Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3784
Peer-review started: May 27, 2019
First decision: September 9, 2019
Revised: September 30, 2019
Accepted: October 15, 2019
Article in press: October 15, 2019
Published online: November 26, 2019
Processing time: 184 Days and 3 Hours
Intravitreal injection has become an efficient approach for delivering drugs at therapeutic levels to the posterior segment in retinal diseases. However, the increased frequency and number of intravitreal injections have raised concerns about their side effects. As manipulation during surgery is relatively simple, details of the procedure are easily overlooked. Iatrogenic crystalline lens injury is a rare complication caused by improper manipulation during surgical procedures. We report two cases of crystalline lens injury during intravitreal injection of triamcinolone acetonide (TA) with the hope of providing an insight into this treatment.
Case 1 was a 62-year-old woman with macular edema caused by central retinal vein occlusion in her right eye, and Case 2 was a 65-year-old man with macular edema caused by branch retinal vein occlusion in his right eye. In view of the patients’ condition and economic constraints, an intravitreal injection of TA was administered. Due to inappropriate manipulation during surgery, the lens was injured. The site of lens injury and clinical manifestations were different in the two cases. Symptomatic treatment and continuous follow-up were carried out. The therapeutic effect following phacoemulsification of the cataract was satisfactory.
Well-defined surgical incision under proper anesthesia, sufficient patient information and proficient anatomical skills of the physician are mandatory to prevent this rare adverse event. Careful and meticulous phacoemulsification of the cataract is suggested.
Core tip: Iatrogenic crystalline lens injury is a rare complication caused by improper manipulation during surgical procedures. We report two cases of crystalline lens injury during intravitreal injection of triamcinolone acetonide. The site of lens injury and clinical manifestations were different in the two cases. Symptomatic treatment and continuous follow-up were carried out. We hope to provide an insight into this treatment.
- Citation: Su J, Zheng LJ, Liu XQ. Iatrogenic crystalline lens injury during intravitreal injection of triamcinolone acetonide: A report of two cases. World J Clin Cases 2019; 7(22): 3784-3791
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3784.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3784
Triamcinolone acetonide (TA) is a type of glucocorticoid with long-lasting effects, which can inhibit cellular immunity, reduce inflammation and maintain the permeability of blood capillaries. It can also maintain the blood-retina barrier, limit fibrin exudation and inhibit the angiogenesis growth factor to prevent the formation of new blood vessels. Based on these features, TA is administered by intravitreal injection to treat vitreoretinal diseases at a local therapeutic and sustainable concentration. Although injection of Ozurdex has become the main treatment for macular edema in recent years[1], TA injection is an effective and inexpensive treatment and is still used in developing countries or regions. Recent research has indicated that intravitreal injection of TA is an efficient approach in the treatment of a variety of proliferative, edematous, neovascular and inflammatory ocular disorders[2-4]. Despite the efficacy of intravitreal TA injection, attention should be paid to its associated complications. These complications may be caused by the injection procedure or the side-effects of the corticosteroid. Long-term complications, such as cataract development and secondary glaucoma especially in the case of repeated injection, are attributed to the side effects of the corticosteroid. Immediate complications, such as conjunctival hemorrhage, retinal pigment epithelium tears, retinal detachment, vitreous hemorrhage and endophthalmitis, are due to the injection procedure. Iatrogenic crystalline lens injury is a rare complication of intravitreal TA injection, which occurs due to contact or penetration of the lens by the needle tip. We report two cases of iatrogenic crystalline lens injury during intravitreal injection of TA.
Case 1: A 62-year-old woman with a 5 mo history of central retinal vein occlusion in the right eye complained of severe vision impairment.
Case 2: A 65-year-old man with macular edema caused by branch retinal vein occlusion in his right eye for 2 mo complained of visual deformity.
In Case 1, the patient had received retinal photocoagulation therapy and treatment with oral Chinese medicine, but her condition did not improve. In Case 2, the patient experienced worsening visual disturbance for two weeks although he had received retinal photocoagulation therapy.
Both patients had no remarkable history of illness.
Both patients had hyperopia. In Case 1, the eye axis was 22.15 mm and the spherical equivalent was 1.50 D. Her best-corrected visual acuity (BCVA) was 20/50 and the intraocular pressure (IOP) was 18 mmHg before injection. In Case 2, the eye axis was 21.68 mm and the spherical equivalent was 2.25 D. His BCVA was 20/100 and the IOP was 15 mmHg. Both patients had a shallow anterior chamber and the crystal lens was transparent on the whole under the slit lamp.
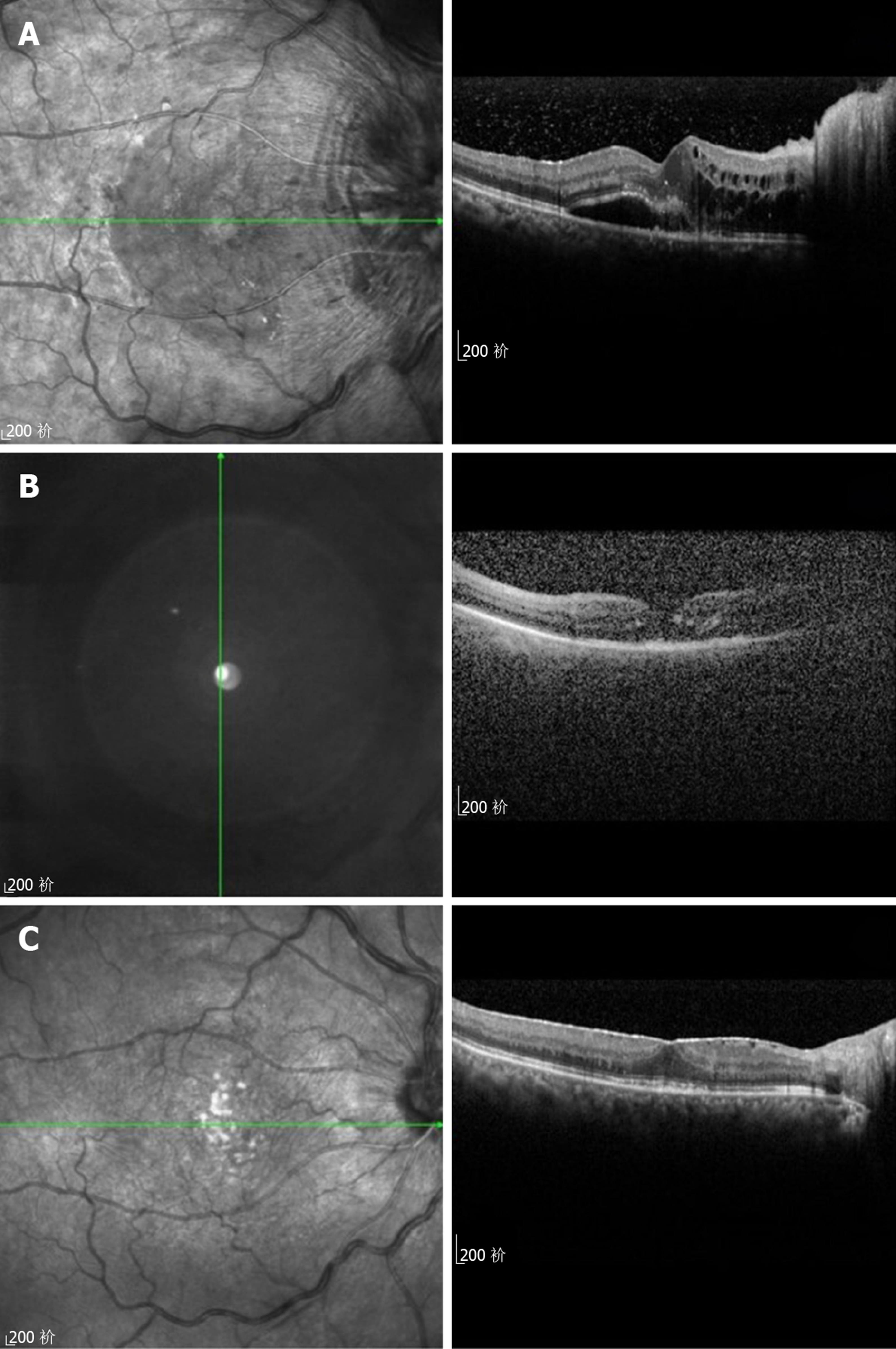
In Case 1, optical coherence tomography (OCT) revealed persistent cystoid macular and optic nerve edema (Figure 1A). In Case 2, OCT revealed cystoid macular edema and hemorrhage in the subtemporal quadrant of the retina.
Macular edema caused by retinal vein occlusion.
In China, anti-vascular therapy for macular edema secondary to retinal vein occlusion is not included in medical insurance. In view of the patients’ economic status and urgent desire for treatment, we treated the patients with intravitreal TA injection after informed consent related to treatment risk and associated complications was obtained. Briefly, 0.1 mL/4 mg TA was intravitreally injected under surface anesthesia into the superior temporal quadrant, 3.5 mm from the limbus of the cornea. All intravitreal injections were performed by the same right-handed resident.
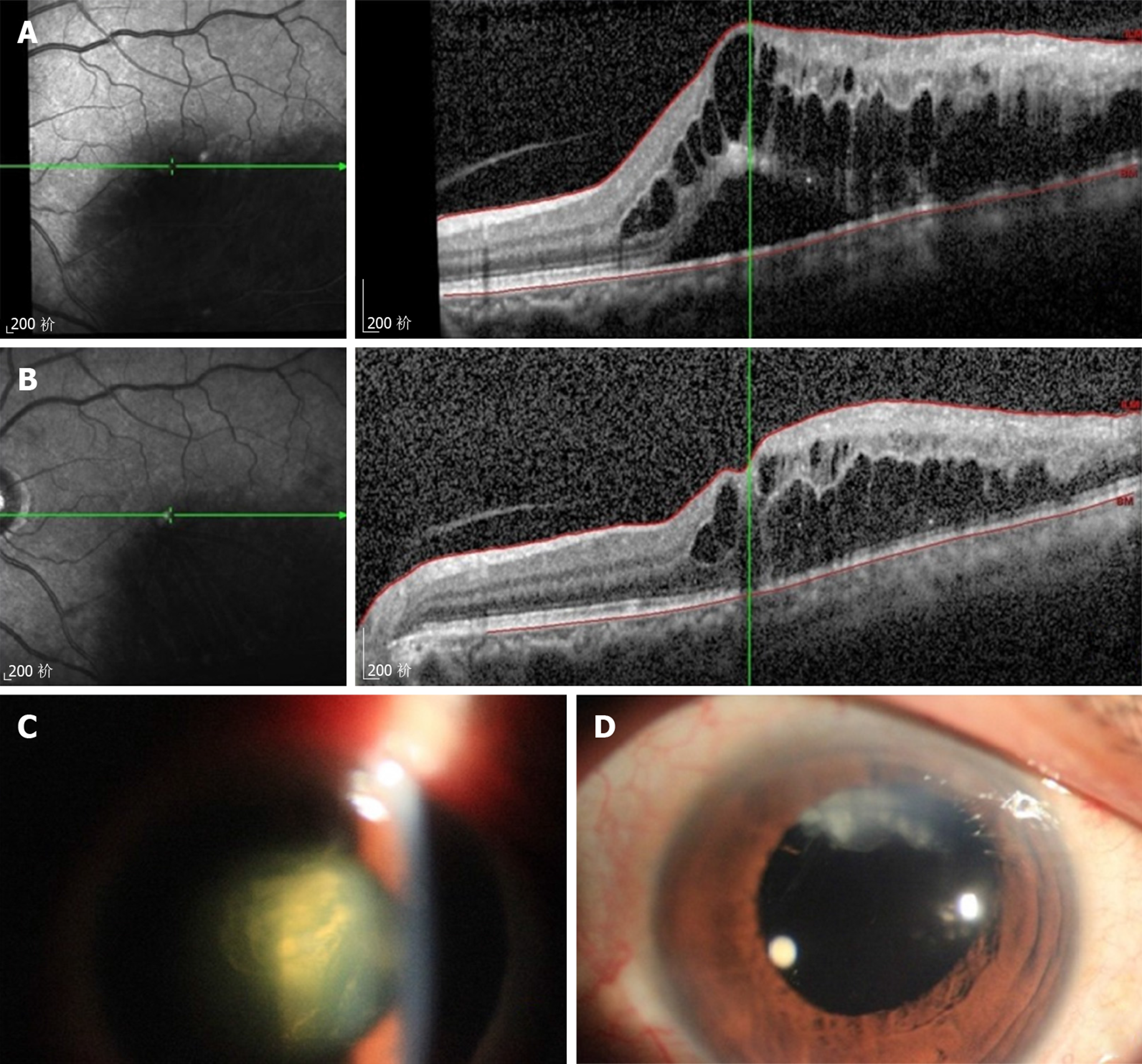
In Case 1, on the first day after TA injection, slit lamp examination showed that the suspended TA particles formed a villiform opacity behind the posterior capsule. However, the lens cortex and core remained transparent (Figure 2A). There seemed to be a visible capsular channel perforation on the posterior capsule of the lens. The patient complained of blurred vision but no other discomfort. BCVA was fingers in front of the eyes and the IOP was 19 mmHg. The fundus was not observed. Follow-up after two weeks showed that the suspended TA particles behind the posterior capsule had a tendency to be absorbed (Figure 2B). The BCVA was enhanced to 20/166 and the IOP was 20 mmHg. One month later, the TA suspension behind the posterior capsule was further absorbed and the lens cortex and core remained transparent (Figure 2C). The BCVA was 20/133 and the IOP was 21 mmHg. Fuzzy fundus was observed and macular edema was alleviated (Figure 1B). The patient was subsequently lost to follow-up as she moved to another city. Eight months after the TA injection, she visited us again. The TA in the posterior capsule was mostly absorbed, limited rice crust opacity had formed and posterior subcapsular opacification was observed. A slow progressive opacity in the lens cortex and core was found (Figure 2D). OCT examination showed that macular edema had mostly subsided, but macular epiretinal membrane had appeared (Figure 1C). BCVA was enhanced to 20/100. However, the IOP rose to 32 mmHg without inflammation of the anterior and posterior chambers. She was prescribed timolol, brimonidine and latanoprost. The IOP was controlled to 21-25 mmHg. At 9 mo after intravitreal injection of TA, cataract surgery was performed with standard phacoemulsification devices. As rupture of the posterior capsule was predicted, we prepared for anterior vitrectomy before surgery. During the operation, the anterior chamber water pressure was reduced by keeping the height of the infusion bottle low. After annular tearing of the anterior capsule, only hydrodelineation was performed to prevent rupture of the posterior capsule or enlargement of the original tear. The nucleus and cortex were easily aspirated by an irrigation-aspiration probe with a low flow parameter due to the slight cataract. Posterior capsule holes were found during the process of removing the residual cortex and polishing the posterior capsule membrane. We were not sure whether the capsular tear was caused by the cataract surgery or needle puncture in the earlier intravitreal injection. In order to prevent further enlargement of the hole, polishing and irrigation-aspiration were stopped. This resulted in some cortical residues on the peripheral cortex and the posterior capsular surface. Fortunately, due to mild liquefaction of the vitreous body, vitreous exfoliation was inconspicuous despite rupture of the posterior capsule. We did not perform anterior vitrectomy and implanted the intraocular lens (IOL) directly into the ciliary sulcus. On the second day after surgery, there was no significant residual cortex in the pupil area, which did not affect the optic axis area.
In Case 2, on the first day after TA injection, the BCVA was 20/200 and the IOP was 42 mmHg. Lens opacity and expansion was observed under the slit lamp (Figure 3C). The image was blurred due to corneal edema. The IOP could not be controlled by anti-glaucoma medications in the following weeks. One week after injection, the patient underwent cataract surgery. The detailed procedure was the same as that in Case 1. The nucleus and cortex were removed by irrigation-aspiration using low flow parameters. A posterior capsule tear secondary to the injection was observed. Anterior vitrectomy was not performed as there was no obvious vitreous overflow. The IOL was then placed in the sulcus.
In Case 1, one week after surgery, the posterior capsule had partial opacity in the upper quadrant of the nose, but no opacity in the pupil area (Figure 2E). The patient’s BCVA increased to 20/33 and IOP was 15 mmHg without anti-glaucoma medications. Despite her improved eyesight, the patient still complained of sight deformation.
In Case 2, four weeks after surgery, BCVA was 20/50, and IOP was 16 mmHg without anti-glaucoma medications. Remnants of the lens cortex were found in the temporal quadrant (Figure 3D). Although not all the drugs were injected into the vitreous cavity, the macular edema partially subsided (Figure 3B).
Regular follow-up visits were performed in both cases and no further complications were found. Both patients were satisfied with the final outcome and visual acuity.
Iatrogenic crystalline lens injury due to needle tip contact or penetration is rare, with a reported incidence of 0.006%[5]. Only 4 cases have been reported. These four cases were all caused by intravitreal injection of dexamethasone into the crystalline lens[6-8]. In recent years, with the increase in Ozurdex injections, cases of iatrogenic lens injury have increased[9-11]. Due to the special suspending property of TA, the complication caused by TA implanted into the crystalline lens is unique. In our cases, the crystalline lens was injured, but cataract progression was not observed over the entire follow-up period. It was presumed that a small lens wound could heal spontaneously due to proliferation of the subcapsular epithelium which would seal the wound before the intraventricular passage of ions and fluid, leading to cataract progression[12]. The cataract remained stable in the superior-temporal quadrant without progress in Case 2. However, since we only monitored the patient for one week, a conclusion could not be drawn. As TA is composed of white suspended particles, feather-like turbidity formed, blocking the line of sight in Case 1 without cataract formation when TA was injected into the posterior capsule of the lens. Although not all TA injected into the posterior capsule of the lens was distributed in the vitreous cavity, it still played a role in the treatment of macular edema in Case 1. Although macular edema subsided, formation of the macular epiretinal membrane is rare. The reason for this requires further investigation.
In Case 1, the increase in IOP may be related to suspended TA particles which clogged the trabecular meshwork, which in turn was due to degeneration of the trabecular meshwork caused by steroid hormones. In Case 2, the increase in IOP was related to expansion of the lens caused by drug injection into the crystalline body. The experiences drawn from these two cases are as follows:
The site and the angle of the injection needle are important and are the main cause of lens injury. The needle used in intravitreal injection should puncture the pars plana corporis ciliaris, which is generally 3.5 mm-4 mm posterior to the limbus. In our two cases, we chose 3.5 mm using a caliper to measure from the limbus. We ignored the ocular axial length change in these cases. In Case 1, the eye axis was 22.15 mm, and in Case 2, the eye axis was 21.68 mm. Both cases had mild hyperopia with a short axial length. If the needle entry was performed according to the conventional 3.5 mm posterior to the limbus in short axial eyes, it would result in injection close to the ciliary body. On the one hand, injection close to the ciliary body would narrow the needle’s movable range and the needle could easily touch the lens. On the other hand, it might stimulate the ciliary body to cause pain, which will cause sudden movement of the operated eye, increase the difficulty of the operation and the risk of injury to adjacent structures. Therefore, the puncture site for intravitreal injection should be 4 mm posterior to the limbus, especially in hyperopia eyes.
The insert angle of the needle should be oblique toward the center of the optic nerve. It has been demonstrated that the angle between the posterior capsule of the crystalline lens and the retinal surface is 90°[5]. During surgery, in order to facilitate manipulation in the superior temporal quadrant, we asked the patient to look at his inferonasal quadrant during the operation. In such a position, the needling should be done perpendicular to the eyeball. If the needle is still at a fairly steep angle of less than 45°, it is more likely to damage the lens. Thus, the needle should be moved toward the optic nerve with a 90° angle after piercing the sclera.
We used surface anesthesia with alcaine eye drops. For some sensitive patients, this method is insufficient. Pain or tension during the operation may cause the patient to move their head or eyeball suddenly and results in lens injury. It is noteworthy that we used cotton swabs to displace the loose conjunctiva during the operation, and this may have led to a shift in the injection site location.
The recommended diameter of the needle is gauge 27 to reduce the risk of injury to ocular structures and wound leakage. In our procedure, we used 26 gauge needles. The thicker the needle, the greater the contact with the sclera, and greater strength for the injection is needed[13]. This caused movement of the eyeball due to local pain, and greater pressure resulted in a shorter distance between the needle and the lens.
Although intravitreal injection is a simple technique, it still requires a learning curve especially for young residents. Accurate selection of needle entry points and angles, appropriate anesthesia, stable head fixation, small-size injection needles and a comprehensive understanding of the patient’s condition before surgery are important to avoid complications. A careful preoperative evaluation and well-prepared cataract surgery can alleviate anatomical and functional damage.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Meyer CH S-Editor: Zhang L L-Editor: Webster JR E-Editor: Liu JH
| 1. | Schmitz K, Maier M, Clemens CR, Höhn F, Wachtlin J, Lehmann F, Bertelmann T, Rüdiger K, Horn M, Bezatis A, Spital G, Meyer CH; German Retinal Vein Occlusion Group. Zuverlässigkeit und Sicherheit von intravitrealen Ozurdex-Injektionen. Ophthalmologe. 2014;111:44-52. [RCA] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Noma H, Funatsu H, Mimura T, Shimada K. Macular sensitivity and morphology after intravitreal injection of triamcinolone acetonide for macular edema with branch retinal vein occlusion. Retina. 2012;32:1844-1852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Campochiaro PA, Wykoff CC, Brown DM, Boyer DS, Barakat M, Taraborelli D, Noronha G; Tanzanite Study Group. Suprachoroidal Triamcinolone Acetonide for Retinal Vein Occlusion: Results of the Tanzanite Study. Ophthalmol Retina. 2018;2:320-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 4. | Ghoraba HH, Leila M, Elgouhary SM, Elgemai EEM, Abdelfattah HM, Ghoraba HH, Heikal MA. Safety of high-dose intravitreal triamcinolone acetonide as low-cost alternative to anti-vascular endothelial growth factor agents in lower-middle-income countries. Clin Ophthalmol. 2018;12:2383-2391. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Meyer CH, Rodrigues EB, Michels S, Mennel S, Schmidt JC, Helb HM, Hager A, Martinazzo M, Farah ME. Incidence of damage to the crystalline lens during intravitreal injections. J Ocul Pharmacol Ther. 2010;26:491-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 6. | Taright N, Guedira G, Morfeq H, Drimbea A, Milazzo S. Prevention of accidental injection of dexamethasone intravitreal implant into the crystalline lens. J Fr Ophtalmol. 2016;39:e211-e212. |
| 7. | Abdolrahimzadeh S, Parisi F, Abdolrahimzadeh B, Cruciani F. Unusual choroidal vessels in neurofibromatosis type 1 observed with near-infrared reflectance and spectral domain optical coherence tomography. Acta Ophthalmol. 2016;94:e815-e816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Berarducci A, Sian IS, Ling R. Inadvertent dexamethasone implant injection into the lens body management. Eur J Ophthalmol. 2014;24:620-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Koller S, Neuhann T, Neuhann I. Conspicuous crystalline lens foreign body after intravitreal injection. Ophthalmologe. 2012;109:1119-1121. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Kurt A, Durukan AH, Küçükevcilioğlu M. Accidental Intralenticular Injection of Ozurdex® for Branch Retinal Vein Occlusion: Intact Posterior Capsule and Resolution of Macular Edema. Case Rep Ophthalmol Med. 2019;2019. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Baskan B, Cıcek A, Gulhan A, Gundogan M, Goktas S. Ozurdex completely located inside a crystallized lens - Results of 14 months. Am J Ophthalmol Case Rep. 2016;4:38-40. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Fagerholm PP, Philipson BT. Human traumatic cataract. A quantitative microradiographic and electron microscopic study. Acta Ophthalmol (Copenh). 1979;57:20-32. [PubMed] |
| 13. | Kozak I, Dean A, Clark TM, Falkenstein I, Freeman WR. Prefilled syringe needles versus standard removable needles for intravitreous injection. Retina. 2006;26:679-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |