Published online Nov 26, 2019. doi: 10.12998/wjcc.v7.i22.3765
Peer-review started: September 18, 2019
First decision: October 24, 2019
Revised: October 29, 2019
Accepted: November 15, 2019
Article in press: November 15, 2019
Published online: November 26, 2019
Processing time: 68 Days and 21 Hours
Intestinal lipomas are rare benign gastrointestinal (GI) tumors, usually asymptomatic, but may become symptomatic as the result of some complications such as intussusception, intestinal obstruction, volvulus or bleeding. They can occur at any site along the entire GI tract, more frequent in colon and rarely in small intestine. The patient reported here is a very rare case of jejunal lipoma, ulcerated and intussuscepted, diagnosed in an adult investigated for a chronic iron deficiency anemia (IDA), and successfully managed by segmental jejunal resection.
A 63-year-old male was referred to “St. Spiridon” Hospital, Institute of Gastroenterology and Hepatology, Iasi, to investigate an obscure GI bleeding with an IDA. After upper GI endoscopy and colonoscopy were performed, excluding potentially bleeding lesions, videocapsule endoscopy was then carried out, revealing fresh blood and a protruding lesion in proximal jejunum, findings confirmed by a single-balloon enteroscopy. Multiple biopsies were taken from the lesion, but histological results were inconclusive. Then, contrast - enhanced computed tomography was performed showing jejunal polypoid mass with homogenous fat density, suggestive for lipoma. A week later a laparotomy was performed revealing the intussuscepted jejunal segment which was resected en bloc, and sent for further histopathologic analysis. The patient made an uneventful recovery and was discharged seven days later, and at six months follow-up he had no complains and his hemoglobin returned to normal value.
Lipomas are very rarely located in the jejunum, usually asymptomatic, but they may lead to complications such as intussusception and bleeding. Surgical resection remains the treatment of choice.
Core tip: Jejunal lipomas are very rare benign tumors in adults, usually asymptomatic, and found incidentally during investigation for other abdominal pathologies or when cases present a complication such as intussusception, intestinal obstruction or bleeding. Here we present a case of jejunal lipoma complicated by ulceration, intussusception, and gastrointestinal bleeding, successfully managed by segmental resection. Location of lipoma in jejunum is exceptional with only 10 cases reported in the literature with similar location and complications as our case.
- Citation: Cuciureanu T, Huiban L, Chiriac S, Singeap AM, Danciu M, Mihai F, Stanciu C, Trifan A, Vlad N. Ulcerated intussuscepted jejunal lipoma-uncommon cause of obscure gastrointestinal bleeding: A case report. World J Clin Cases 2019; 7(22): 3765-3771
- URL: https://www.wjgnet.com/2307-8960/full/v7/i22/3765.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i22.3765
Lipomas are benign, fatty gastrointestinal (GI) tumors, more commonly located in the colon (64%)[1], the small intestine being the second site, and very rarely in the jejunum (< 2%)[2]. Usually, small bowel lipomas are asymptomatic, uncomplicated and discovered incidentally during investigation for other abdominal diseases such as an obstructive bowel syndrome or GI bleeding[2,3]. However, they may become symptomatic as the result of a number of complications such as bleeding, intussusception, and obstruction. The intussusception is defined as the telescoping of a proximal segment of bowel into the lumen of an adjacent segment of bowel (usually resulting in obstruction), and it is more common in children, where is generally idiopathic; it seldom occurs in adults (with 5% of all cases of intussusception)[3] and it is often due to a malignancy (70% of the colonic and 30% of small bowel intussusceptions are attributable to malignancy)[4]. In a retrospective study including all adult patients diagnosed with intussusception at Mayo Clinic, Rochester from 1983 to 2008, among all 196 patients, only 10 presented with small bowel lipomas[5]. We report a very rare case of an ulcerated intussuscepted jejunal lipoma in an adult, discovered after investigating an obscure GI bleeding and managed by surgical resection. We also made a short review of the literature regarding the small bowel (jejunal) intussuscepted lipoma.
A 63-year-old man with personal history of hypertension was admitted to our department of Gastroenterology and Hepatology to investigate an obscure GI bleeding with iron deficiency anemia (IDA).
He complained of intermittent abdominal pain accompanied by nausea.
He had a prior history of hypertension well controlled by treatment with angiotensin-converting enzyme inhibitors. He had no abdominal surgery.
He was a construct engineer and a current smoker (15 cigarettes/d for the past 20 years). He had no serious family history.
Physical examination showed pale teguments, and the abdomen was soft and tender in the umbilical and right flank area, without any palpable abdominal mases.
Laboratory data showed IDA (hemoglobin 9.5 g/dL, serum iron 45 µg/dL, ferritin 10 µg/L).
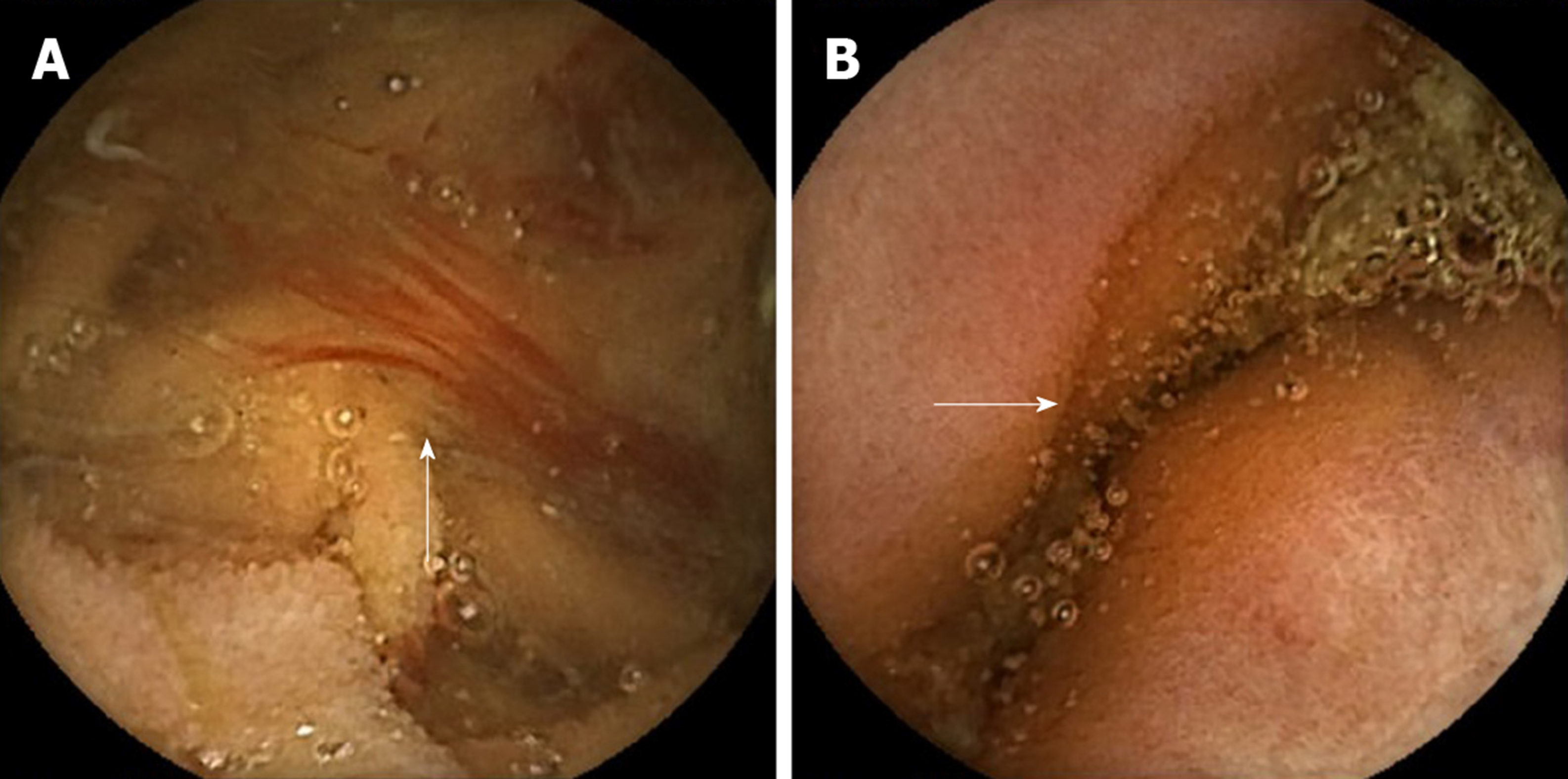
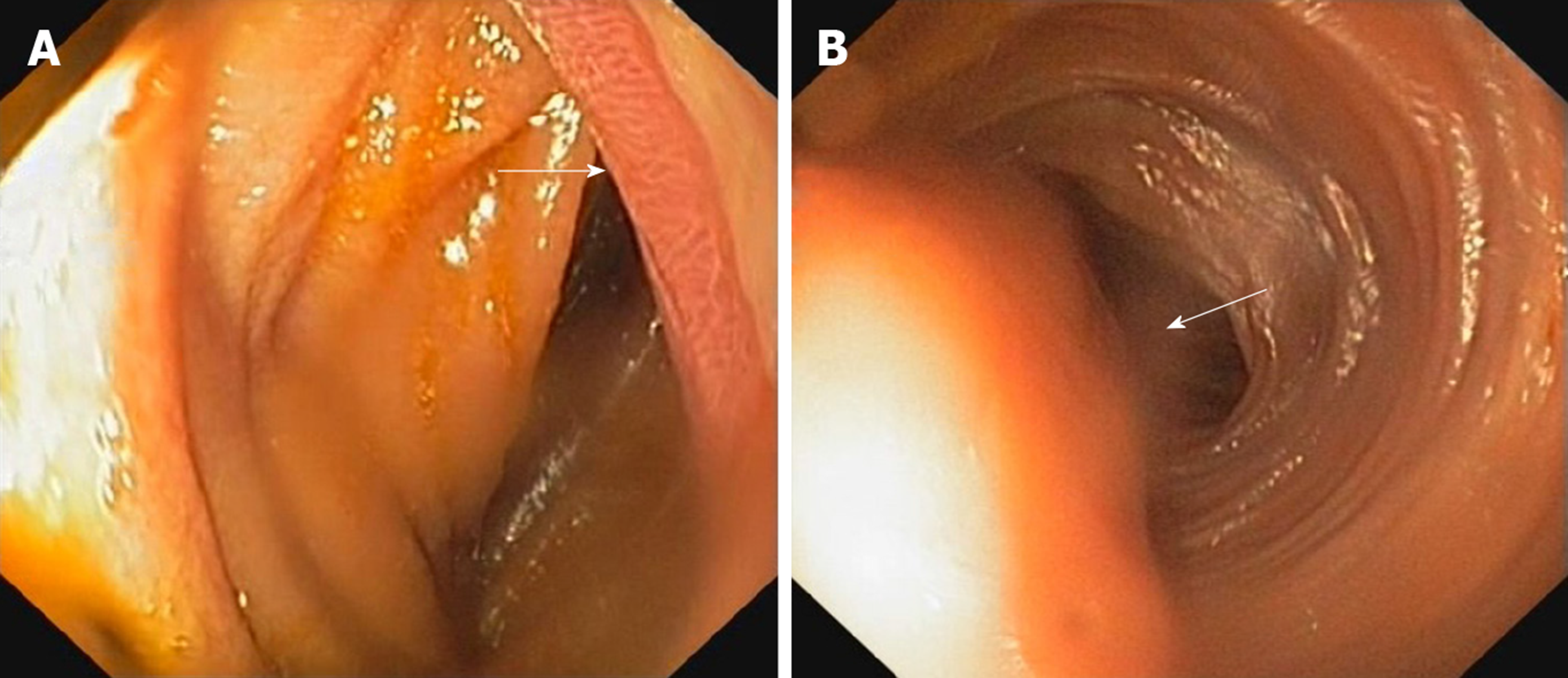
An upper GI endoscopy and colonoscopy were performed, excluding lesions with potential for bleeding. Then, videocapsule endoscopy was performed, revealing fresh blood in the proximal jejunum, and a protruding lesion, with discolored covering mucosa (Figure 1A and B). Next, a single–balloon enteroscopy was carried out, which showed a polypoid mass with ulceration, situated in the proximal segment of jejunum (Figure 2A and B). Multiple biopsies were taken from the lesion, but the histological result was inconclusive, as it frequently occurs in submucosal GI benign tumors including lipomas, due to depth factor–the amount of submucosal tissue required in biopsies of the lesion. Then, contrast-enhanced abdominal computed tomography was performed which showed a 6 centimeters elongated structure inside the intestinal lumen with homogenous fat density and smooth well-defined contour, suggestive for an intestinal lipoma (Figure 3). Within the next week the patient complained of abdominal pain, nausea and several episodes of vomiting. A laparotomy was performed revealing jejuno-jejunal intussusception.
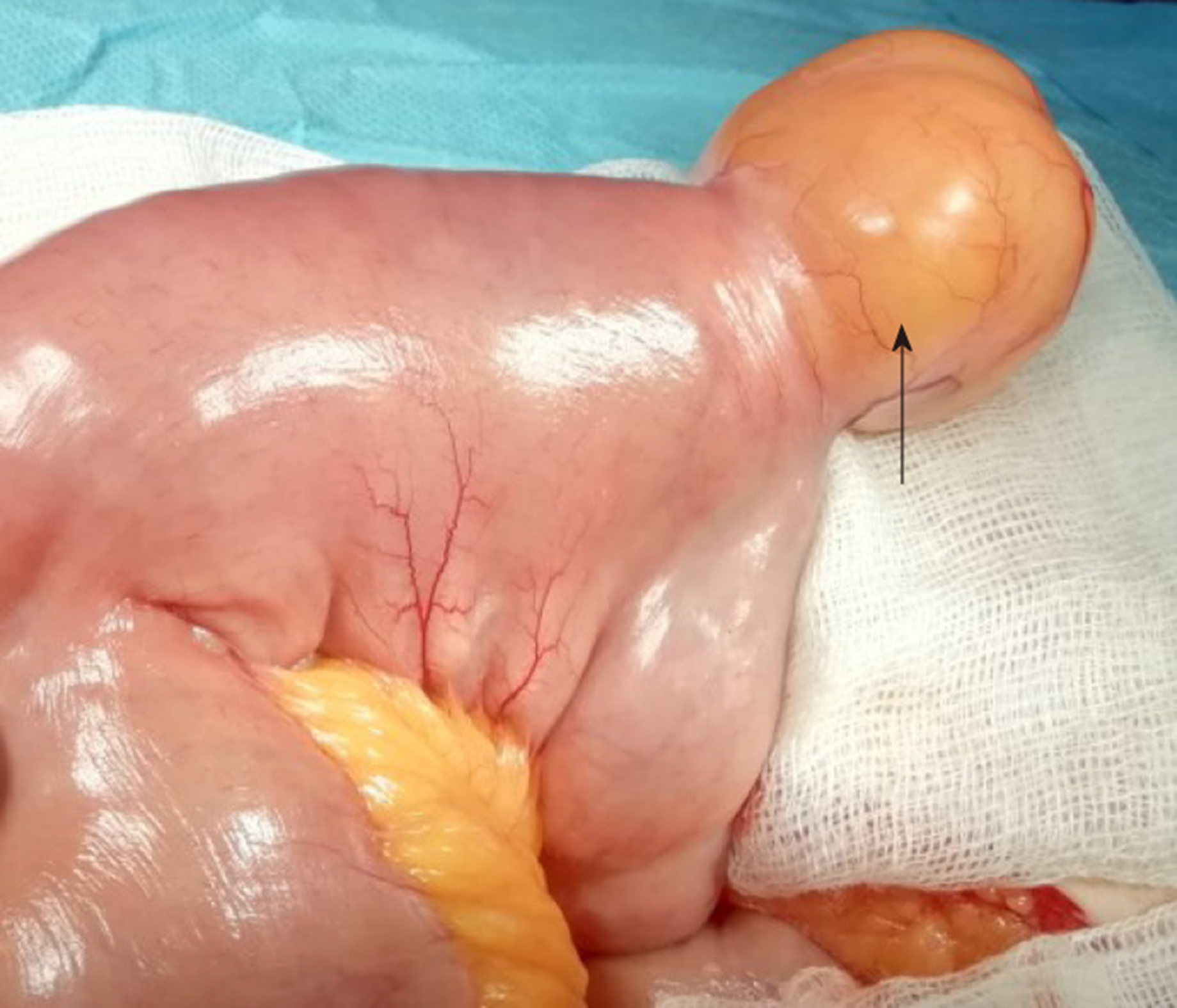
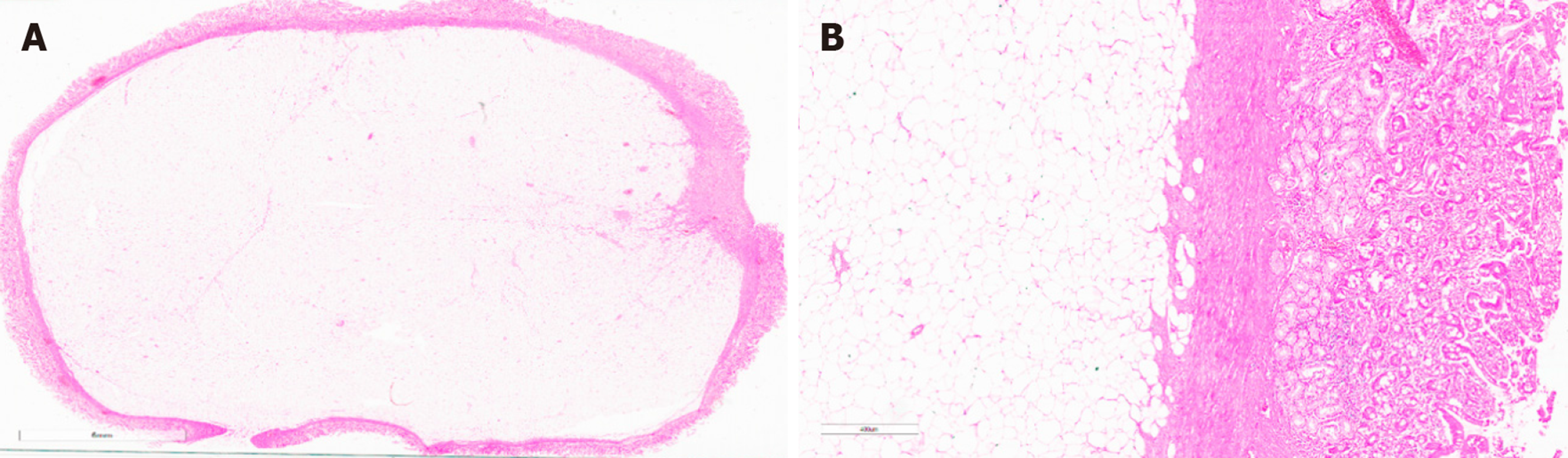
Intra-operative macroscopic observation identified six centimeters intussuscepted yellowish mass suggestive for lipoma (Figure 4). The histological examination revealed in the submucosa a nodular mesenchymal tumor consisting in mature adipocytes, with no pleomorphism and no mitotic activity. These findings were compatible with a diagnosis of lipoma (Figure 5A and B).
The intussuscepted jejunal segment was resected en bloc and the inspection of this segment showed a submucosal firm mass with ulceration of the mucosa. End-to-end anastomosis was performed.
The patient made an uneventful recovery and was discharged seven days later, and at six months follow-up he had no complains and his hemoglobin returned to normal value.
Jejunal lipomas are rare, but they may, nonetheless, represent a diagnostic challenge when complicated by lower gastrointestinal tract hemorrhage or intussusception. Large benign tumors of the small bowel rarely include intussusception in their spectrum, which may become an important risk factor for ischemia and necrosis of the intestinal wall.
The most common sites of GI lipomas reported in the literature are the colon (64%), followed by the small bowel (31%), stomach (3%) and the esophagus (12%)[6]. While most of small bowel lipomas are small in size and asymptomatic, those surpassing 2 cm in size usually manifest through clinical symptoms such as abdominal pain, hemorrhage or bowel obstruction[7].
In adult patients, intussusception is more likely to present progressive misleading symptomatology with diffuse abdominal pain and rarely with classical triad-symptoms such as intense abdominal pain, vomiting and lower gastrointestinal hemorrhage, making the diagnosis complex and requiring further radiological documentation. Intussusception is documented frequently on computed tomography, a method of choice due to its accuracy of virtually staging the lesion[8]. Over 90% of intussusception cases found in adults have an organic cause[9].
In order to find similar cases, we have reviewed the literature using Pub Med and found ten cases in the published accounts[4,10-18]. The keywords used were “lipoma”, “intussusception”, “jejunum”, “bleeding”. All ten cases presented jejunal lipoma with intussusception and bleeding (Table 1).
| Ref. | Gender/Age | Diagnostic modality | Size (cm) | Treatment |
| Ferrara et al[10], 2011 | F/78 | CT, VCE, Laparoscopy | 3 × 3 × 2.5 | Surgical resection |
| Mouaqit et al[11], 2012 | M/35 | CT, Laparotomy | 4 | Surgical resection |
| Pinto et al[12], 2018 | M/46 | CT, VCE, Enteroscopy | 7.5 | Surgical resection |
| Sarabjit et al[13], 2013 | M/22 | CT, Exploratory laparotomy | 4 | Surgical resection |
| Manouras et al[4], 2007 | M/55 | CT, Laparoscopy | 4 × 4 | Surgical resection |
| Yiğitler et al[14], 2007 | M/76 | US, CT | 4 × 5 | Surgical resection |
| Charalambous et al[15], 2012 | M/46 | CT, Laparotomy | 4 × 4 | Surgical resection |
| Kida et al[16], 2017 | M/67 | CT, Enteroscopy | 4 | Surgical resection |
| Akyüz et al[17], 2018 | F/61 | CT | 1.5 × 1.5 | Surgical resection |
| Baron et al[18], 1996 | F/60 | CT | 5 | Surgical resection |
Over the past decade, there has been a constant debate about the appropriate and safe treatment of small bowel benign tumors. Clinical presentation differed probably on account of the different sizes in tumoral mass. Yu et al[19] reported fifteen cases of gastrointestinal lipomas with different sizes that benefited from endoscopic therapy without important complications. However, it should be noted that endoscopic resection may be associated with a risk of bleeding and perforation. Thus, Raju et al[20] reported that endoscopic removal of lipomas > 2 cm in diameter was associated with a greater risk of perforation. In our case, the patient presented a tumor over 5 cm in length with a wide base of implantation. Due to its size and vascularization, surgical resection was considered to be the optimal treatment.
Jejunal lipomas, very rare benign tumors of the GI tract, are mostly asymptomatic and found incidentally during investigations for other abdominal diseases. However, in some cases, they may lead to complications such as intussusception and hemorrhage. Surgical resection remains the treatment of choice for large and complicated lipomas.
CARE Checklist (2016) Statement: The manuscript was prepared and revised according to the CARE Checklist (2016).
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Romania
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Kwon KA S-Editor: Zhang L L-Editor: A E-Editor: Liu JH
| 1. | Zirpe D, Wani M, Tiwari P, Ramaswamy PK, Kumar RP. Duodenal Lipomatosis as a Curious Cause of Upper Gastrointestinal Bleed: A Report with Review of Literature. J Clin Diagn Res. 2016;10:PE01-PE04. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Kordzadeh A, Lorenzi B, Elias S, Khan MJK, Charalabopoulos A. Subtle presentation of jejunal lipomata with intussusception in a young adult. J Surg Case Rep. 2017;2017:rjx199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Uyulmaz S, Zünd M, Caspar U, Diebold J, Slankamenac K. Ileoileal intussusception in unspecific recurrent abdominal pain in adult: A case report. SAGE Open Med Case Rep. 2018;6:2050313X18792814. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Manouras A, Lagoudianakis EE, Dardamanis D, Tsekouras DK, Markogiannakis H, Genetzakis M, Pararas N, Papadima A, Triantafillou C, Katergiannakis V. Lipoma induced jejunojejunal intussusception. World J Gastroenterol. 2007;13:3641-3644. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 44] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Onkendi EO, Grotz TE, Murray JA, Donohue JH. Adult intussusception in the last 25 years of modern imaging: is surgery still indicated? J Gastrointest Surg. 2011;15:1699-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 51] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Toya Y, Endo M, Orikasa S, Sugai T, Matsumoto T. Lipoma of the small intestine treated with endoscopic resection. Clin J Gastroenterol. 2014;7:502-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Wilson JM, Melvin DB, Gray G, Thorbjarnarson B. Benign small bowel tumor. Ann Surg. 1975;181:247-250. [PubMed] |
| 8. | Heiken JP, Forde KA, Gold RP. Computed tomography as a definitive method for diagnosing gastrointestinal lipomas. Radiology. 1982;142:409-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 64] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Martínez-Ubieto F, Jiménez-Bernadó T, Bueno-Delgado A, Martínez-Ubieto J, Pascual-Bellosta A. Recurrent intestinal intussusception in an adult due to intestinal pseudopolyps not associated with inflammatory bowel disease: a case report. J Med Case Rep. 2015;9:260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Ferrara F, Duburque C, Quinchon JF, Gaudissart Q. Laparoscopic resection of small bowel lipoma causing obscure gastrointestinal bleeding. Updates Surg. 2012;64:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Mouaqit O, Hasnai H, Chbani L, Benjelloun B, El Bouhaddouti H, Ibn El Majdoub K, Toughrai I, Laalim SA, Oussaden A, Maazaz K, Amarti A, Taleb KA. Adult intussusceptions caused by a lipoma in the jejunum: report of a case and review of the literature. World J Emerg Surg. 2012;7:28. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Pinto J, Castela J, Mão de Ferro S. Jejunal Lipoma, an Uncommon Cause of Gastrointestinal Bleeding. GE Port J Gastroenterol. 2018;25:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Sarabjit S, Dabar S, Suman S, Vineet K. Intussusception due to Jejunal Lipoma: A Case Report. JIMSA. 2013;26:112-113. |
| 14. | Yiğitler C, Ataç K, Yiğit T, Güleç B, Balkan M, Oner K. [A rare cause of bleeding intestinal intussusception in adult: jejunal lipoma]. Ulus Travma Acil Cerrahi Derg. 2007;13:237-240. [PubMed] |
| 15. | Charalambous G, Katergiannakis V, Manouras A. Jejunojejunal lipoma causing intussusception. Case Rep Gastroenterol. 2012;6:684-688. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Kida A, Matsuda K, Matsuda M, Sakai A, Noda Y. A unique case of massive gastrointestinal bleeding. SAGE Open Med Case Rep. 2017;5:2050313X17700345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Akyüz U, Erzin Y, Gürses B, Yalniz F, Pata C. Jejunal lipoma causing intussusception and gastrointestinal bleeding. Turk J Gastroenterol. 2008;19:291-292. [PubMed] |
| 18. | Baron Y, Priesack W, Sötje G, Brix F, Scheunemann C. Hemorrhagic jejunal lipoma with intermittent intussusception. Eur J Radiol. 1996;22:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Yu HG, Ding YM, Tan S, Luo HS, Yu JP. A safe and efficient strategy for endoscopic resection of large, gastrointestinal lipoma. Surg Endosc. 2007;21:265-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 20. | Raju GS, Gomez G. Endoloop ligation of a large colonic lipoma: a novel technique. Gastrointest Endosc. 2005;62:988-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 43] [Article Influence: 2.2] [Reference Citation Analysis (0)] |