Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3838
Peer-review started: August 1, 2019
First decision: September 9, 2019
Revised: September 30, 2019
Accepted: October 5, 2019
Article in press: October 5, 2019
Published online: November 26, 2019
Processing time: 116 Days and 16.8 Hours
Adult retropharyngeal abscess (RPA) is extremely rare, and most cases reported in the literature were related to tuberculous infection. We present a case of RPA with acute airway obstruction as the main manifestation in a 66-year-old woman that was considered to be non-tubercular suppurative inflammation in the retropharyngeal space.
A 66-year-old woman complaining of chills and fever was admitted to our hospital. She was initially diagnosed with an acute upper respiratory tract infection. She lost consciousness twice during hospitalization. She regained consciousness immediately upon emergency tracheal intubation. Acute upper airway obstruction was suspected as arterial blood gas analysis showed obvious acute retention of carbon dioxide before the second tracheal intubation. The diagnosis of RPA was confirmed by computed tomography and magnetic resonance imaging. Kocuria kristinae was isolated from blood samples taken from both hands. The patient recovered and was subsequently discharged after receiving antibiotic therapy together with surgical incision and drainage of the abscess.
Clinicians should be alert to the possibility of RPA in patients with acute airway obstruction. Surgical incision and drainage is an effective treatment for RPA.
Core tip: Adult retropharyngeal abscess is extremely rare as degeneration of the lymph nodes in the retropharyngeal space occurs after the age of 5 years, and most adult retropharyngeal abscesses are related to cervical spine tuberculosis. In this case report, the patient was considered to have acute non-tubercular suppurative inflammation in the retropharyngeal space. The clinical course of the patient was not straightforward, in that the initial manifestation was acute upper airway obstruction and the diagnosis of retropharyngeal abscess was only confirmed after two tracheal intubations when relevant examinations were performed.
- Citation: Lin J, Wu XM, Feng JX, Chen MF. Retropharyngeal abscess presenting as acute airway obstruction in a 66-year-old woman: A case report. World J Clin Cases 2019; 7(22): 3838-3843
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3838.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3838
Retropharyngeal abscess (RPA) involves suppurative inflammation of the retropharyngeal space, and mostly refers to acute suppurative lymphadenitis. RPA is most common in infants and children younger than 5 years and is associated with acute upper respiratory tract infection or lymphadenitis[1]. Adult RPA is very rare as the lymph nodes in the retropharyngeal space gradually degenerate after the age of 5 years. RPA may lead to complications such as acute airway obstruction, jugular necrotizing fasciitis, mediastinitis, aspiration pneumonia, thrombosis of the jugular vein, carotid artery erosion, and sepsis when diagnosis and treatment of the disease are delayed or the disease progresses, and some severe cases are life-threatening[1-3]. Herein, we present a case of RPA with acute airway obstruction as the main manifestation in a 66-year-old woman. The patient recovered and was subsequently discharged after undergoing tracheal intubation twice and treatment with surgical incision and drainage of the abscess.
A 66 year-old woman was admitted to our hospital due to chills and fever on September 4, 2013.
Two days prior to admission, she developed chills and fever (maximum temperature 39.5 °C) accompanied by pharynx pain, chest tightness, and headache. She had no cough, sputum, wheezing, dysphagia, hoarseness, weight loss, or edema of lower extremities. The patient was initially diagnosed with acute upper respiratory tract infection on admission.
The patient had a history of type 2 diabetes mellitus for 4 years and denied a history of respiratory disease, trauma, or foreign-body ingestion.
The patient was well built and nourished. Her temperature was 39.1 °C, pulse rate was 125 beats per min, respiratory rate was 24 breaths/min, and blood pressure was 110/68 mmHg. She had no clubbing, icterus, or generalized lymphadenopathy. Clinical examinations of the respiratory, cardiovascular, gastrointestinal, and nervous systems were normal.
Routine laboratory examinations revealed a leukocyte count of 9900/μL with segmented neutrophils (88%), an elevated erythrocyte sedimentation rate (79 mm/h), and increased C-reactive protein (42.9 mg/dL, reference range ˂ 0.8 mg/dL).
Computed tomography (CT) of the lung, magnetic resonance imaging (MRI) of the brain, and an ultrasonic study of the heart and liver were normal.
On the 1st day, treatment with intravenous amoxicillin, levofloxacin, and ribavirin was initiated. On the 2nd day, the patient’s body temperature remained at 39.0 °C, and the preliminary result of blood culture was gram-positive cocci; therefore, the antibiotics were changed to teicoplanin and moxifloxacin. On the 5th day, the patient’s body temperature lowered, but dyspnea was suddenly worsened. The patient then went into respiratory and cardiac arrest, lost consciousness, and developed systemic cyanosis. Arterial blood gas analysis showed that arterial partial pressure of carbon dioxide was 52 mmHg, arterial partial pressure of oxygen was 57 mmHg, and pH was 7.35. The patient received cardiopulmonary resuscitation, intravenous epinephrine, and emergency tracheal intubation, and a simple breathing bag was used. She gradually regained consciousness and restored spontaneous rhythm. The patient was transferred to the Respiratory Intensive Care Unit. Penicillin-sensitive Kocuria kristinae was isolated from blood samples 5 d after the procedure (blood samples from both the left and right hand revealed the same bacterium); thus, a diagnosis of sepsis was made and intravenous antibiotic therapy was changed to vancomycin and piperacillin-tazobactam.
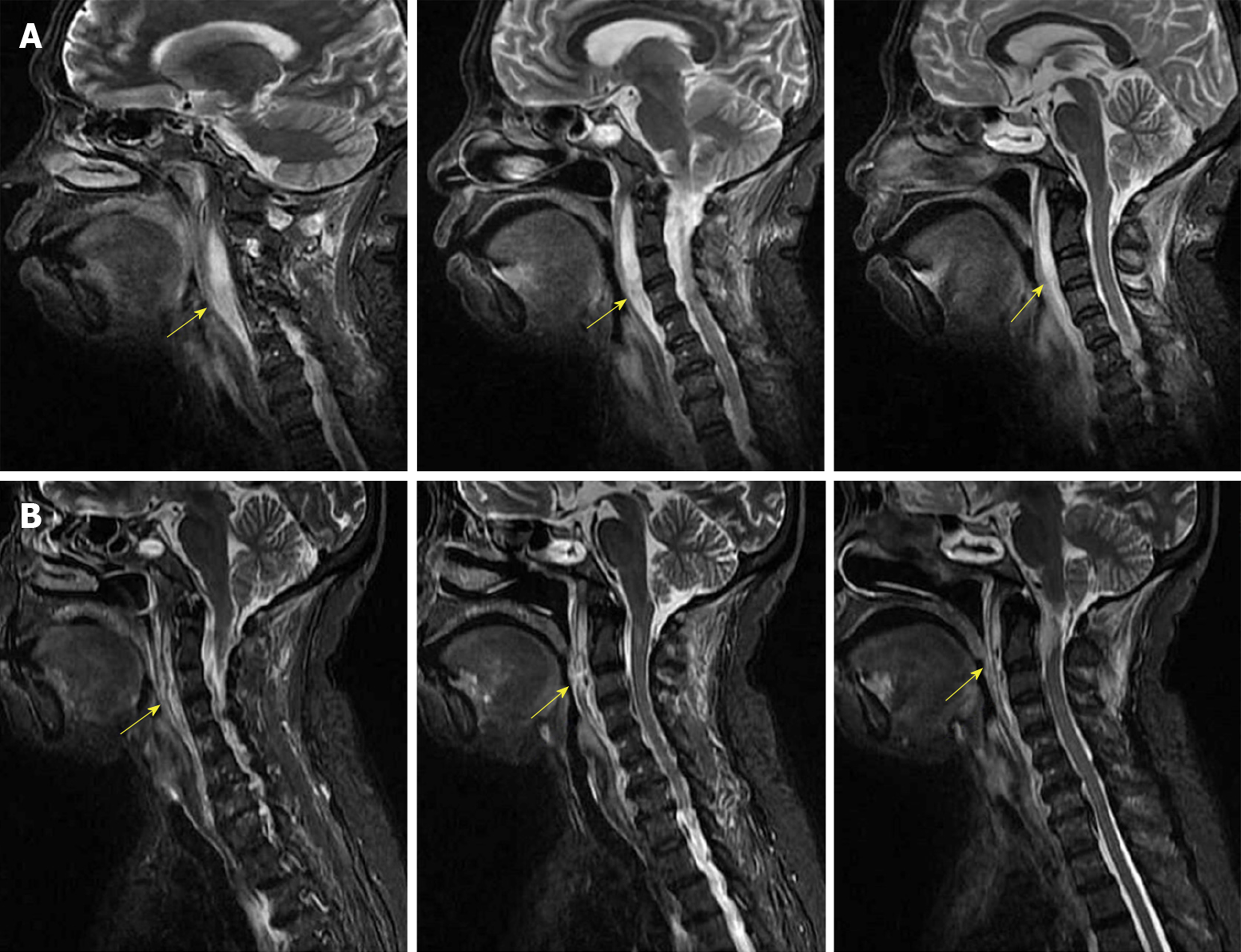
In the afternoon of the 6th day, mechanical ventilation was withdrawn and the patient was extubated as the bedside chest radiograph showed no obvious abnormalities and evaluation of arterial blood gas analysis met the weaning criteria. On the 8th day, the patient developed dyspnea again. Her heart and respiratory rates slowed, she lost consciousness again and arterial blood gas analysis showed an arterial partial pressure of carbon dioxide of 82 mmHg, arterial partial pressure of oxygen of 259 mmHg, and pH value of 7.06. She gradually regained consciousness following emergency tracheal intubation and mechanical ventilation. Acute airway obstruction was considered as arterial blood gas analysis showed obvious acute retention of carbon dioxide before the second tracheal intubation. Her symptoms rapidly improved after the second intubation, respiratory secretions were less, and a radiological examination was normal; however, the cause of a possible airway obstruction was unclear. As central nervous system diseases could not be ruled out, a lumbar puncture was performed. Analysis of cerebrospinal fluid showed a high leukocyte count (350/μL, reference range 0-8/μL) with lymphocytes (75%), no Cryptococcus, and an increased protein level (132 mg/dL, reference range 8-43 mg/dL), which indicated the possible presence of intracranial infection, but cerebrospinal fluid culture was negative. On the 9th day, a CT scan of the neck demonstrated soft tissue swelling of the nasopharyngeal and oropharyngeal wall, and occlusion of the nasopharyngeal and oropharyngeal cavity. Bedside flexible bronchoscopy was performed that revealed edema of the nasopharynx and oropharynx mucosa. MRI was performed on the 13th day that showed obvious soft tissue swelling and thickening in the anterior region of the neck, with stenosis of the nasopharynx, oropharynx, and upper airway (Figure 1A).
The diagnosis of RPA was established.
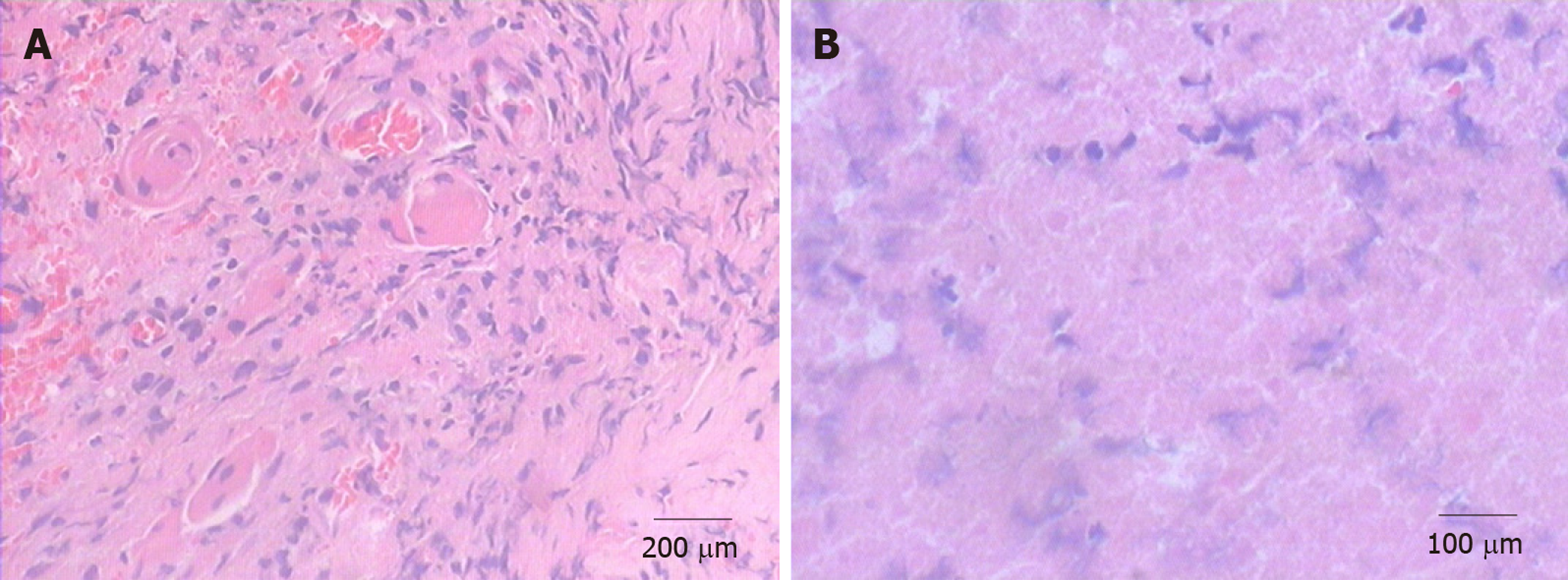
The patient underwent incision and drainage of the RPA under general anesthesia on the 14th day. Histopathology of surgical specimens showed inflammatory necrosis with granulation tissue (Figure 2), and the culture of pus was negative. MRI demonstrated stenosis of the upper airway that was alleviated after surgery (Figure 1B).
The patient had an uneventful recovery in the postoperative period and was discharged from hospital on 26 September 2013. In the 70-mo follow-up period, she was asymptomatic and had no recurrence of RPA.
The retropharyngeal space extends longitudinally downward from the base of the skull to the posterior mediastinum. Its posterior border is the prevertebral fascia, and its anterior boundary is the posterior portion of the pretracheal fascia. There is loose connective tissue and abundant lymph nodes within the retropharyngeal space during infancy. The lymph nodes are arranged in two rows at the midline of the neck and receive lymphatic drainage from the nasal cavity, paranasal sinuses, nasopharynx, and soft palate; thus, infectious diseases of the ear, nose, pharynx, and throat may spread through the lymph nodes resulting in RPA. RPA in infants is mostly associated with acute upper respiratory tract infection and generally has an acute course[1]. Adult RPA is extremely rare as degeneration of the lymph nodes in the retropharyngeal space occurs after the age of 5 years. Most adult RPAs have a chronic course and are associated with cervical spine tuberculosis that spreads through the retropharyngeal space and forms a “cold abscess”[4-5]. Due to the special anatomical location of the retropharyngeal space, an abscess can cause a series of serious complications such as jugular necrotizing fasciitis, mediastinitis, empyema, aspiration pneumonia, acute airway obstruction, or asphyxia if it spreads to the surrounding tissues[1,6]. Acute upper airway obstruction caused by RPA is rare. Hoffmann et al[2] analyzed 101 cases of retropharyngeal abscesses in children and found that only three cases had acute upper airway obstruction. In our case, the patient was an elderly woman with a dangerous clinical course that presented as acute upper airway obstruction, and her symptoms were improved after tracheal intubation, surgical drainage of the abscess, and antibiotic therapy.
“Tubercular cold abscess” was excluded as our patient was an adult with no history of oropharyngeal trauma or foreign-body ingestion. Borgohain[4] described a case of tubercular RPA caused by cervical tuberculosis in an 18-year-old Indian man who had a good prognosis after fine needle aspiration drainage of the abscess and antitubercular therapy. In our patient, we should be alert to whether RPA was caused by tuberculosis, as China is a tuberculosis prevalent country. However, this patient’s presentation did not support tuberculosis according to the following clinical data: (1) No evidence of cervical tuberculosis was found on CT images; (2) She had a series of symptoms of acute-onset systemic inflammatory response syndrome that did not meet the criteria of “tubercular cold abscess”; (3) The patient’s intracranial infection was not thought to be tubercular meningitis according to the analysis of monism as tubercular meningitis always has more severe neurological symptoms such as high fever, severe headache, positive meningeal irritation signs, and no response to general antibiotics. The patient was responsive to antibiotic treatment; (4) Biopsy findings revealed inflammatory necrosis and granulation tissue with negative acid-fast staining that did not conform to the typical tubercular granuloma with caseous necrosis and positive acid-fast staining; and (5) Acid-fast bacilli were not found in pus or sputum samples. Therefore, the patient was determined to have acute non-tubercular suppurative inflammation of the retropharyngeal space.
Staphylococcus aureus is a common pathogen of retropharyngeal abscesses[3,7]. The patient had blood cultures (from left and right hands at the same time) on admission when she had chills and fever. The culture results suggested K. kristinae, which were believed to be reliable and in line with systemic inflammatory response syndrome and sepsis. Unfortunately, pus culture of the RPA and cerebrospinal fluid culture were negative, which may have been related to the use of broad-spectrum antibiotics for several days. K. kristinae is a gram-positive coccus that is often found in the environment and on human skin. K. kristinae infections are uncommon but are increasingly being recognized, especially in immunocompromised patients[8]. The patient was in the high risk population for K. kristinae infection as she suffered from diabetes and her normal blood glucose control was unknown. Systemic sepsis leading to metastatic retropharyngeal space abscess is extremely rare. Thus, it is inferred that the patient inhaled the bacterium into her upper respiratory tract, causing the RPA, sepsis, and intracranial infection.
Endotracheal intubation, tracheotomy, fine needle aspiration drainage, or emergency surgical drainage should be performed when acute upper airway obstruction is caused by an RPA. Intubation may result in rupture of the abscess and suffocation. Borgohain[4] adopted ultrasonography-guided needle aspiration drainage together with antitubercular therapy that achieved a good effect with partial neurological recovery in a patient with a huge tubercular RPA. Compared to surgical drainage, ultrasonography-guided fine needle aspiration has many advantages such as less invasive, repeatable drainage, and local injection of drugs, but surgery has become a more appropriate choice when the abscess is large or the pus is sticky and difficult to drain. Hoffmann et al[2] recommended that conservative medical treatment should be chosen if the retropharyngeal abscess is less than 20 mm in pediatric cases, and surgical treatment should be chosen if the abscess is greater or equal to 20 mm. At times, tracheotomy is an emergency substitute for tracheal intubation in order to alleviate the airway obstruction immediately and prevent rupture of the abscess[1]. In our patient, intubation was an emergency option to relieve airway obstruction as throat CT or MRI had not been performed, and we were unaware of the RPA when acute airway obstruction occurred. Of course, the key to successful treatment in this patient was powerful antibiotic therapy and the subsequent combination of surgical incision and drainage.
The case in the present report is relatively rare for the following reasons: (1) The patient had an adult-onset acute RPA, which is rare in clinical practice; (2) The clinical course of the patient was not straightforward, in that the initial manifestation was acute upper airway obstruction, and the diagnosis of retropharyngeal abscess was only confirmed after two tracheal intubations when relevant examinations were performed; and (3) K. kristinae isolated from the patient’s blood is a relatively rare pathogen causing sepsis, and its combination with intracranial infection indicated the presence of severe systemic inflammatory response syndrome in this patient. The patient was in good condition during the 70-mo follow-up period.
We are grateful to Abigail Howard (School of Medicine, the University of Chicago) for revision of this manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Isik A S-Editor: Wang J L-Editor: Filipodia E-Editor: Liu JH
| 1. | Ozbek C, Dagli S, Tuna EE, Ciftci O, Ozdem C. Giant retropharyngeal abscess in an adult as a complication of acute tonsillitis: case report. Ear Nose Throat J. 2009;88:E20-E22. [PubMed] |
| 2. | Hoffmann C, Pierrot S, Contencin P, Morisseau-Durand MP, Manach Y, Couloigner V. Retropharyngeal infections in children. Treatment strategies and outcomes. Int J Pediatr Otorhinolaryngol. 2011;75:1099-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Hari MS, Nirvala KD. Retropharyngeal abscess presenting with upper airway obstruction. Anaesthesia. 2003;58:714-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Borgohain B. Prompt restoration of airway along with rapid neurological recovery following ultrasonography-guided needle aspiration of a tubercular retropharyngeal abscess causing airway obstruction. Singapore Med J. 2011;52:e229-e231. [PubMed] |
| 5. | Garg A, Wadhera R, Gulati SP, Kishore D, Singh J. Giant retropharyngeal abscess secondary to tubercular spondylitis. Indian J Tuberc. 2009;56:225-228. [PubMed] |
| 6. | Chen CH, Wang CJ, Lien R, Chou YH, Chang CC, Chiang MC. Mediastinal and retropharyngeal abscesses in a neonate. Pediatr Neonatol. 2011;52:172-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Shin JH, Sung SI, Kim JK, Jung JM, Kim ES, Choi SH, Kim YJ, Ahn KM, Chang YS, Park WS. Retropharyngeal abscess coinfected with Staphylococcus aureus and Mycobacterium tuberculosis after rhinoviral infection in a 1-month-old infant. Korean J Pediatr. 2013;56:86-89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Cheung CY, Cheng NH, Chau KF, Li CS. An unusual organism for CAPD-related peritonitis: Kocuria kristinae. Perit Dial Int. 2011;31:107-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |