Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3583
Peer-review started: June 10, 2019
First decision: September 9, 2019
Revised: September 29, 2019
Accepted: October 15, 2019
Article in press: October 15, 2019
Published online: November 6, 2019
Processing time: 151 Days and 22.1 Hours
Kawasaki disease (KD) is an acute type of systemic vasculitis involving small to medium-sized muscular arteries and outbreaks during childhood. KD can cause myocardial ischemia, infarction, and sudden cardiac arrest. We present a case of a young adult survivor of out-of-hospital cardiac arrest as late KD sequelae.
A 29-year-old man with presumed acute KD history at the age of 5 suddenly lost consciousness while jogging and was diagnosed a sudden cardiac arrest by an emergency doctor. After about 10 min cardiopulmonary resuscitation, return of spontaneous circulation was achieved, and the patient was transferred to our hospital. A coronary computed tomography angiogram and coronary angiography revealed extensive calcifications of left anterior descending and right coronary artery aneurysms. The patient was an active individual who took exercise regularly and claimed no previous symptoms of chest pain or shortness of breath on exertion. The most possible cause of his sudden cardiac arrest could be presumed as a thrombus within the coronary artery aneurysms. After that, a thromboembolism induced extensive ischemia, and this ischemia-induced arrhythmia led to a cardiac arrest.
Few patients who suffer a late sequela of KD can survive from out-of-hospital cardiac arrest. Medications, surgical intervention, and active follow-up are extremely important for this patient to prevent occurrence of adverse events in the future.
Core tip: Kawasaki disease (KD) is an acute type of systemic vasculitis involving small to medium-sized muscular arteries in childhood. One of the most severe complications of KD is coronary artery aneurysms. We reported a case of out-of-hospital cardiac arrest of a young adult survivor, who probably had KD during childhood. Undiagnosed and untreated KD can have serious long-term sequelae. Few patients who suffer a late sequela of KD can survive from out-of-hospital cardiac arrest. Timely cardiopulmonary resuscitation is very critical for survival of sudden cardiac arrest.
- Citation: Zhu KF, Tang LJ, Wu SZ, Tang YM. Out-of-hospital cardiac arrest in a young adult survivor with sequelae of childhood Kawasaki disease: A case report. World J Clin Cases 2019; 7(21): 3583-3589
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3583.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3583
Kawasaki disease (KD), first reported by Kawasaki in 1967[1], is an acute type of systemic vasculitis involving small to medium-sized muscular arteries in childhood. One of the complications of KD is a coronary artery (CA) aneurysm, with an incident rate of approximately 20% if left KD untreated[2]. CA aneurysm causes stenosis or occlusion of CA due to the remodeling of aneurysm, thereby resulting in ischemic heart disease, myocardial infarction, and sudden cardiac arrest[3-5]. Few patients who suffer a late sequela of KD can survive from out-of-hospital cardiac arrest. We treated one case of a 29-year-old survivor with no previous medical history. The patient was admitted to our hospital after cardiac arrest with extensive calcifications of multiple CA aneurysms, which we surmised to be residual lesions derived from the coronary arteritis of KD.
A 29-year-old Chinese man presented with a sudden loss of consciousness.
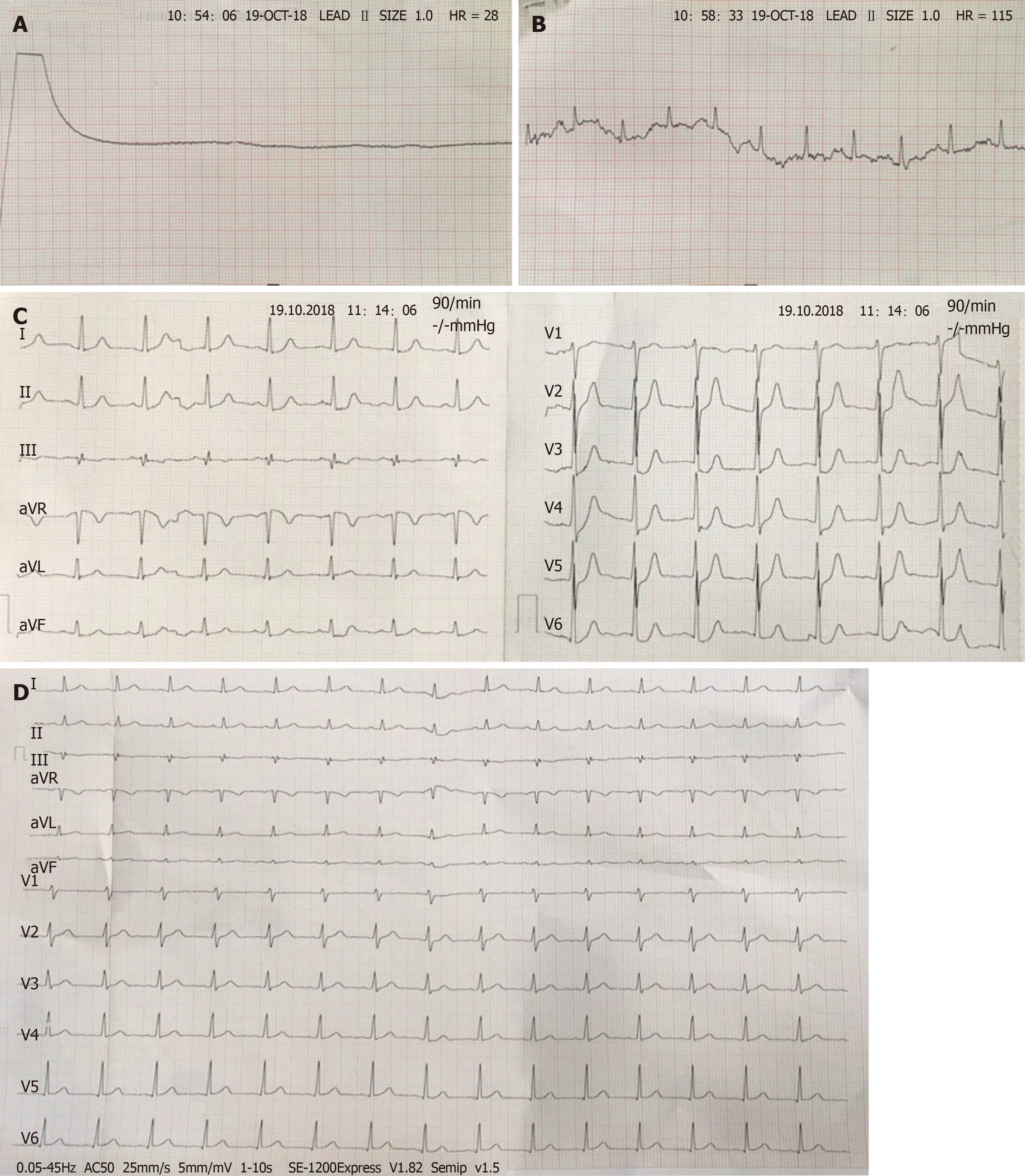
A 29-year-old Chinese man suddenly passed out while jogging at the school sports field. He was found unconscious with disappearance of carotid pulsation when a doctor from the school hospital arrived in 3 min. His electrocardiogram (ECG) showed a flat line without any electrical activities (Figure 1). Then he was quickly diagnosed with sudden cardiac arrest. After about 10 min cardiopulmonary resuscitation (CPR), return of spontaneous circulation was achieved, and the patient was transferred to our hospital for assessment as soon as the ambulance arrived. After admission, the patient regained consciousness on the next day and had no symptoms of discomfort. He claimed no previous symptoms of chest pain or shortness of breath on exertion.
The patient was an active individual who took exercise regularly with height of 183 cm and weight of 75 kg. He suffered a high fever at the age of 5 but was not able to recall whether there was any other discomfort like a skin rash. There was no other history of past illness.
He does not drink alcohol or smoke and has no history of trauma and drug use. This patient has no family history of cardiac disease or any clinical feature to suggest connective tissue disease.
Vital signs were steady during hospitalization. No abnormalities were found on cardiopulmonary examination. There were no swollen lymph nodes, and no skin rash on the whole body.
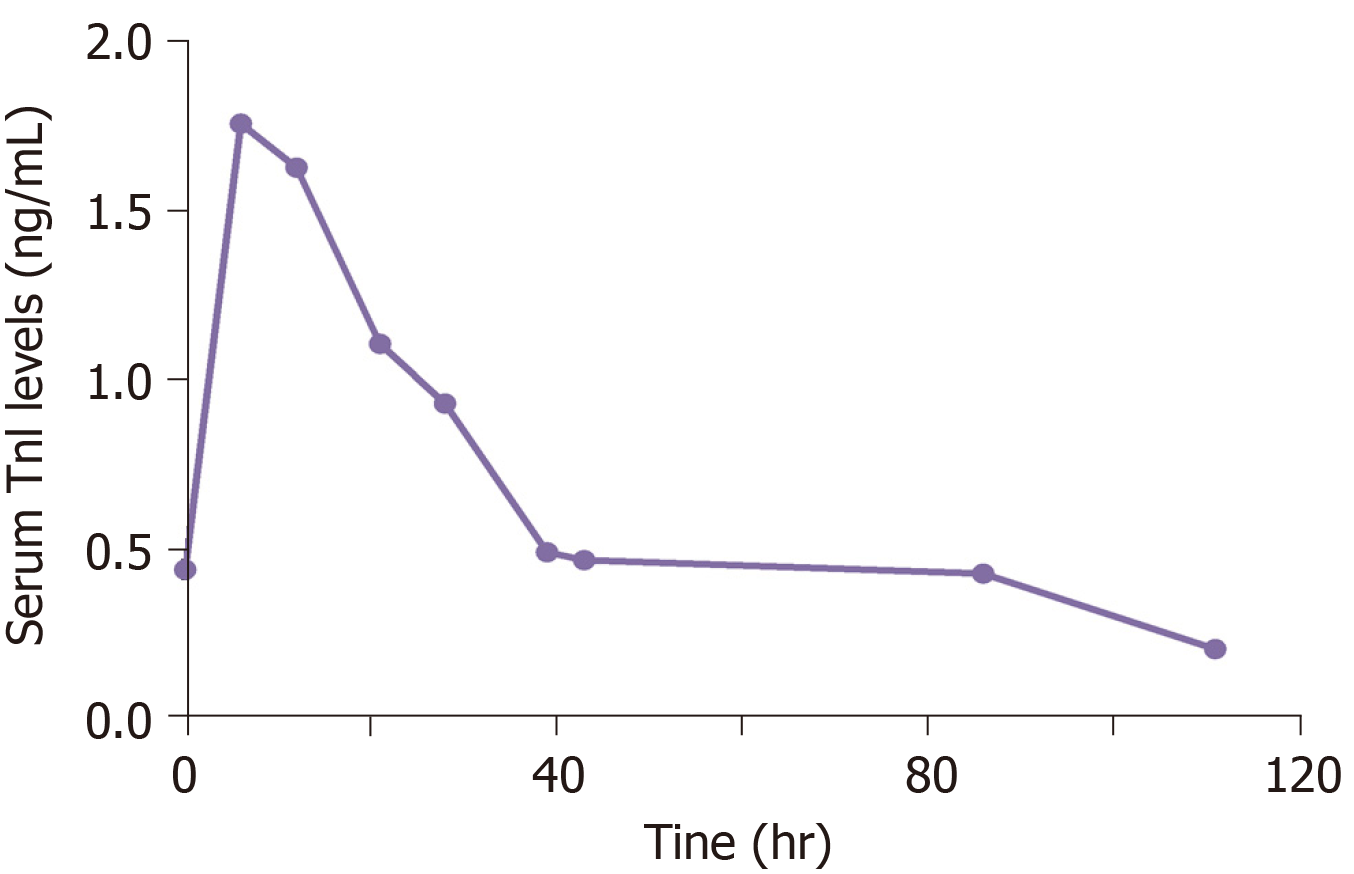
The levels of troponin I were slightly elevated from admission to normal levels after a few days (from 0.44 ng/mL to normal, Figure 2). His liver function suggested that alanine aminotransferase was 454 U/L and aspartate aminotransferase 357 U/L at admission, which gradually decreased to normal levels, consistent with the expression of myocardial injury markers. The blood routine showed that white blood cells (13.3 × 109/L) and neutrophils (11.3 × 109/L) were slightly increased at admission to normal levels after a few days. His routine chemistry panel was normal with sodium 138.94 mmol/L; potassium 4.00 mmol/L; and magnesium 0.84 mmol/L. His renal and coagulative functions were normal. Test results of syphilis antibody, human immunodeficiency virus antibody, hepatitis series, anti-nuclear antibodies, and antineutrophil cytoplasmic antibodies were negative. The 12-lead ECG performed upon admission showed depressed ST-segments in I, II, aVF, and V2-6 leads. Followed-up ECG 4 hr later showed normal ECG parameters (Figure 1).
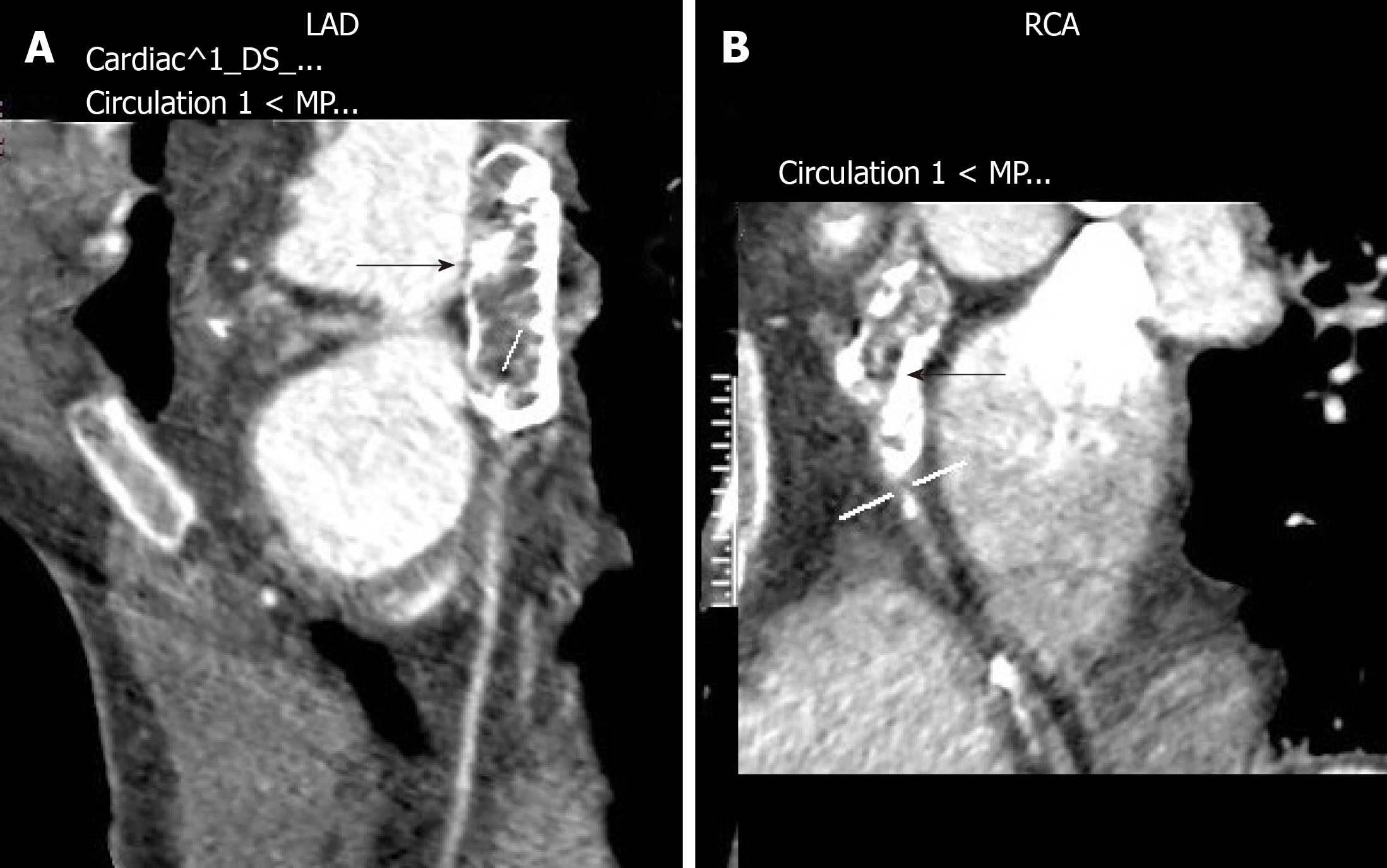
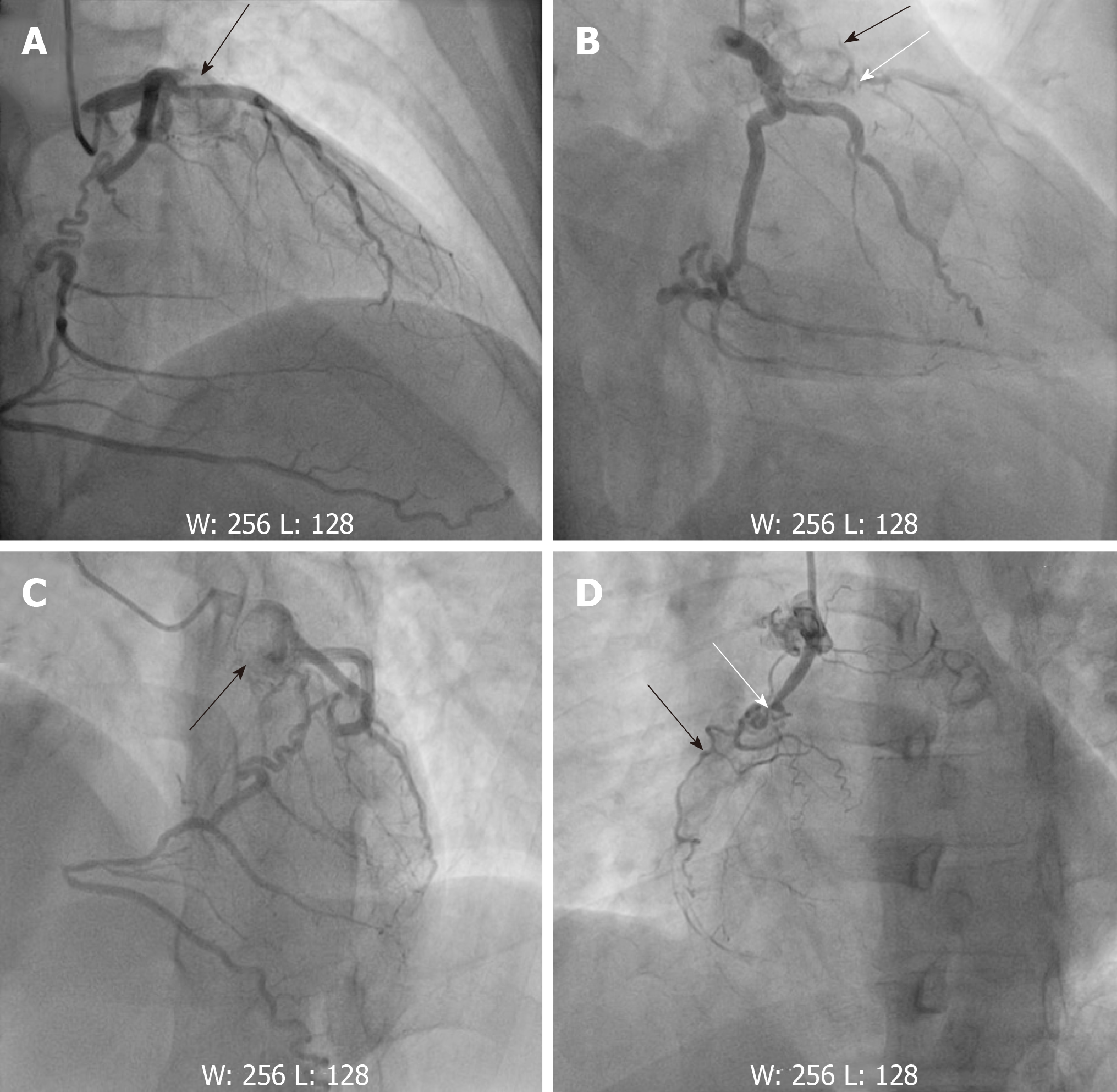
Echocardiography indicated normal atrial and ventricular size, normal wall thickness, normal systolic and diastolic function, and an ejection fraction of 63.2%. Computed tomography of brain showed no evidence of intracranial hemorrhage. Coronary computed tomography angiography (CTA) revealed marked aneurysms and extensive calcifications in the proximal and mid left anterior descending (LAD) and right coronary artery (RCA), (Figure 3). Coronary angiography was performed at day 10, which showed giant aneurysms of the proximal LAD with subtotal occlusion and the proximal and mid RCA with chronic total occlusion. The RCA received left-to-right epicardial collateral circulation from left circumflex coronary artery (Figure 4).
The final diagnosis of the presented case is CA aneurysms due to a cardiac sequela of KD at the age of 5.
The patient was medically managed with aspirin, clopidogrel, clexane, and isosorbide mononitrate. At day 28, the surgery of coronary artery bypass grafting was performed. The left internal mammary artery was grafted onto the LAD, and saphenous vein grafts were made to the left circumflex coronary artery and RCA.
There was no adverse event during the surgery, and the patient recovered well postoperatively with no complications. He is being regularly followed up since the operation. There were no myocardial ischemia symptoms, change in cardiac function, or adverse events during the 9-mo follow-up period.
The case described has several notable features. Firstly, to our best knowledge, the survival odds of patients with CA aneurysms after out-of-hospital cardiac arrest is low, and few cases were found in the literature. Previous studies revealed sudden cardiac death in undiagnosed KD patients was identified by histopathological analysis of the autopsy materials[6,7]. Secondly, the young adult who lives with CA aneurysms for approximately 24 years has normal heart function and is not affected by long-term cardiac ischemia. Additionally, medical treatment and coronary artery bypass grafting were successful, and long-term follow-up was well taken to this patient.
KD is not only the most common vasculitis in children, but it is also the most common vasculitis across all age groups[8]. One of the most severe complications of KD is CA aneurysms. If KD is not treated in time, about 20% of affected patients can end up with CA aneurysms[2,9]. CA aneurysms are classified into small size (< 4 mm), medium size (4 to 8 mm), and giant size (> 8 mm) based on their diameter[10]. Larger CA aneurysms in patients with KD were proved to have a higher probability of developing calcification. Kaichi et al[11] found that the prevalence of coronary calcification with initial diameters ≥ 6 mm was 12% at 5 years, 44% at 10 years, and 94% at 20 years. In this specific case, it took approximately 24 years for a significant calcification to develop.
Other diseases leading to CA aneurysms such as atherosclerosis, infectious diseases like syphilis, and connective tissue diseases like systemic lupus erythematosus also need to be identified. However, the patient was a young man without the history of metabolic syndrome such as hypertension and diabetes. Moreover, he had no fever or rash, and his blood test showed negative syphilis antibody and anti-nuclear antibodies. Thus, according to the patient’s past medical history, clinical manifestations and examinations, the patient was diagnosed with CA aneurysms caused by KD.
Sudden cardiac arrest may occur in the acute phase of KD during infancy or develop as a late sequela of this disease during adolescence and adulthood. The incidence of CA aneurysm can be reduced by five times through standard treatment of KD with lowered rate of sudden death to less than 0.1%[12,13]. Many asymptomatic adolescents or young adults may currently live with a CA aneurysm caused by undiagnosed KD or late KD treatment[14]. Serious cardiac events may occur in those who lack awareness of this late KD sequelae. Kazuma et al[15] reported that several sudden death cases in KD patients with left ventricular dysfunction suffered non-sustained ventricular tachycardia for 10 years before death. Few patients with a late sequela of KD could survive out-of-hospital cardiac arrest. In this case, the young adult survivor has normal left ventricular function, and arrhythmia was not observed in ECG monitoring during hospitalization. According to the medical history, clinical manifestation, and image examinations of this patient, the most likely cause of his sudden cardiac arrest in the presented case could be presumed as follows: Firstly, turbulent flow caused by local stenosis with intimal thickening forming a thrombus within the CA aneurysms; After that, a thromboembolism inducing extensive ischemia without infarction; And this ischemia-induced arrhythmia led to a cardiac arrest. In this case, timely CPR is the significant path for patient to survive from the sudden cardiac arrest.
Echocardiography is typically used to evaluate cardiac structure and function. Extensive calcification at the CA may induce an acoustic shadow. Meanwhile, coronary CTA imaging is helpful to detect calcified lesions. Sengupta et al[16] reported that CA aneurysms caused by KD lead to hemodynamic effects, where markedly abnormal flow patterns might lead to increasing risk of thrombosis and severe coronary events[16]. In this reported case, patient had normal atrial and ventricular size, wall thickness, and systolic and diastolic function in echocardiography examination. Coronary CTA revealed marked aneurysms and extensive calcifications in CA.
We reported a case of out-of-hospital cardiac arrest of a young adult survivor who probably had KD during childhood. Undiagnosed and untreated KD can have serious long-term sequelae. Few patients who suffer a late sequela of KD can survive from out-of-hospital cardiac arrest. Timely CPR is very critical for survival of sudden cardiac arrest. Meditations, surgical intervention, and active follow-up are extremely important for this patient to prevent adverse events from happening in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ajmal M, Ito S S-Editor: Zhang L L-Editor: Filipodia E-Editor: Qi LL
| 1. | Kawasaki T. [Acute febrile mucocutaneous syndrome with lymphoid involvement with specific desquamation of the fingers and toes in children]. Arerugi. 1967;16:178-222. [PubMed] |
| 2. | Kato H, Sugimura T, Akagi T, Sato N, Hashino K, Maeno Y, Kazue T, Eto G, Yamakawa R. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation. 1996;94:1379-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 923] [Cited by in RCA: 931] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 3. | Senzaki H. Long-term outcome of Kawasaki disease. Circulation. 2008;118:2763-2772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 81] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 4. | Jung JW. Long-Term Outcome of Kawasaki Disease Complicated by a Large Coronary Aneurysm. Korean Circ J. 2017;47:444-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Cohen P, O'Gara PT. Coronary artery aneurysms: a review of the natural history, pathophysiology, and management. Cardiol Rev. 2008;16:301-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 144] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 6. | Yajima D, Shimizu K, Oka K, Asari M, Maseda C, Okuda K, Shiono H, Ohtani S, Ogawa K. A Case of Sudden Infant Death Due to Incomplete Kawasaki Disease. J Forensic Sci. 2016;61 Suppl 1:S259-S264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Okura N, Okuda T, Shiotani S, Kohno M, Hayakawa H, Suzuki A, Kawasaki T. Sudden death as a late sequel of Kawasaki disease: postmortem CT demonstration of coronary artery aneurysm. Forensic Sci Int. 2013;225:85-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Singh S, Kawasaki T. Kawasaki Disease in India, Lessons Learnt Over the Last 20 Years. Indian Pediatr. 2016;53:119-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Brown TJ, Crawford SE, Cornwall ML, Garcia F, Shulman ST, Rowley AH. CD8 T lymphocytes and macrophages infiltrate coronary artery aneurysms in acute Kawasaki disease. J Infect Dis. 2001;184:940-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 203] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 10. | JCS Joint Working Group. Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2013). Digest version. Circ J. 2014;78:2521-2562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 180] [Article Influence: 16.4] [Reference Citation Analysis (0)] |
| 11. | Kaichi S, Tsuda E, Fujita H, Kurosaki K, Tanaka R, Naito H, Echigo S. Acute coronary artery dilation due to Kawasaki disease and subsequent late calcification as detected by electron beam computed tomography. Pediatr Cardiol. 2008;29:568-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Newburger JW, Takahashi M, Burns JC, Beiser AS, Chung KJ, Duffy CE, Glode MP, Mason WH, Reddy V, Sanders SP. The treatment of Kawasaki syndrome with intravenous gamma globulin. N Engl J Med. 1986;315:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1051] [Cited by in RCA: 964] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 13. | Nakamura Y, Aso E, Yashiro M, Uehara R, Watanabe M, Oki I, Yanagawa H. Mortality among persons with a history of kawasaki disease in Japan: mortality among males with cardiac sequelae is significantly higher than that of the general population. Circ J. 2008;72:134-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Tsuda E, Matsuo M, Naito H, Noguchi T, Nonogi H, Echigo S. Clinical features in adults with coronary arterial lesions caused by presumed Kawasaki disease. Cardiol Young. 2007;17:84-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Kazuma N, Tatara K, Murata M. Can heart rate variability predict sudden death? A case of sudden death in a child with severe coronary sequelae of Kawasaki disease. Pediatr Cardiol. 2000;21:403-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Sengupta D, Kahn AM, Burns JC, Sankaran S, Shadden SC, Marsden AL. Image-based modeling of hemodynamics in coronary artery aneurysms caused by Kawasaki disease. Biomech Model Mechanobiol. 2012;11:915-932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |