Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3649
Peer-review started: August 18, 2019
First decision: September 9, 2019
Revised: September 23, 2019
Accepted: October 5, 2019
Article in press: October 5, 2019
Published online: November 6, 2019
Processing time: 81 Days and 18.2 Hours
We report a case of giant gastroduodenal trichobezoar, an extremely rare upper gastrointestinal bezoar due to trichotillomania and trichophagia.
The patient was a 10-year-old girl who presented with an abdominal mass that was discovered at palpation and noninvasive imaging examinations. Computed tomography (CT) showed a well-circumscribed heterogeneous mass extending from the stomach into the duodenum. The patient underwent a laparotomy to pull out the trichobezoar. Although these imaging findings are nonspecific, trichobezoar should be included in the differential diagnosis of gastric mass, especially with the history of an irresistible urge to pull out and swallow their hair.
Laparotomy is useful and practical for the management of giant gastroduodenal trichobezoar.
Core tip: A case of giant gastroduodenal trichobezoar, an extremely rare upper gastrointestinal bezoar due to trichotillomania and trichophagia, is reported. The patient was a 10-year-old girl who presented with an abdominal mass that was discovered at palpation and noninvasive imaging examinations. Computed tomography showed a well-circumscribed heterogeneous mass extending from the stomach into the duodenum. Laparotomy is useful and effective for the treatment of giant gastroduodenal trichobezoar.
- Citation: Dong ZH, Yin F, Du SL, Mo ZH. Giant gastroduodenal trichobezoar: A case report. World J Clin Cases 2019; 7(21): 3649-3654
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3649.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3649
A trichobezoar is a rarely encountered mass of hair, wool, and similar material in the stomach and intestine of some patients with trichotillomania and trichophagia. The accumulated hair within the stomach and intestine is resistant to digestion, which occasionally presents as trichobezoar-induced bowel or gastric outlet obstruction[1-6]. Moreover, trichobezoar frequently leads to a spectrum of nonspecific clinical findings, including early satiety, anorexia, vomiting, and vague abdominal pain[7,8]. Clinically, most of the trichobezoars are usually found in young females between 15 and 20 years of age because of their nonspecific presentations or even lack of clinical symptoms in the early stage[9,10]. Herein, we describe the clinical and imaging features of a 10-year-old girl determined as having a giant gastroduodenal trichobezoar with a history of an uncontrolled urge to pull out her hair (trichotillomania) and swallow it (trichophagia).
A ten-year-old girl presented to our emergency department with a one-day history of abdominal pain after intermitten vomiting of gastric contents and inappetence for approximately 9 d.
Acute gastritis was initially suspected, while it was not supported by the symptoms and therapy history.
It is noteworthy that her mother admitted that this girl had developed an irresistible habit of pulling and swallowing her hair from two years old, which mainly happened unconsciously during sleep or when she was lonely.
Her parents had no history of swallowing hair.
On physical examination, a movable mass was palpable in the left upper quadrant, and no sign of a rebound, peritonitis, or apparent hair loss was noted.
Laboratory results indicated anemia, hypoproteinemia, and hyponatremia, with a hemoglobin level of 115 g/L (normal range, 120–160 g/L), hematocrit 33.5% (normal range, 35.0%-49.0%), total protein 58 g/L (normal range, 63-82 g/L), albumin 28 g/L (normal range, 35-50 g/L), and natrium 136 mEq/L (normal range, 137-145 mEq/L). An elevated white blood cell count of 10050/µL (normal range, 4000–10000/µL) and a neutrophil ratio of 80% (normal range, 50.0%-70.0%) were demonstrated.
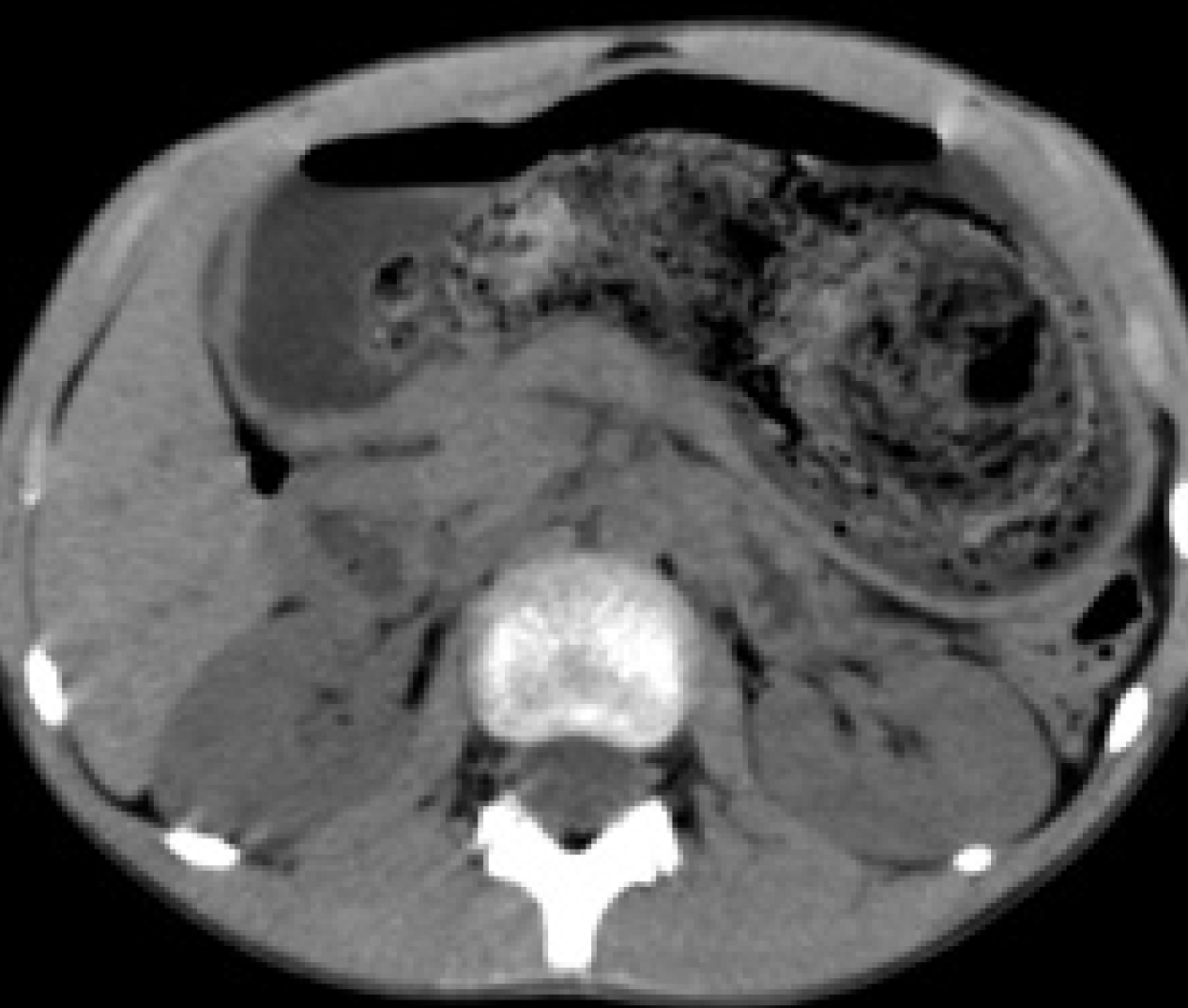
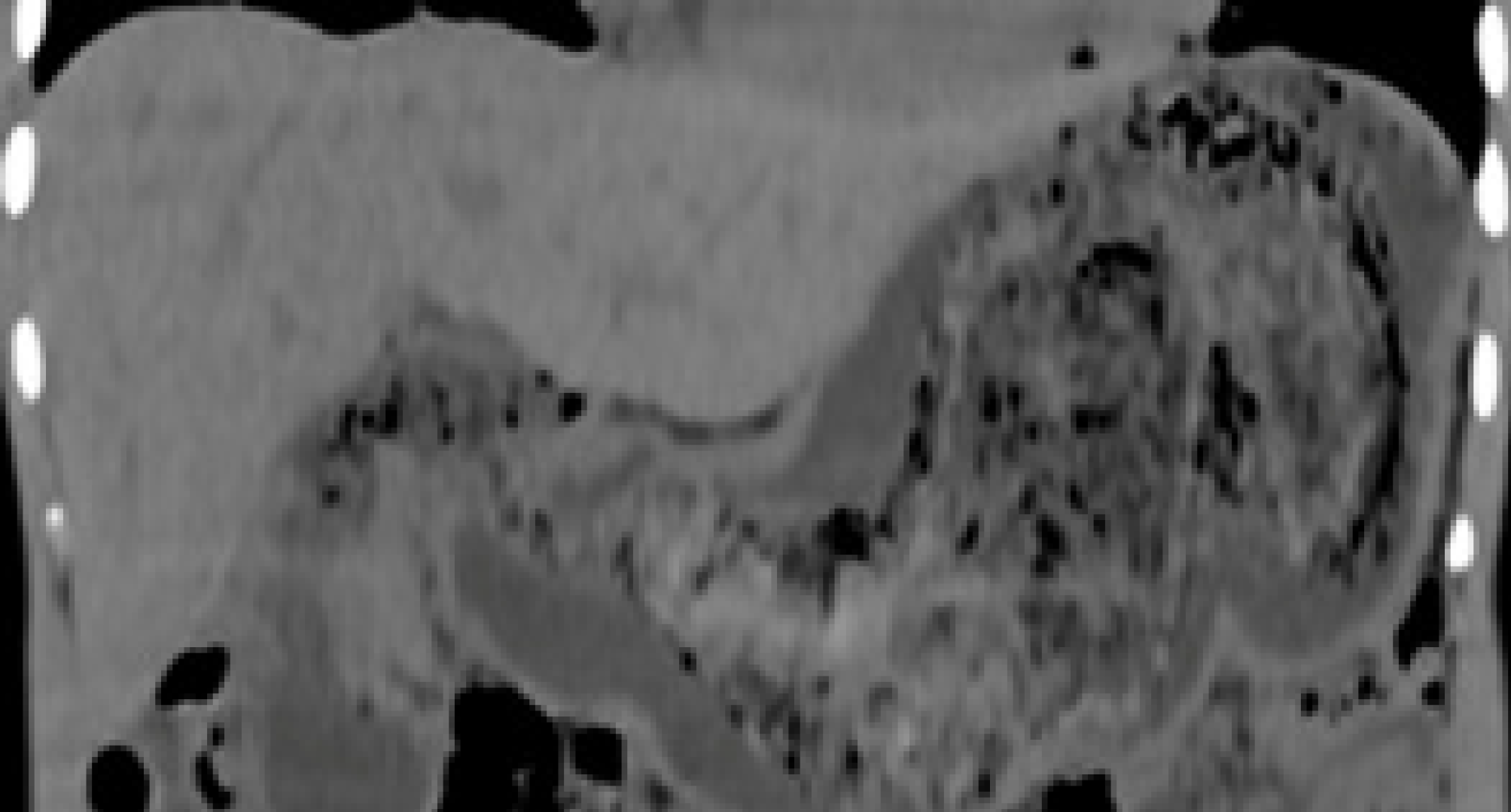
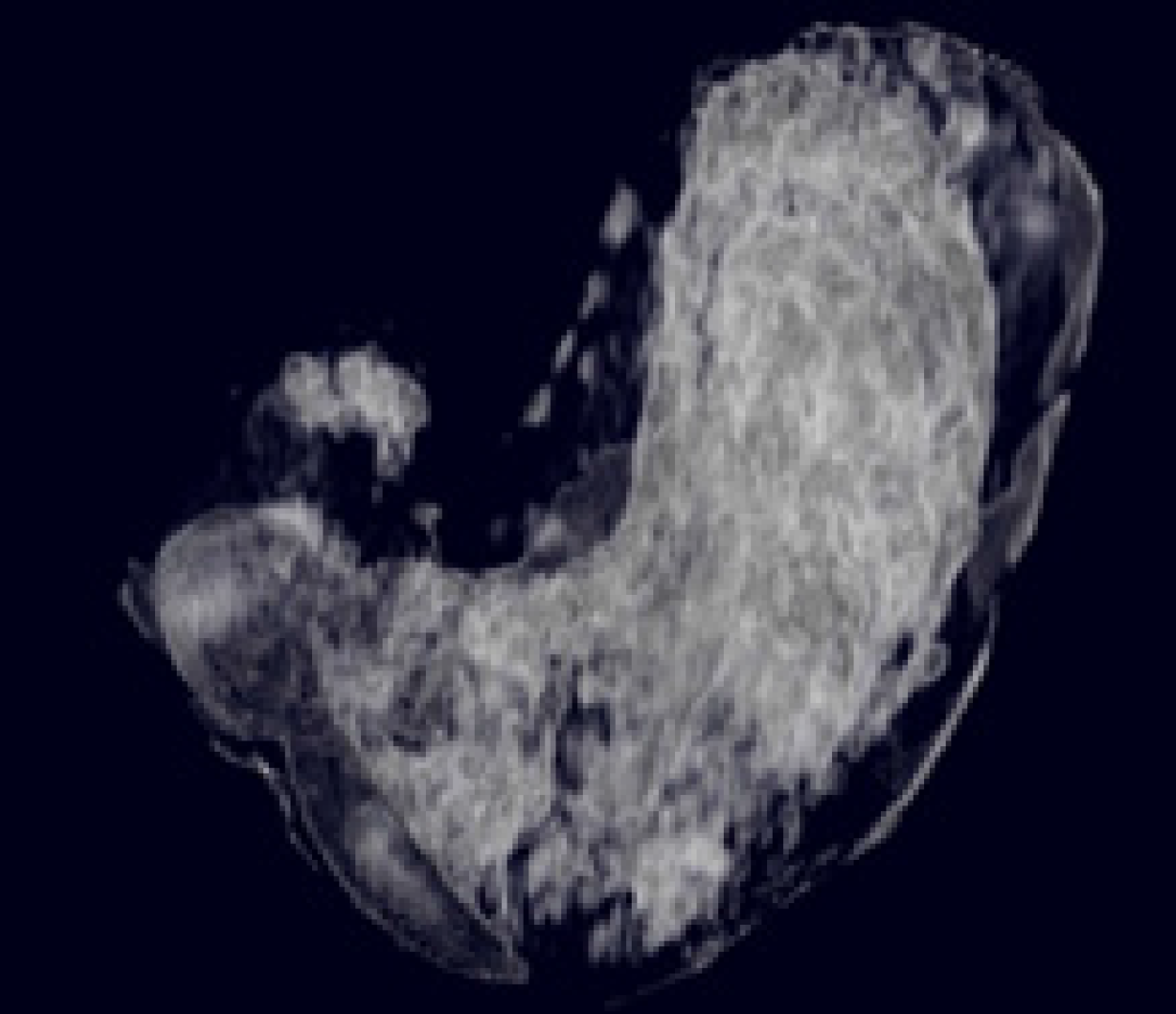
Noninvasive imaging examinations were performed, including plain chest radiography, ultrasound, and computed tomography (CT). Plain radiographs showed that the the chest was normal. Abdominal ultrasound demonstrated an intragastric hyperechoic mass, with a prominent posterior acoustic shadow of 13 cm in the maximum diameter. The residualdual gastric cavity could be detected at the fundus of 1.3 cm in width after drinking 300 mL of water. Noncontrasted-enhanced CT clearly showed a heterogeneous, meshlike mass with air sign filling the gastric cavity, from the fundus to the pylorus, measuring approximately 12.7 cm × 9.4 cm × 5.3 cm in size (Figure 1). On the coronal CT images, the mass extended from the stomach into the duodenum (Figure 2). Furthermore, the well-defined margin of the mass was outlined by the surrounding air in the stomach on the three-dimensional (3D) maximum intensity projection images (Figure 3).
Based on the clinical, imaging, and surgical outcomes, the final diagnosis was a giant gastroduodenal trichobezoar due to trichotillomania and trichophagia.
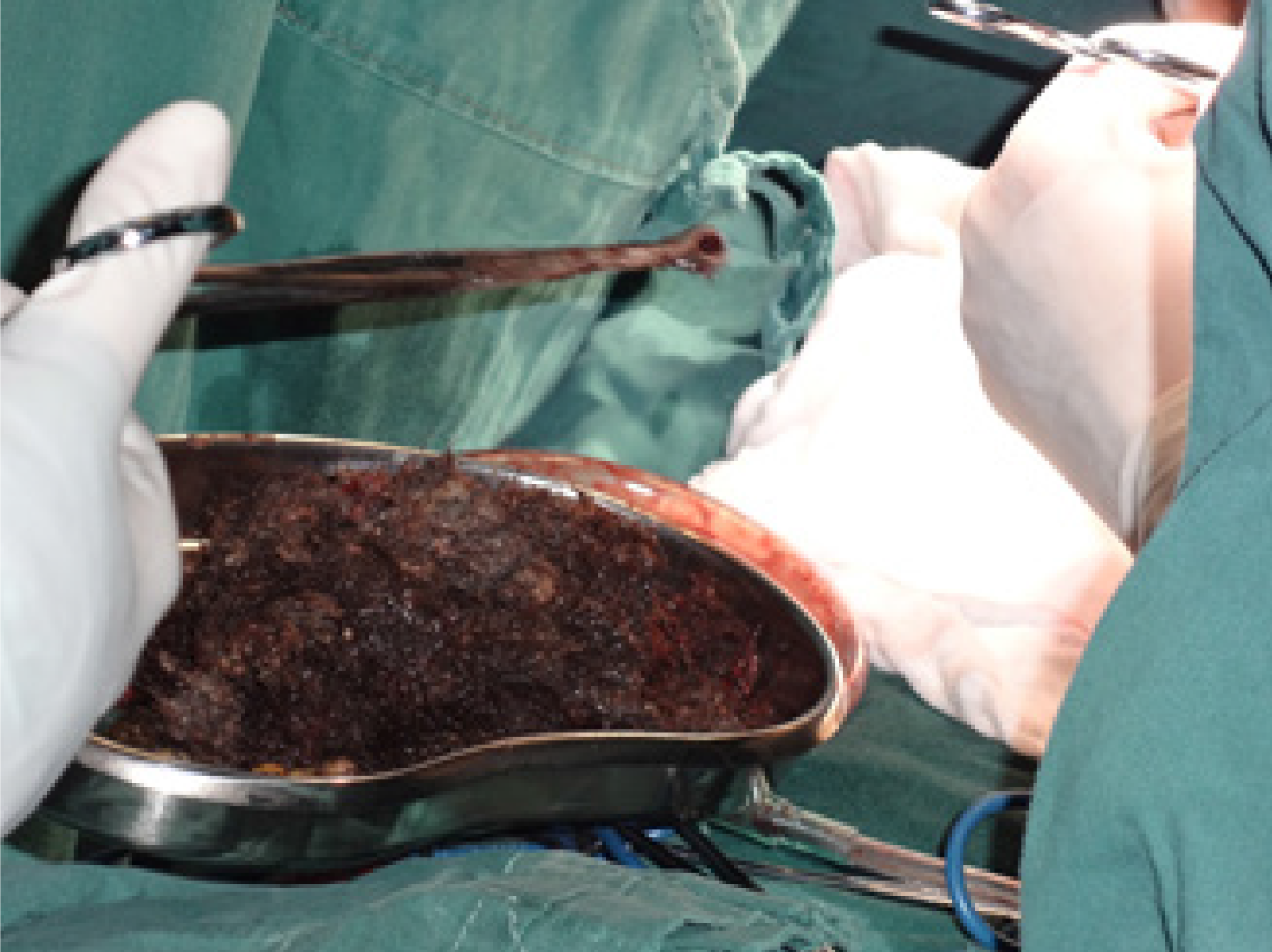
Since the mass was so large, laparotomy was considered (Figure 4). Under general anesthesia, all the imaging findings mentioned above were confirmed during the surgical process.
The postoperative course was uneventful, and the girl was referred to behavioral and mental health providers after discharge.
In 1779, Baudamant described the first case of trichobezoar that is one of the bezoars with intraluminal accumulations of indigestible ingested hair. Trichotillomania is an uncommon disorder affecting about 1% of the population, and one-third of these patients have trichophagia[11]. It usually occurs in patients with mental retardation, personality or psychiatric abnormalities, and sufferers have an irresistible urge to pull out and swallow their hair, termed as trichotillomania and trichophagia. Occasionally, Rapunzel syndrome is encountered as an infrequent complication of trichobezoar formation in which the gastric bezoar is extended into the duodenum and small intestine, which can increase the risk of complications such as obstruction and perforation. Trichobezoar with Rapunzel syndrome is predominantly found in emotionally disturbed or developmentally disabled youngsters because of their nonspecific presentations or even lack of clinical symptoms in the early stage[12].
Clinically, patients with trichobezoar frequently present nonspecific symptoms and signs including loss of appetite, weight loss, vomiting, and abdominal pain[10,13,14]. After long periods of time, the epigastric mass can be palpable when it is gradually enlarged, even associated with trichobezoar-induced gastric pylorus or bowel obstruction. In clinical practice, early diagnosis may be difficult for these nonspecific symptoms and signs. However, advanced noninvasive imaging modalities, including conventional upper gastrointestinal radiography, ultrasound, CT, and nuclear magnetic resonance imaging (MRI), are beneficial for making preoperative diagnosis and clinical management decision as previously reported[13,15-19]. In our case, the little girl was initially suspected with acute gastritis based on the nonspecific symptoms and laboratory results such as abdominal pain, anemia, hypoproteinemia, and hyponatremia. Fortunately, ultrasound and CT provided the positive information for the diagnosis, especially combined with 3D reconstructed CT images. As a noninvasive and nonirradiated tool, MRI is also useful for detecting this entity, especially in the pediatric population[20]. More importantly, the history of mental disorder, the uncontrolled urge to pull out one’s hair and swallow it, is vital as a critical clue for making a clinical diagnosis. After the diagnosis is made, treatment modalities, including observation, dissolution, and surgery, could be considered. When a thickened mass is detected, surgical approach severing as an optimal choice could either be laparoscopic or open laparotomy[6,8,12,21,22]. Before the operation, noninvasive imaging modalities are beneficial for the pre- and post-operative assessment of trichobezoar and its possible complications, which can help make management decisions to reduce the frequency of clinical hazards.
As above, laparotomy is useful and practical for the treatment of giant gastroduodenal trichobezoar.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ishibashi H, Zimmerman M S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Liu MY
| 1. | Al-Wadan AH, Al-Absi M, Al-Saadi AS, Abdoulgafour M. Rapunzel syndrome. Saudi Med J. 2006;27:1912-1914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Balik E, Ulman I, Taneli C, Demircan M. The Rapunzel syndrome: a case report and review of the literature. Eur J Pediatr Surg. 1993;3:171-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 3. | Dalshaug GB, Wainer S, Hollaar GL. The Rapunzel syndrome (trichobezoar) causing atypical intussusception in a child: a case report. J Pediatr Surg. 1999;34:479-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Dindyal S. Bhuva Nj, Dindyal S, Ramdass M, Narayansingh V. Trichobezoar presenting with the 'comma sign' in Rapunzel Syndrome: a case report and literature review. Cases J. 2008;1:286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Duncan ND, Aitken R, Venugopal S, West W, Carpenter R. The Rapunzel syndrome. Report of a case and review of the literature. West Indian Med J. 1994;43:63-65. [PubMed] |
| 6. | Hassan AA, Panesar KJ. The Rapunzel syndrome: a rare presentation of trichobezoar. Ulster Med J. 1989;58:94-96. [PubMed] |
| 7. | Fallon SC, Slater BJ, Larimer EL, Brandt ML, Lopez ME. The surgical management of Rapunzel syndrome: a case series and literature review. J Pediatr Surg. 2013;48:830-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Gorter RR, Kneepkens CM, Mattens EC, Aronson DC, Heij HA. Management of trichobezoar: case report and literature review. Pediatr Surg Int. 2010;26:457-463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 163] [Cited by in RCA: 167] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 9. | Lalith S, Gopalakrishnan KL, Ilangovan G, Jayajothi A. Rapunzel Syndrome. J Clin Diagn Res. 2017;11:TD01-TD02. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Mathai J, Chacko J, Kumar TS, Scott JX, Agarwal I, Varkki S. Rapunzel syndrome: a diagnosis overlooked. Acta Paediatr. 2007;96:135-137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Frey AS, McKee M, King RA, Martin A. Hair apparent: Rapunzel syndrome. Am J Psychiatry. 2005;162:242-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 12. | Gonuguntla V, Joshi DD. Rapunzel syndrome: a comprehensive review of an unusual case of trichobezoar. Clin Med Res. 2009;7:99-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 107] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 13. | Mehta P, Bhutiani R. The Rapunzel syndrome: is it an Asian problem? (case report and review of literature). Eur J Gastroenterol Hepatol. 2009;21:937-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Middleton E, Macksey LF, Phillips JD. Rapunzel syndrome in a pediatric patient: a case report. AANA J. 2012;80:115-119. [PubMed] |
| 15. | Nour I, Abd Alatef M, Megahed A, Yahia S, Wahba Y, Shabaan AE. Rapunzel syndrome (gastric trichobezoar), a rare presentation with generalised oedema: case report and review of the literature. Paediatr Int Child Health. 2019;39:76-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Obinwa O, Cooper D, Khan F, O'Riordan JM. Rapunzel syndrome is not just a mere surgical problem: A case report and review of current management. World J Clin Cases. 2017;5:50-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV. Trichobezoars in the stomach and ileum and their laparoscopy-assisted removal: a bizarre case. Singapore Med J. 2007;48:e37-e39. [PubMed] |
| 18. | Tayyem R, Ilyas I, Smith I, Pickford I. Rapunzel syndrome and gastric perforation. Ann R Coll Surg Engl. 2010;92:W27-W28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Western C, Bokhari S, Gould S. Rapunzel syndrome: a case report and review. J Gastrointest Surg. 2008;12:1612-1614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 20. | Ben Cheikh A, Gorincour G, Dugougeat-Pilleul F, Dupuis S, Basset T, Pracros JP. [Gastric trichobezoar in an adolescent presenting with anemia: ultrasound and MRI findings]. J Radiol. 2004;85:411-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Jones GC, Coutinho K, Anjaria D, Hussain N, Dholakia R. Treatment of recurrent Rapunzel syndrome and trichotillomania: case report and literature review. Psychosomatics. 2010;51:443-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |