Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3562
Peer-review started: July 21, 2019
First decision: September 9, 2019
Revised: September 17, 2019
Accepted: September 25, 2019
Article in press: September 25, 2019
Published online: November 6, 2019
Processing time: 113 Days and 15.7 Hours
A recurrent valgus deformity was a common complication after total knee arthroplasty (TKA) in patients with valgus deformity. However, re-revision surgery for re-recurrent valgus deformity after revision TKA in patients with valgus deformity before primary TKA was uncommon.
We reported a 72-year-old female patient with two recurrent valgus deformities after TKA for a valgus knee deformity who underwent two revision surgeries to rectify the deformity. In the re-revision surgery, bone defects were successfully reconstructed by the augments and cement in combination with screws and a sleeve. An appropriate neutral alignment of the lower limb was restored by the perfect femoral entry point and the long diaphyseal cementless stem. Adequate fixation of the metaphysis and diaphysis of the femur was obtained by the sleeve and long diaphyseal cementless stem. The patient was pain-free and deformity-free for 2.5 years.
The management of bone defects, the choice of the stem and the femoral entry point were of vital importance in the revision or re-revision TKA for a recurrent valgus deformity.
Core tip: Recurrent valgus deformity was a complication of total knee arthroplasty (TKA) in patients with a severe valgus deformity. It is very difficult to perform the revision TKA. The management of bone defects, the choice of the stem and the femoral entry point were of vital importance in the revision TKA.
- Citation: Du YQ, Sun JY, Ni M, Zhou YG. Re-revision surgery for re-recurrent valgus deformity after revision total knee arthroplasty in a patient with a severe valgus deformity: A case report. World J Clin Cases 2019; 7(21): 3562-3568
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3562.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3562
For more than a decade, the number of total knee arthroplasties (TKAs) had been steadily increasing with the increased demand for rectifying deformities and alleviating pain[1,2]. However, TKA with valgus deformity was considered a surgical challenge, and the incidence of recurrent valgus deformities was very high[3]. The revision surgery for failed TKAs became unusually complex because of the presence of tremendous bone defects of the lateral femoral condyle. While the development of highly porous cones and sleeves has enabled the reconstruction of areas with massive metaphyseal bone defects and the improvement of solid fixations[4-6], the fixation of the diaphyseal stem was also crucial for revision TKA success. The extension of the stem was important in transferring the bending and torsional stresses generated by articulation of the joint away from the joint surface toward the strong diaphyseal bone[7]. The length of the diaphyseal stem and the entry point of the femoral intramedullary (IM) rod were the cornerstones of achieving perfect lower limb alignment. Therefore, the management of bone defects, the choice of the stem and the femoral entry point were of vital importance in revision TKA for recurrent valgus deformity. Here, we report a patient with a rare, severe valgus deformity who underwent two revision surgeries for recurrent valgus deformity after TKA.
A 72-year-old female patient visited our hospital 6 years after revision surgery for left TKA with a chief complaint of pain, and the pain worsened for 1 mo.
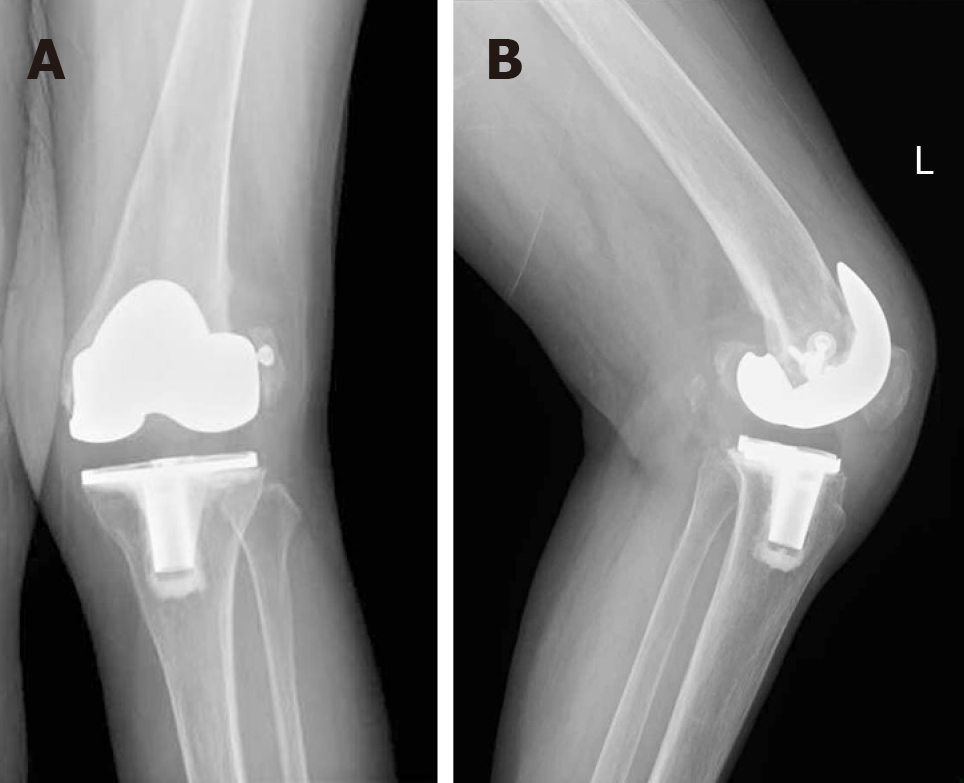
The patient underwent left primary TKA (NexGen LPS-FLEX, Zimmer, Warsaw, Indiana, United States) and sliding osteotomy of the lateral femur condyle in 2008 for a severe valgus deformity at another institution. Six months later, she again presented with valgus deformity and pain in the left knee. In-house X-rays revealed notable femoral component loosening and recurrent valgus deformity (Figure 1).
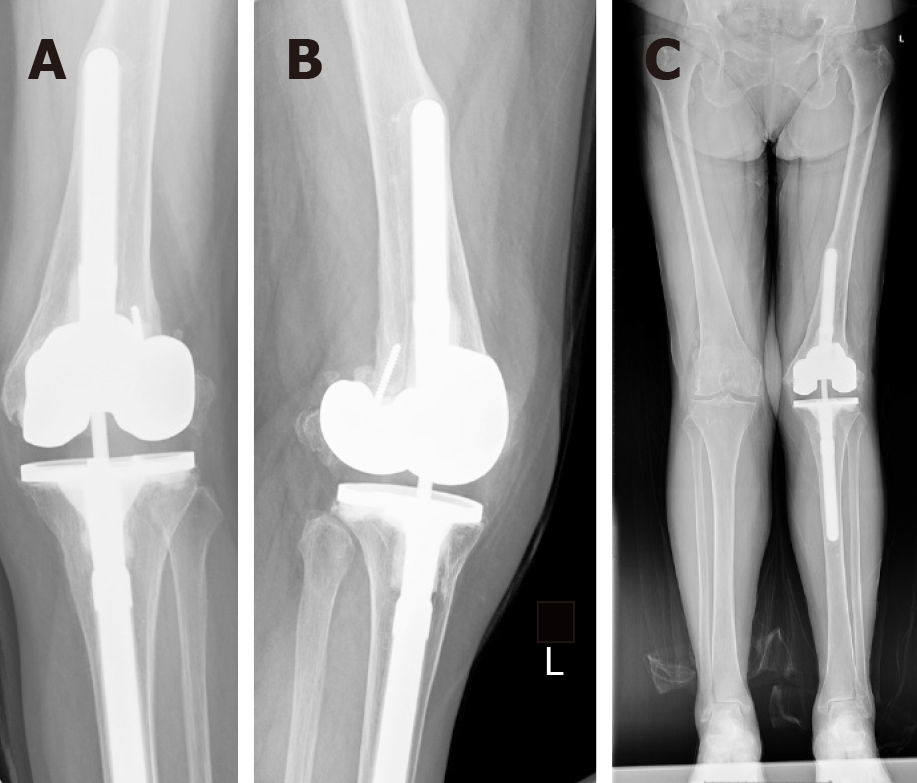
Then, the revision of the knee components was performed in 2010 at another institution. The system that the surgeon used was the press fit condylar, Sigma, total condylar III (TC3) system (DePuy, Warsaw, Indiana, United States). All the stems on the femoral and tibial sides were cementless, and the cement that was reinforced with screws was used to reconstruct the defects of the lateral femoral condyle (Figure 2). The patient did not report any serious symptoms for six years. In 2016, she started complaining of knee pain again, and she showed limited movement and valgus deformity.
She suffered from hypertension for 2 years. Her blood pressure was controlled by using antihypertensive drugs.
The patient did not have any specific personal or family history of disease.
We evaluated her before re-revision TKA. In the clinical examination, the knee was equally painful with weight-bearing and passive motions. The range of motion was from 5° to 80° of flexion. There was anterior-posterior laxity of 5-10 mm. With valgus stress, there was a marked medial instability of more than 15°.
The patient was evaluated to rule out infection. The knee was aspirated preoperatively. The synovial red blood cell count was 13-18/HPF, and the synovial white blood cell count, polymorphonuclear (%) and leukocyte esterase were normal. There was no bacterial growth in the aspirate. Likewise, the serum C-reactive protein, erythrocyte sedimentation rate and interleukin 6 were normal. An emission computed tomography scan of the bone in the whole body was also found to be negative for infection.
In 2016, X-rays showed loosening of the femoral component and the stem (Figure 3).
The final diagnosis included loosening of the components and stem of the femoral side and recurrent valgus deformity in the left knee.
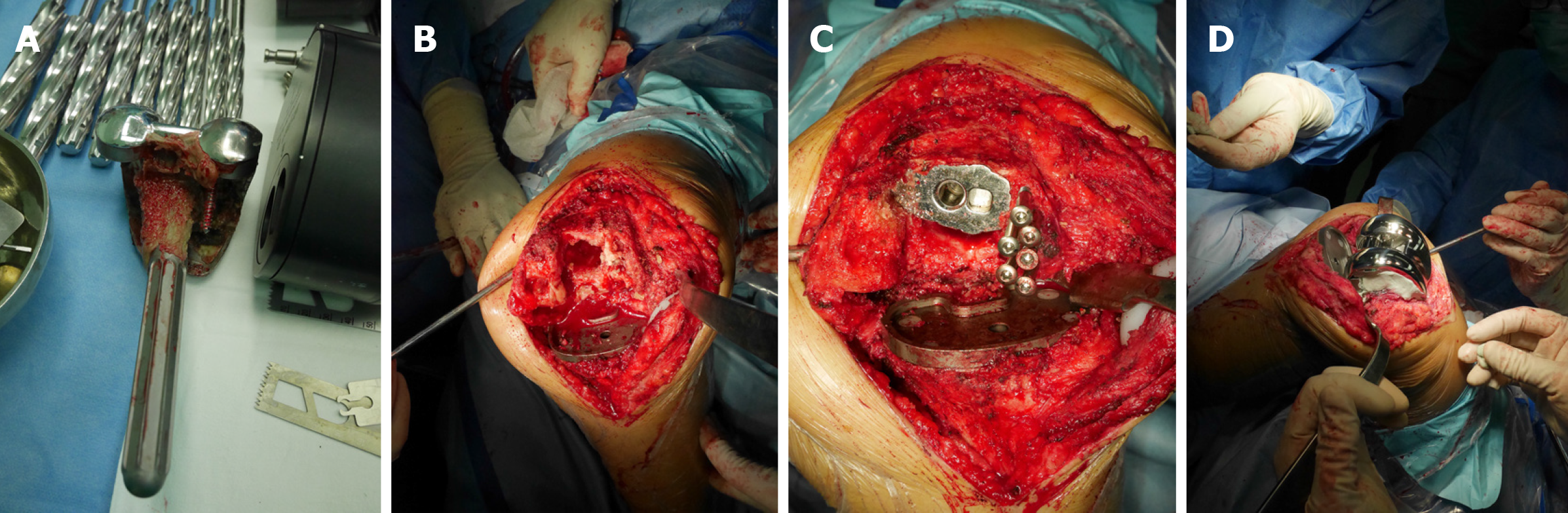
During surgery, the medial joint space opened widely with valgus stress during flexion and extension. The quadriceps snip technique was used to assist in the surgical exposure of the knee. The components and stem of the femoral side were loosened, and those of the tibial side were well stabilized. After removal of the loose femoral component and stem, we evaluated the intraoperative bone defects (type FIIB) according to the Anderson Orthopaedic Research Institute (AORI) classification (AORI classification of bone defects in revision TKA)[8]. The cement reinforced with screws was used to reconstruct the defects of the lateral femoral condyle. A lateral distal femoral block augment (4 mm thick) and posterior femoral augments (the medial and lateral sides were 4 mm and 8 mm thick, respectively) were used to restore the defects of the joint surface and epiphysis. A porous titanium metaphyseal sleeve (size: 40 mm) was used in the treatment of metaphyseal bone defects. A TC3 femoral component (size: 4) in combination with a cementless stem (size: 16 mm × 115 mm), which was engaged in the cortical bone of diaphysis, was implanted with a hybrid fixation. Then, a new constrained polyethylene liner (17.5 mm) was placed in the tibial component plate (Figure 4).
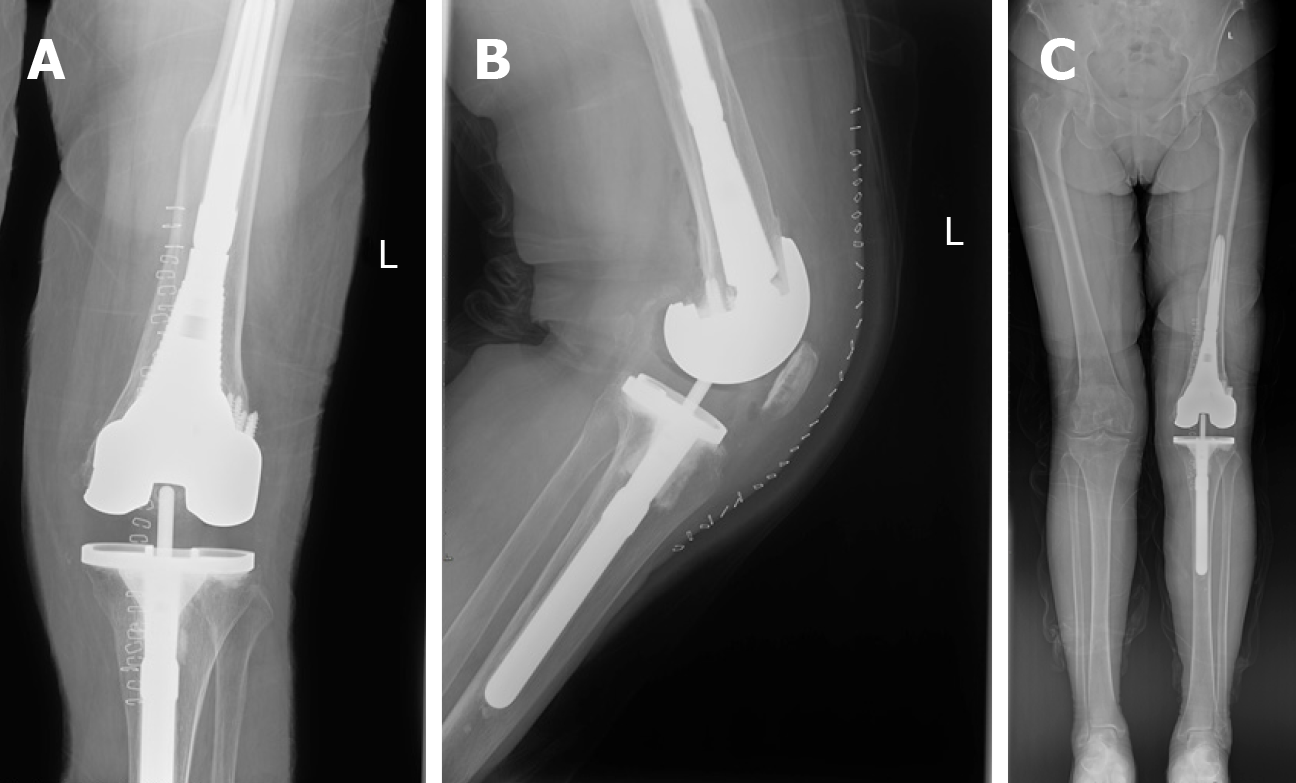
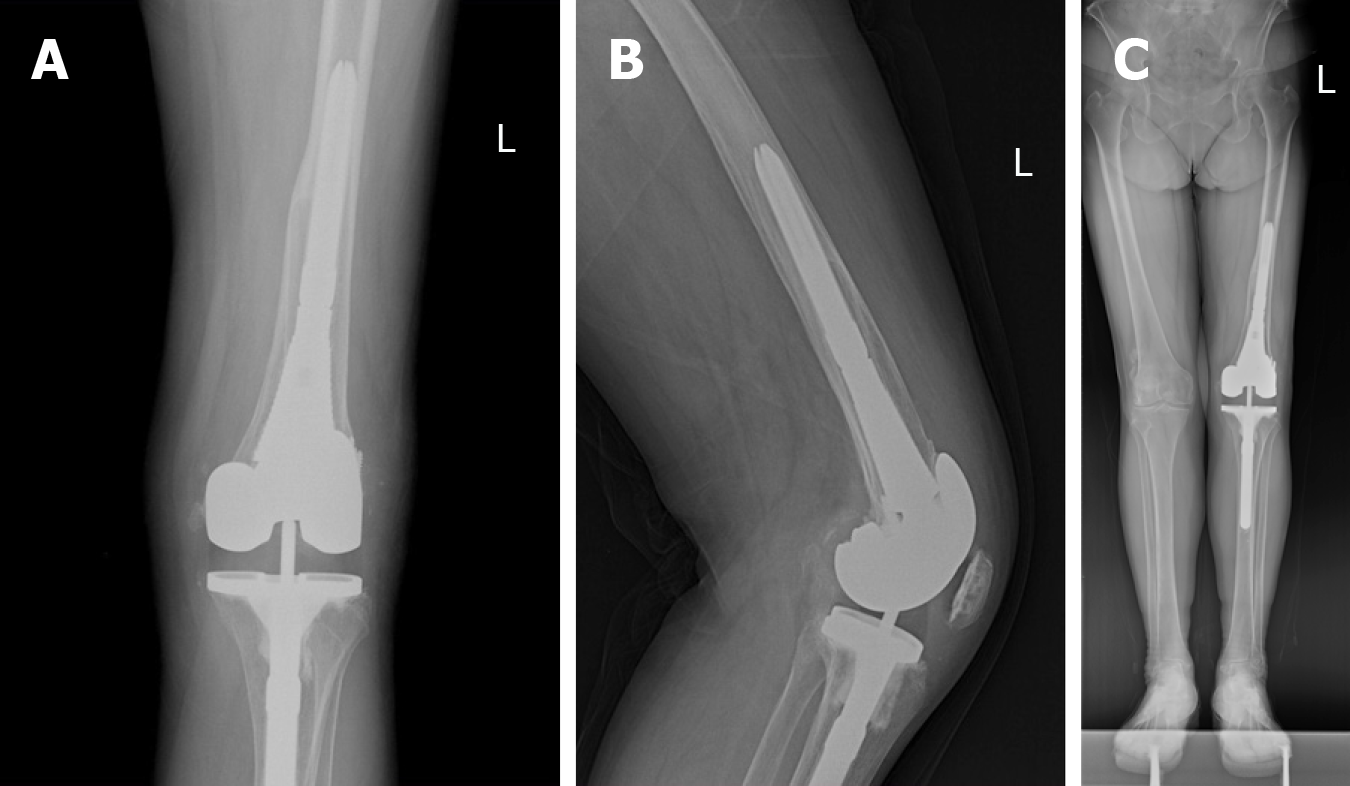
Postoperative X-rays confirmed excellent placement of the components after left TKA (Figure 5). Continuous passive motions and partial weight-bearing actions with a walking aid were initiated on the second postoperative day, and the range of motion was gradually increased to 0°-90° of flexion. The patient had no postoperative complications and was discharged from the hospital on postoperative day 4. Physical therapy stressed a gentle range of motion and strengthening exercise with no forced flexion. Four weeks after surgery, she gradually resumed full weight-bearing activities.
Following this surgery, the patient made an eventful recovery, and 2.5 years have now passed after the re-revision TKA. She was satisfied with her knee, with a hospital for special surgery score of 84 (preoperative score: 31), was pain-free, and had a range of motion of 0°-100° of flexion. The X-rays showed that the left knee arthroplasty was in the expected position with no radiographic signs of loosening (Figure 6).
We presented an experience with a 72-year-old female patient with two recurrent valgus deformities after TKA for a valgus knee deformity. The patient underwent two revision surgeries because of the recurrent valgus deformity.
A primary TKA for a valgus knee deformity represented a challenge for orthopaedic surgeons, especially beginners[9,10]. Nikolopoulos et al[9] presented in his review article several complications that have been reported more frequently in patients with a valgus knee deformity who underwent TKA, and the incidence of recurrent valgus deformity ranged from 4% to 38%. A recurrent valgus deformity could result in massive bone defects of the lateral femoral condyle. For large or uncontained defects, including AORI type II, treatment alternatives include modular augments, the cement reinforced with screws and porous titanium metaphyseal sleeve. Distal and posterior femoral defects managed with modular augments allow for the placement of well-positioned and correctly sized femoral components in contact with host bone[11], and posterior femoral augments are particularly useful in restoring the proper anteroposterior dimension of the component, achieving the correct rotation of the femoral component and addressing the extension-flexion mismatch by altering the flexion gap[12]. Porous titanium metaphyseal sleeves with a stepped shape and titanium bead coating were easy to use for fixation by bone ingrowth and were available to fill the metaphyseal defects. The femoral component was attached to the sleeve through the Morse junction on the instrument[13]. Although many authors recommended the use of cement in combination with screws in cases of contained or uncontained defects between 5 mm and 10 mm, we still used the cement to reconstruct the massive defects of the lateral femoral condyle. According to zonal fixation concepts, solid fixation should be achieved in at least two of three zones[14]. The cementless stem and metaphyseal sleeve at least helped in promoting an additional fixation in the metaphysis (zone 2) and diaphysis (zone 3) of femur, so the cement in combination with screws was safe to use to reconstruct the lateral femoral condyle.
We analysed the causes of failure of the revision TKA and considered the invalid entry point of the femoral IM rod and the short cementless stem as the main causes.
According to the postoperative X-rays after revision TKA, the entry point of the femoral IM rod was located at the centre of the coronal plane and posterior to the centre of the femoral marrow cavity in the sagittal plane, which resulted in residual valgus deformity, gross flexion-extension mismatch and loading stresses on the lateral femoral condyle and ultimately led to the failure of the reconstruction of the lateral femoral condyle. Tan et al[15] suggested that the femoral entry point should be located medial to the centre of the knee joint in the coronal plane for a valgus knee arthroplasty. In the re-revision surgery, we adjusted the entry point of the femoral IM rod to be medial of the centre of the joint in the coronal plane (the intersection of the anatomical axis and the distal femoral joint line) and in the centre of the femoral marrow cavity in the sagittal plane, restoring the neutral alignment of the lower limb.
While augments and sleeves greatly enhanced the modern surgeon’s ability to gain solid fixation in metaphyseal bone, stems continue to be useful in revision TKA to bypass defects and enhance the structural stability of revision components[16]. In revision surgery, the surgeon chose a cementless stem to bypass the metaphyseal defect. However, the stem was too short and thin to achieve solid fixation in the diaphysis (zone 3) of the femur. In the re-revision surgery, we used a long diaphyseal cementless stem, which engaged in the cortical bone of diaphysis, to transfer loads to the diaphysis and reduce micromotions. The long diaphyseal cementless stem not only assisted in offloading interface stresses but also guided the IM rod to prevent malalignment[17,18].
When the joint surface and epiphysis (zone 1) were inadequate, fixation of the metaphysis (zone 2) and diaphysis (zone 3) of the femur became particularly important. In this case, the insufficient fixation of the metaphysis and diaphysis were reasons the revision TKA failed. The invalid entry point of the femoral IM rod and the short cementless stem, which led to lower limb malalignment, were major causes of failure and re-revision surgery.
Recurrent valgus deformity was the most commonly reported complication after TKA for a valgus knee deformity, leading to massive bone defects of the lateral femoral condyle. The restoration of bone defects, component stability and perfect lower limb alignment were the main challenges in the revision or re-revision TKA. Bone defects were successfully reconstructed by the augments, the cement in combination with screws and the sleeve. An appropriate neutral alignment of the lower limb was restored by the perfect entry point of the femoral IM rod and the long diaphyseal cementless stem. Adequate fixation of the metaphysis and diaphysis of the femur was obtained by the sleeve and the long diaphyseal cementless stem. All these factors were the cornerstones of the success of this case.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ünver B S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Qi LL
| 1. | Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780-785. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2079] [Cited by in RCA: 3251] [Article Influence: 180.6] [Reference Citation Analysis (0)] |
| 2. | Patel A, Pavlou G, Mújica-Mota RE, Toms AD. The epidemiology of revision total knee and hip arthroplasty in England and Wales: a comparative analysis with projections for the United States. A study using the National Joint Registry dataset. Bone Joint J. 2015;97-B:1076-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 397] [Article Influence: 39.7] [Reference Citation Analysis (0)] |
| 3. | Rossi R, Rosso F, Cottino U, Dettoni F, Bonasia DE, Bruzzone M. Total knee arthroplasty in the valgus knee. Int Orthop. 2014;38:273-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 107] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 4. | Thorsell M, Hedström M, Wick MC, Weiss RJ. Good clinical and radiographic outcome of cementless metal metaphyseal sleeves in total knee arthroplasty. Acta Orthop. 2018;89:84-88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Sandiford NA, Misur P, Garbuz DS, Greidanus NV, Masri BA. No Difference Between Trabecular Metal Cones and Femoral Head Allografts in Revision TKA: Minimum 5-year Followup. Clin Orthop Relat Res. 2017;475:118-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Sheth NP, Bonadio MB, Demange MK. Bone Loss in Revision Total Knee Arthroplasty: Evaluation and Management. J Am Acad Orthop Surg. 2017;25:348-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 70] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 7. | Completo A, Simões JA, Fonseca F. Revision total knee arthroplasty: the influence of femoral stems in load sharing and stability. Knee. 2009;16:275-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Engh GA, Ammeen DJ. Classification and preoperative radiographic evaluation: knee. Orthop Clin North Am. 1998;29:205-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 92] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Nikolopoulos D, Michos I, Safos G, Safos P. Current surgical strategies for total arthroplasty in valgus knee. World J Orthop. 2015;6:469-482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Favorito PJ, Mihalko WM, Krackow KA. Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg. 2002;10:16-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Sculco PK, Abdel MP, Hanssen AD, Lewallen DG. The management of bone loss in revision total knee arthroplasty: rebuild, reinforce, and augment. Bone Joint J. 2016;98-B:120-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 78] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 12. | Vasso M, Beaufils P, Cerciello S, Schiavone Panni A. Bone loss following knee arthroplasty: potential treatment options. Arch Orthop Trauma Surg. 2014;134:543-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 33] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Agarwal S, Neogi DS, Morgan-Jones R. Metaphyseal sleeves in revision total knee arthroplasty: Minimum seven-year follow-up study. Knee. 2018;25:1299-1307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 14. | Morgan-Jones R, Oussedik SI, Graichen H, Haddad FS. Zonal fixation in revision total knee arthroplasty. Bone Joint J. 2015;97-B:147-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 190] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 15. | Tan H, Wang Y, Long T, Nie B, Mao Z, Yue B. How to accurately determine the distal femoral valgus cut angle in the valgus knee arthroplasty. Int Orthop. 2018;42:537-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Driesman AS, Macaulay W, Schwarzkopf R. Cemented versus Cementless Stems in Revision Total Knee Arthroplasty. J Knee Surg. 2019;32:704-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Mancuso F, Beltrame A, Colombo E, Miani E, Bassini F. Management of metaphyseal bone loss in revision knee arthroplasty. Acta Biomed. 2017;88:98-111. [PubMed] |
| 18. | Huten D. Femorotibial bone loss during revision total knee arthroplasty. Orthop Traumatol Surg Res. 2013;99:S22-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 48] [Article Influence: 4.0] [Reference Citation Analysis (0)] |