary nodules, detect anatomical variations, identify surgical margins, and protect intersegmental veins[11-12]. As a result, it is necessary to perform thoracoscopic segmentectomy assisted by 3D-CTBA[13]. In this case, the position of the mGGO was in the left S2, close to the segmental blood vessels. Careful identification in accordance with 3D-CTBA was used to clarify the location of the GGO lesion as well as its relationship to the surrounding blood vessels and bronchi, and so avoid any accidental damage.
Notably, the thoracoscopic segmentectomy of the present patient brought more challenges to surgeon owing to the transposition of the thoracic and abdominal organs to the opposite side of the body, known as SIT[1-2]. When compared to typical individuals, the anatomical structure in patients with SIT tends to be more complex and prone to anatomical variation, meaning that the risk and difficulty of surgical resection are increased. To the best of our knowledge, there are few reports of surgical resection for primary lung cancer in patients with SIT, due to its extremely low incidence[14-15].
Regarding this surgical procedure in patients with SIT and lung cancer, while previous reports have presented cases of pneumonectomy or lobectomy[16-17], we could only find two cases of thoracoscopic segmentectomy in our literature review. Wójcik et al[18] retrospectively reviewed 21 cases of lung cancer in patients with SIT which had been published worldwide since 1952, when the first case was described. Surgical treatment was performed through thoracotomy in ten cases and by VATS-assisted surgery only in two cases. The majority of the study group was male (20/21), and squamous cell carcinoma was the most frequent pathological type (8/21). The patient in our study is female, with adenocarcinoma treated by thoracoscopic segmentectomy. Matsui et al[19] reported a case of thoracoscopic segmentectomy for double primary lung cancers in a patient with SIT. However, 3D-CTBA was unavailable as a result of the patient’s renal dysfunction.
It is the first time we have performed thoracoscopic segmentectomy for a patient with lung cancer and SIT, with no adequate experience but a successful result. In rare cases, the selection of optimal surgical procedure as well as utilization of prior image training to simulate operation with 3D-CTBA will be beneficial to ensure surgical safety.
Video-assisted thoracoscopic segmentectomy to treat lung cancer can be performed safely in patients living with SIT. The assistance of 3D-CTBA facilitates surgical procedures and leads to more accurate manipulation as well as precise segmentectomy for early lung cancer, which is both effective and safe.
This research was supported by Dr Chen of Jiangsu Province Hospital. We thank him for his helpful support in operational skills.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aribas BK, El-Razek AA S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Li X
| 1. | Liu CC, Huang YC, Yeh PH. Three-dimensional printing technology: An aid for preoperative airway evaluation in patient with situs inversus totalis. J Clin Anesth. 2019;54:55-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Abdel Razek AA, Denewer AT, Hegazy MA, Hafez MT. Role of computed tomography angiography in the diagnosis of vascular stenosis in head and neck microvascular free flap reconstruction. Int J Oral Maxillofac Surg. 2014;43:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Elmokadem AH, Ibrahim EA, Gouda WA, Razek AA. Whole-Body Computed Tomography Using Low-Dose Biphasic Injection Protocol With Adaptive Statistical Iterative Reconstruction V: Assessment of Dose Reduction and Image Quality in Trauma Patients. J Comput Assist Tomogr. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Razek AA, Ezzat A, Azmy E, Tharwat N. Role of whole-body 64-slice multidetector computed tomography in treatment planning for multiple myeloma. Radiol Med. 2013;118:799-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Yao F, Wang J, Yao J, Hang F, Lei X, Cao Y. Three-dimensional image reconstruction with free open-source OsiriX software in video-assisted thoracoscopic lobectomy and segmentectomy. Int J Surg. 2017;39:16-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Xue L, Fan H, Shi W, Ge D, Zhang Y, Wang Q, Yuan Y. Preoperative 3-dimensional computed tomography lung simulation before video-assisted thoracoscopic anatomic segmentectomy for ground glass opacity in lung. J Thorac Dis. 2018;10:6598-6605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 31] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Iwano S, Yokoi K, Taniguchi T, Kawaguchi K, Fukui T, Naganawa S. Planning of segmentectomy using three-dimensional computed tomography angiography with a virtual safety margin: technique and initial experience. Lung Cancer. 2013;81:410-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Yang SC, Lai WW, Lin CC, Su WC, Ku LJ, Hwang JS, Wang JD. Cost-effectiveness of implementing computed tomography screening for lung cancer in Taiwan. Lung Cancer. 2017;108:183-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 9. | D'Andrilli A, Rendina EA. POINT: Should Segmentectomy Rather Than Lobectomy Be the Operation of Choice for Early-Stage Non-small Cell Lung Cancer? Yes. Chest. 2018;153:590-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Ghaly G, Kamel M, Nasar A, Paul S, Lee PC, Port JL, Stiles BM, Altorki NK. Video-Assisted Thoracoscopic Surgery Is a Safe and Effective Alternative to Thoracotomy for Anatomical Segmentectomy in Patients With Clinical Stage I Non-Small Cell Lung Cancer. Ann Thorac Surg. 2016;101:465-72; discussion 472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 11. | Gossot D, Lutz JA, Grigoroiu M, Brian E, Seguin-Givelet A. Unplanned Procedures During Thoracoscopic Segmentectomies. Ann Thorac Surg. 2017;104:1710-1717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Roman M, Labbouz S, Valtzoglou V, Ciesla A, Hawari M, Addae-Boateng E, Thorpe JA, Duffy JP, Majewski A. Lobectomy vs. segmentectomy. A propensity score matched comparison of outcomes. Eur J Surg Oncol. 2019;45:845-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Wu WB, Xu XF, Wen W, Xu J, Zhu Q, Pan XL, Xia Y, Chen L. Three-dimensional computed tomography bronchography and angiography in the preoperative evaluation of thoracoscopic segmentectomy and subsegmentectomy. J Thorac Dis. 2016;8:S710-S715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 52] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Shimizu J, Arano Y, Adachi I, Morishita M, Fuwa B, Saitoh M, Minato H. Adenosquamous carcinoma of the lung in a patient with complete situs inversus. Ann Thorac Cardiovasc Surg. 2011;17:178-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Divisi D, De Vico A, Ferrari V, Crisci R. Management of lung cancer in a situs viscerum inversus patient. Eur J Cardiothorac Surg. 2014;45:197-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Ye M, Shen J, Kong M, Lin J, Li X, Chen B. Video-assisted thoracoscopic surgery right upper lobectomy in a situs inversus totalis patient. J Thorac Dis. 2017;9:E1018-E1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Yoshida M, Hino H, Machida H, Hatakeyama N, Okano Y, Iwahara Y, Shinohara T, Oogushi F. Video-assisted thoracic surgery lobectomy for lung cancer in a patient with complete situs inversus. Gen Thorac Cardiovasc Surg. 2013;61:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Wójcik J, Grodzki T, Bielewicz M, Wojtyś M, Kubisa B, Pieróg J, Wójcik N. Lung cancer in situs inversus totalis (SIT)--literature review. Adv Med Sci. 2013;58:1-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Matsui T, Mizuno K, Yamada T. Video-assisted thoracoscopic bisegmentectomies for double primary lung cancers in a patient with situs inversus totalis. Gen Thorac Cardiovasc Surg. 2018;66:671-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |