Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3590
Peer-review started: June 4, 2019
First decision: August 1, 2019
Revised: August 24, 2019
Accepted: September 11, 2019
Article in press: September 11, 2019
Published online: November 6, 2019
Processing time: 161 Days and 15.5 Hours
Squamous cell carcinoma (SCC) of the nail bed is a poorly reported malignant subungual tumor. Because it presents with nonspecific symptoms and signs, it is frequently misdiagnosed by dermatologists or surgeons. A delay in diagnosis and/or wrong treatment might increase the possibility of disease progression. Thus, new perspectives are needed to assist dermatologists and surgeons with diagnosing and treating SCC. This rare case presented with a 2-year delay in the diagnosis of SCC teaches a valuable lesson.
A 62-year-old female presented with a non-healing subungual growth in the nail bed of the right middle finger for 2 years. The lesion was first medicated with iodine by the patient herself without any relief. Twenty months later, a dermatologist diagnosed the lesion as paronychia and treated it with nail avulsions repeatedly with no obvious alleviation. A lesionectomy confirmed the lesion was SCC. An extended excision of the tumor with amputation of the distal interphalangeal joint was subsequently performed. A biopsy of sentinel lymph nodes was negative. Due to the result of preoperative positron emission tomography-computed tomography scanning, sweeping of axillary lymph nodes was considered dispensable and was skipped. At the 2-year follow-up, the patient showed a quick recovery and no sign of recurrence.
Our successful diagnosis and treatment of the case highlights the need for additional attention to long-standing non-healing lesions of the nail bed and the necessity for discreet evaluation and customization of surgical interventions.
Core tip: Squamous cell carcinoma of the nail bed is a malignant subungual tumor that is poorly reported. Considering its nonspecific symptoms and signs, it is usually misdiagnosed by dermatologists or surgeons. We present herein, a rare case of squamous cell carcinoma in the nail bed in which the diagnosis was delayed by belated medical help and misdiagnosis. Our successful diagnosis and treatment of the case highlights the need for additional attention to long-standing non-healing lesions of the nail bed and the necessity for discreet evaluation and customization of surgical interventions.
- Citation: Li PF, Zhu N, Lu H. Squamous cell carcinoma of the nail bed: A case report. World J Clin Cases 2019; 7(21): 3590-3594
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3590.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3590
Squamous cell carcinoma (SCC) of the nail bed is a poorly reported low-grade malignant tumor that preferentially involves the digits of hands[1,2]. Risk factors for the development of SCC include trauma, chronic paronychia, chronic actinic damage, X-ray irradiation, burns, and chemical or virus exposure among others[3]. Its resemblance to various common nail disorders and the lack of specific clinical signs or symptoms lead to frequent misdiagnoses or a long delay in finding a diagnosis[4]. A delay in diagnosis and/or wrong treatment might increase the possibility of disease progression. We report a case of SCC of the nail bed in which diagnosis was delayed by 2 years. It highlights a necessity for dermatologists or surgeons to be sensitive to specific clinical conditions and for customized treatment for patients.
A 62-year-old female patient presented in our clinic complaining of a painful, non-healing subungual growth at the lateral nail fold of the right middle finger for 2 years.
There was no history of trauma or other possible causes. Initially, though the growth occurred along with intermittent pain, it did not attract the patient’s attention. She self-medicated the lesion with iodine without any relief. Four months prior to our visit, she consulted a dermatologist who treated her twice for chronic paronychia by nail avulsion and corresponding medication. Granulated tissue recurred along with deformity of the nail plate.
The patient had a medical history of hypertension that was well-controlled by oral medication (Aprovel; irbesartan).
Examination revealed a subungual growth with granulated tissue overlying the ulnar side of the nail plate. Other nails of both the hands and feet were normal (Figure 1).
Blood and urine analysis were normal. The electrocardiogram and chest X-ray were also normal.
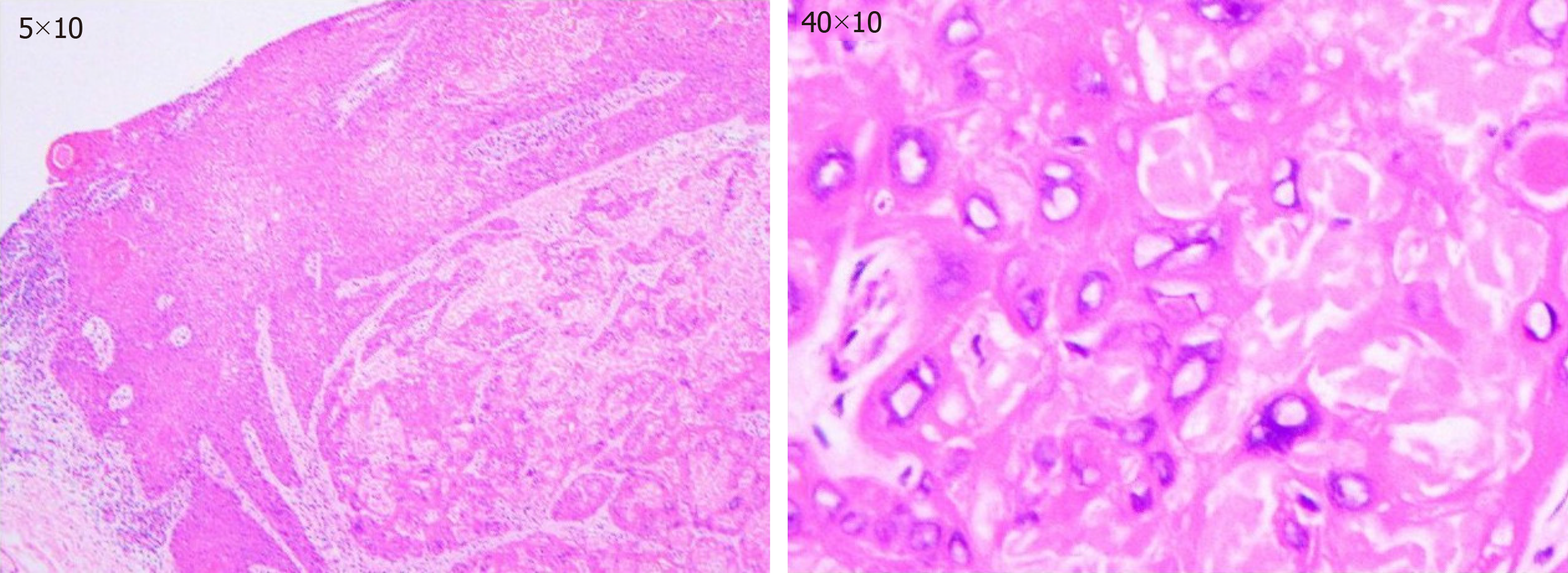
With the suspicion of SCC, pyoderma gangrenosum, and amelanotic melanoma, total nail avulsion along with excision of the growth and lateral nail fold of the right middle fingernail was performed and sent for histopathological examination. The result reported the lesion was SCC (Figure 2).
The final diagnosis of the presented case was SCC of the nail bed of the right middle finger.
Further physical examination showed no evidence of lymphadenopathy at the adjacent elbow or axilla or any cutaneous lesions suggestive of metastasis. An X-ray of the right middle finger showed no abnormalities. A type-B ultrasound detected multiple lymph nodes in both axillae. Positron emission tomography-computed tomography scanning showed no sign of metastasis or local inflammatory response in the right middle finger. The patient was then subjected to disarticulation of the distal interphalangeal joint followed by rotator advancement flap. With the aid of nanocarbon, sentinel lymph nodes were removed for intraoperative frozen section, which were negative. Further sweeping of axillary lymph nodes was skipped.
The patient responded favorably and was discharged 3 d later due to relatively minor injuries. No adverse events were observed. At the 2-year follow-up, there was no sign of tumor recurrence.
SCC of the nail bed is a rare disease, or at least it has been poorly reported[1,2]. Potential risk factors of SCC include trauma, chronic paronychia, chronic actinic damage, X-ray irradiation, burns, and chemical or virus exposure among others[3]. Its myriad of unspecific symptoms ranging from chronic intermittent pain, nail deformity, subungual growth, ulcers, and complicated infections[1,5], frequently lead to misdiagnoses, like chronic paronychia, onychomycosis, pyogenic granuloma, subungual wart, subungual glomus tumor, and enchondroma[5-7].
It was reported 40 years before that the delay in diagnosis of SCC of the nail bed was 4 years on average[4], which is a huge hazard for a patient’s well-being. Although conditions might be improved nowadays, practitioners should remain vigilant. Thus, we appeal that careful physical examination, assisting tests, and detailed history deserve much more attention when dealing with suspicious malignant lesions. Moreover, a biopsy of a non-healing ulcer lasting more than 1 mo should be considered a necessity. In this particular case, the patient self-medicated the lesion for 20 mo before seeking medical help, which warns us of the importance of popularizing medical inspection. Together with the Departments of Plastic Surgery and Dermatology, the Department of Hand Surgery in our hospital has initiated various ways in popularizing the importance of medical inspection for delayed lesions by distributing brochures, welfare lectures, and multimedia notification messages. We believe these measures can advance the timing of medical treatment, and we propose other hospitals do the same.
For surgical treatment, specific surgical planning depends on the extent of digit involvement and distal metastasis, which is highly related with the time of definite diagnosis[1]. Mohs micrographic surgery is an ideal model, providing a high possibility of curing the disease and maximally preserves the surrounding healthy tissue[8]. Nevertheless, for specific patients, customized treatment plans should be projected. As for our patient, after the histopathological examination proved the lesion was SCC, careful evaluation was performed for further surgical intervention. Although results from X-ray and positron emission tomography-computed tomography scans were negative, possible metastasis cannot be easily ignored because multiple lymph nodes in both axillae were detectable by type-B ultrasound. Considering the patient’s prognosis and quality of life postoperatively, we decided to disarticulate the distal interphalangeal joint, which was a complete and relatively less progressive treatment as well as a biopsy of sentinel lymph nodes with the assistance of nanocarbon to assess whether sweeping of axillary lymph nodes was necessary.
Our successful diagnosis and treatment of this case highlight the need for additional attention to long-standing non-healing lesions of the nail bed and the necessity for discreet evaluation and customization of surgical interventions.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koukourakis GV S-Editor: Zhang L L-Editor: Filipodia E-Editor: Qi LL
| 1. | Vashisht D, Singh PY, Tewari R, Baveja S. Squamous cell carcinoma of nail bed: A great mimicker. Med J Armed Forces India. 2018;74:190-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Tambe SA, Patil PD, Saple DG, Kulkarni UY. Squamous Cell Carcinoma of the Nail Bed: The Great Mimicker. J Cutan Aesthet Surg. 2017;10:59-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Frankel DH. Squamous cell carcinoma of the skin. Hosp Pract (Off Ed). 1992;27:99-102, 105-106. [PubMed] |
| 4. | Carroll RE. Squamous cell carcinoma of the nail bed. J Hand Surg Am. 1976;1:92-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Meesiri S. Subungual squamous cell carcinoma masquerading as chronic common infection. J Med Assoc Thai. 2010;93:248-251. [PubMed] |
| 6. | Lu H, Chen LF, Chen Q. Rupture of a subungual glomus tumor of the finger. BMC Cancer. 2018;18:505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Lu H, Chen Q, Yang H, Shen H. Enchondroma in the distal phalanx of the finger: An observational study of 34 cases in a single institution. Medicine (Baltimore). 2016;95:e4966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Goldminz D, Bennett RG. Mohs micrographic surgery of the nail unit. J Dermatol Surg Oncol. 1992;18:721-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | McGarry K, McBride M, Lewis H. Arm amputation secondary to squamous cell carcinoma: exotic expeditions leading to a delayed diagnosis? BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Ryu TH, Kye H, Choi JE, Ahn HH, Kye YC, Seo SH. Features Causing Confusion between Basal Cell Carcinoma and Squamous Cell Carcinoma in Clinical Diagnosis. Ann Dermatol. 2018;30:64-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Que SKT, Zwald FO, Schmults CD. Cutaneous squamous cell carcinoma: Incidence, risk factors, diagnosis, and staging. J Am Acad Dermatol. 2018;78:237-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 513] [Article Influence: 73.3] [Reference Citation Analysis (0)] |