Published online Nov 6, 2019. doi: 10.12998/wjcc.v7.i21.3535
Peer-review started: March 11, 2019
First decision: April 18, 2019
Revised: May 15, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: November 6, 2019
Processing time: 245 Days and 12 Hours
Carbapenem-resistant Enterobacteriaceae has become a significant public health concern as hospital outbreaks are now being frequently reported and these organisms are becoming difficult to treat with the available antibiotics.
An outbreak of VIM-producing Serratia marcescens occurred over a period of 11 wk (August, 1 to October, 18) in patients admitted to the adult polyvalent intensive care unit of the University of Campania “Luigi Vanvitelli” located in Naples. Four episodes occurred in three patients (two patients infected, and one patient colonized). All the strains revealed the production of VIM.
After three decades of carbapenem antibiotics use, the emergence of carbapenem-resistance in Enterobacteriaceae has become a significant concern and a stricter control to preserve its clinical application is mandatory. This is, to our knowledge, the first outbreak of VIM-producing Serratia marcescens in Europe. Surveillance policies must be implemented to avoid future outbreaks.
Core Tip: An outbreak of VIM-producing Serratia marcescens occurred in patients admitted to the adult polyvalent intensive care unit of the University of Campania “Luigi Vanvitelli” located in Naples. All the strains revealed the production of VIM. After three decades of carbapenem antibiotics use, the emergence of carbapenem-resistant Enterobacteriaceae has become a significant concern and is mandatory a stricter control to preserve its clinical application. This is, to our knowledge, the first outbreak of VIM-producing Serratia marcescens occurred in a European hospital.
- Citation: Iovene MR, Pota V, Galdiero M, Corvino G, Di Lella FM, Stelitano D, Passavanti MB, Pace MC, Alfieri A, Di Franco S, Aurilio C, Sansone P, Niyas VKM, Fiore M. First Italian outbreak of VIM-producing Serratia marcescens in an adult polyvalent intensive care unit, August-October 2018: A case report and literature review. World J Clin Cases 2019; 7(21): 3535-3548
- URL: https://www.wjgnet.com/2307-8960/full/v7/i21/3535.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i21.3535
Carbapenem-resistant Enterobacteriaceae (CRE) has become a significant public health concern as hospital outbreaks are now being frequently reported and these organisms are becoming difficult to treat with the available antibiotics. Early recognition through molecular characterization, epidemiologic studies, and surveillance is essential to prevent hospital outbreaks of these organisms[1]. Serratia marcescens (S. marcescens), an aerobic Gram-negative pathogen belonging to the family of Enterobacteriaceae, is known to cause hospital-acquired infections, commonly in an outbreak setting. Carbapenem resistance in S. marcescens may be chromosomal (SME), or plasmid (KPC, Oxa-48, IMP, NDM and VIM) mediated. Carbapenem resistance in is an ominous event as this pathogen is intrinsically resistant to polymyxins[2]. S. marcescens outbreaks in intensive care units (ICUs) are associated with considerable mortality rates, ranging from 14% to 60%[3,4]. Previous S. marcescens outbreaks in Italy has been mostly reported in neonatal ICUs (NICUs)[5-9]. The present study aimed to describe the first Italian nosocomial outbreak of VIM-producing S. marcescens occurred in our adult polyvalent ICU located in Campania region, Southern Italy.
The index case of the outbreak of three patients infected and/or colonized by VIM-producing S. marcescens was a 49-year-old man with a history of schizophrenia admitted with a diagnosis of descending necrotizing mediastinitis whose CRE screening at admission was negative.
The second patient was a 69-year-old woman with a history of recurrent episodes of urinary tract infection (UTI) admitted from the community with UTI and septic shock (SS).
The third patient was a 67-year-old woman with various underlying diseases (Paranoid personality disorder, diabetes mellitus, ulcerative colitis, hypothyroidism and hypertrophic cardiomyopathy) who was admitted to our ICU for a hypovolemic haemorrhagic shock.
For every patient admitted to our six-bed adult polyvalent ICU, a rectal swab (RS) was obtained (CRE screening) using a Copan Amies sterile transport swab (Copan Diagnostics, Murrieta, CA). The RS was streaked onto Mac Conkey Agar (Biomerieux, Marcy l'Etoule, France) with a 10 μg meropenem disk. Mac Conkey agar plates were incubated aerobically at 37°C overnight. Antibiotic susceptibility was determined using the disk diffusion method. Suspicious colonies growing into the meropenem disk-halo were picked up and identified using MALDI-TOF MS (Matrix- Assisted Laser Desorption/Ionization Time of Flight mass spectroscopy).
Carbapenem resistance were identified in accordance with the European Committee on Antimicrobial Susceptibility Testing (EUCAST) guidelines using updated EUCAST breakpoint tables (EUCAST clinical breakpoint valid from 15/05/2018) (Table 1).
| MIC (μg/mL) | ||||
| AMK | ≤ 4 | 8 | ≤ 4 | ≤ 4 |
| AMC | > 32/2 | > 32/2 | > 32/2 | > 32/2 |
| AMP | > 8 | > 8 | > 8 | > 8 |
| FEP | > 8 | > 8 | > 8 | > 8 |
| CTX | > 4 | > 4 | > 4 | > 4 |
| CAZ | > 8 | > 8 | > 8 | > 8 |
| CIP | 1 | > 1 | 0.5 | 0.5 |
| CST | > 4 | > 4 | ≤ 1 | ≤ 1 |
| ETP | > 1 | > 1 | > 1 | > 1 |
| FOF | ≤ 32 | 64 | ≤ 32 | ≤ 32 |
| GEN | > 4 | > 4 | 4 | 4 |
| IPM | > 8 | > 8 | > 8 | > 8 |
| LVX | 2 | > 2 | 1 | ≤ 0.5 |
| MEM | > 8 | > 8 | > 8 | 8 |
| PIP | > 16 | > 16 | > 16 | > 16 |
| TZP | > 16/4 | > 16/4 | > 16/4 | > 16/4 |
| TGC | > 2 | > 2 | > 2 | > 2 |
| TOB | > 4 | > 4 | > 4 | > 4 |
| SXT | > 4/76 | > 4/76 | > 4/76 | > 4/76 |
| Date | Aug, 1 | Aug, 17 | Sep, 20 | Sep, 24 |
| Site | Blood | Blood | RS | RT |
Molecular analysis to identify carbapenemase genes was performed using the Xpert Carba-R Cartridge (GeneXpert®, Cepheid, Sunnyvale, CA).
The Xpert Carba-R Assay, conducted on the GeneXpert® device, is an automated qualitative real-time polymerase chain reaction based test that detects specific gene associated with carbapenem resistance(blaKPC , blaNDM, blaVIM, blaOXA-48 and blaIMP-1).
After 65 d of the first patient hospitalization, a blood culture grew VIM-producing S. marcescens. Three days after the diagnosis of bacteraemia his RS was positive for the same organism. The same patient developed a new episode of bacteraemia during further ICU stay.
The second patient, eleven days after admission in ICU, developed lower respiratory tract infection (LRTI) with bronchial culture positive for VIM-producing S. marcescens. Her RS also tested positive for S. marcescens on the same day.
VIM-producing S. marcescens was isolated in the third patient from tracheal aspirate after seven days and from urine after eleven days of hospitalization. In both cases, the isolated was considered as a contaminant. During the ICU admission she developed an acute respiratory distress syndrome due to Enterococcus faecium.
The first episode of VIM-producing S. marcescens bacteraemia was treated with ceftazidime-avibactam (CZA) plus gentamicin for 14-d. The second episode was initially treated with amikacin (AMK) and Fosfomycin. Fosfomycin was later substituted with meropenem due to hypernatremia. The total duration of the antibiotic treatment in this episode was 47 d.
The second patient was treated by the ward of origin with piperacillin-tazobactam (TZP) in association with AMK; initially (September, 12) we treated the SS with ceftolozane-tazobactam (C/T) and metronidazole; ceftaroline, not active against VIM-producing S. marcescens, was added later (September, 24), as her condition deteriorated, for a suspected methicillin-resistant Staphylococcus aureus infection[10]. The duration of total antibiotic therapy was 14 d.
The third patient was initially empirically treated with tigecycline and TZP; subsequently, due to the worsening of clinical conditions, antibiotic therapy was modified with the introduction of CZA, AMK, Colistin and ampicillin-sulbactam. VIM-producing S. marcescens, considered as a contaminant, in the third patient was not treated.
Both episodes of bacteraemia of the first patient resulted in a favourable outcome: The patient was transferred to a rehabilitation unit at the end of the ICU stay.
The second and the third patient died. Unfortunately for the third patient the microbiological result, with the isolation of the Enterococcus faecium, arrived posthumously.
The main clinical and epidemiological characteristics of the patients are reported in Table 2.
| Patient | Admission from | Age(yr) | Sex | Underlying disease(s) | Previous AT | Admission diagnosis | Date of admission | Stool screening | 1° site of identifi-cation |
| 1 | Community | 49 | M | SC | No | DNM | May, 28 | Yes | Blood |
| 1 | ICU | 49 | M | SC | Yes | DNM | May, 28 | Yes | Blood |
| 2 | Community | 69 | F | rUTI | Yes | SS | Sep, 9 | Yes | RS |
| 3 | Internal ward | 67 | F | PPD, DM, UC, SHT, HCM | Yes | HS | Sep, 17 | Yes | RT |
| Patient | Infection (1° site) | Date of 1° isolation | 2° site of identification | Infection (2° site) | Date of the 2° isolation site | Initial AT | Final AT | AT duration(d) | Outcome |
| 1 | Yes | Aug, 1 | RS | No | Aug, 4 | CZA + GEN | CZA + GEN | 14 | Favourable |
| 1 | Yes | Aug, 17 | - | - | - | AMK + FOF | AMK + MEM | 47 | Favourable |
| 2 | No | Sep, 20 | RT | Yes | Sep, 20 | C/T + MTZ | C/T + MTZ + CPT | 14 | Death |
| 3 | No | Sep, 24 | Urine | No | Sep, 28 | AFG + TGC + TZP | CST + SAM + CZA + AMK + AFG | 16 | Death |
S. marcescens is an essential cause of hospital-acquired infections. Although most infections have been linked to hospital outbreaks, occasional infections can occur outside the outbreak settings also. The first hospital outbreak was reported in San Francisco in 1950 where 11 patients developed UTI by S. marcescens, one of them complicated by endocarditis[11]. Many hospital outbreaks have been reported after that[12]. It has been associated with various infections including UTI, bloodstream infection, pneumonia, skin and soft tissue infections, meningitis and ocular infections.
Antibiotic resistance has been a worrisome issue to physicians treating infections caused by S. marcescens. This organism is intrinsically resistant to a large number of antibiotics including ampicillin, amoxicillin, amoxicillin-clavulanate, ampicillin-sulbactam, narrow-spectrum cephalosporins, cefuroxime, nitrofurantoin, macrolides and polymixins[13]. It also carries a chromosomal AmpC beta-lactamase which when overexpressed can render all beta-lactams except carbapenems ineffective[14]. They also can produce plasmid-mediated extended spectrum beta-lactamase (ESBL) and carbapenemases. Carbapenemases in S. marcescens can be chromosomal (SME) or plasmid-mediated (KPC, OXA-48, IMP, VIM, and NDM). Quinolone resistance can arise due to alterations in gyrA, outer membrane proteins, and expression of efflux pumps[12].
Carbapenem resistance can be devastating in case of Serratia infections considering its intrinsic resistance to polymixins. Many outbreaks of KPC2 producing Serratia marcescens has been reported[15,16]. Plasmid-mediated Metallo-β-lactamases (IMP, VIM, and NDM-1) which inactivate carbapenems can be produced by some Serratia strains[17].
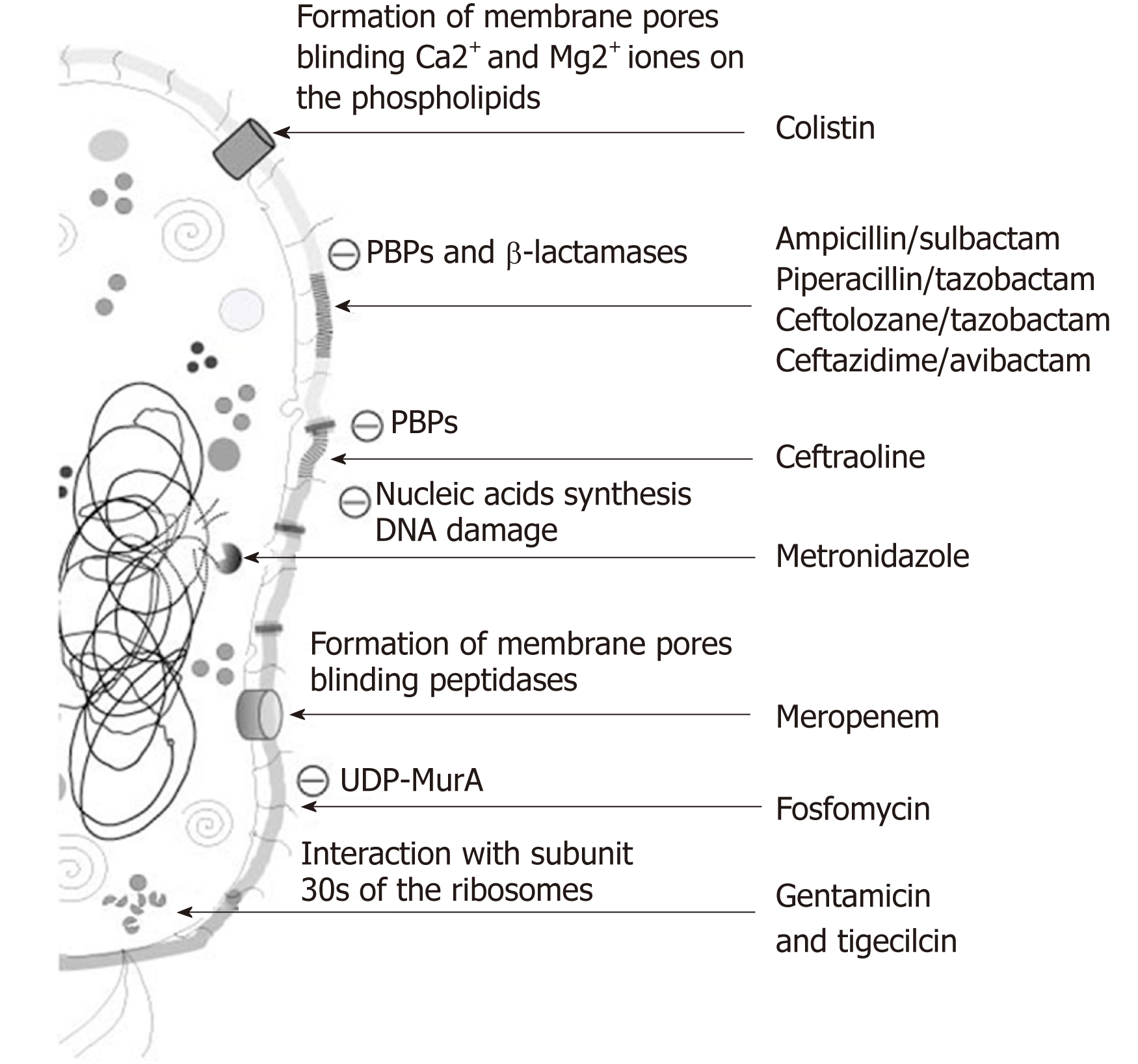
Nosocomial outbreaks of VIM-producing S. marcescens has been reported infrequently in literature, most of them are from NICUs[18,19]. Nosocomial outbreaks of VIM-producing pathogens have been reported in multiple major Gram-negative bacteria, making VIM-producing bacteria a severe public health concern. The first VIM-producing Gram-negative pathogen and the most frequently reported in the literature is Pseudomonas aeruginosa, followed by Klebsiella pneumonia and Acinetobacter baumannii (Table 3). In our study, VIM-producing S. marcescens was isolated in a University Hospital ICU. This is in line with previous reports in the literature because most cases of VIM-producing Gram-negative pathogens have been isolated in ICUs of tertiary care teaching hospitals (Table 3). Unlike what has been reported in the last ten years in our Country, where the S. marcescens outbreaks have mostly taken place in NICUs (Table 4) this first Italian outbreak of VIM-producing Serratia marcescens occurred in an adult ICU. Fatality rate in our outbreak was 50% (2 of 4 episodes), similar to the first nosocomial outbreak of VIM-producing S. marcescens happened in Argentina, which however occurred in NICU setting[19]. The high mortality is probably due to the inappropriate use of antibiotics for the treatment of severe infections in ICU patients[20]. In Figure 1 are represented the mechanisms of action of antibiotics used in our patients with VIM-producing S. marcescens infection. Given that no effective treatment is known, isolated reports describe successful therapy combining CZA and Aztreonam. The rationale of this antibiotic association is that Aztreonam remains intact in the presence of carbapenemases but hydrolyzed by ESBLs and CZA neutralizes the ESBLs and AmpC beta-lactamases[21]. In our study CZA was never co-administered with aztreonam, though there was clinical success in one of two patients who were given CZA in combination with other antibiotics (Table 2).
| Year | City, Country, time span | Pathogen | Type of Hospital | Setting | VIM cases | Comments |
| 2000 | Verona, Italy; February 1997 - February 1998[29] | Pseudomonas aeruginosa | University Hospital | ICU patients | 83 | All patients from ICU |
| 2000 | Thessaloniki, Greece; 1996-1998[30] | Pseudomonas aeruginosa | University Hospital | ICU patients | 211 | More than one sample for patient; |
| 2001 | Southern Taiwan; January 1999 - December 2000[31] | Klebsiella pneumoniae | University Medical Center | ICU and Other Wards | 5 | Multidrug-resistant Klebsiella pneumoniae |
| 2004 | Heraklion, Greece; Summer 2001[32] | Escherichia coli | University Hospital | ICU patients | 4 | All patients from ICU |
| 2004 | Cali, Colombia; February 1999 - July 2003[33] | Pseudomonas aeruginosa | Tertiary Care Medical Center | ICU patients | 66 | All patients from ICU |
| 2005 | Larissa and Thessaloniki, Greece; December 2004 - March 2005[34] | Klebsiella pneumoniae | University Hospital | ICU and Other Wards | 27 | Outbreaks in distinct regions due to a single Klebsiella pneumoniae clone |
| 2005 | Calgary, Canada; May 2002 - April 2004[35] | Pseudomonas aeruginosa | 1 pediatric and 3 large adult hospitals | ICU and Other Wards | 228 | Population-based epidemiological study of infections |
| 2005 | USA; May 2013[36] | Pseudomonas aeruginosa | Public Teaching Hospital | ICU and Other Wards | 17 | First outbreak of carbapenemase in USA |
| 2005 | Porto Alegre, southern Brazil; January - October 2004[37] | Pseudomonas aeruginosa | Tertiary-care Teaching Hospital | ICU and Other Wards | 135 | Outbreak of carbapenem-resistant |
| 2006 | Athens, Greece; March 2002-October 2002[38] | Acinetobacter baumannii | Tertiary Care Hospital | ICU and Other Wards | 15 | Outbreak of multiple clones of imipenem-resistant |
| 2006 | Paris, France; 2003-2004[39] | Klebsiella pneumoniae | Teaching Hospital | ICU and Other Wards | 8 | Recovered from clinical specimens or rectal swabs - Surgical ward or ICU patients |
| 2006 | Trieste, Italy; 1996-1997/ 2000-2002[40] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 91 | Nosocomial setting of high-level endemicity |
| 2006 | Hungary; October 2003-November 2005[41] | Pseudomonas aeruginosa | seven hospitals in Hungary | ICU and Other Wards | 19 | Molecular epidemiology of VIM-4 Pseudomonas sp |
| 2007 | Madrid, Spain; March 2005 - September 2006[42] | Enterobacteriaceae | University Hospital | ICU and Other Wards | 25 | (52% of patients were in ICU) |
| 2007 | Warsaw, Poland ; September 2003 - May2004/July 2005-January2006[43] | Pseudomonas aeruginosa | Tertiary Care Hospital | ICU and Other Wards | 41 | Outbreak of Pseudomonas aeruginosa infections |
| 2007 | Athens, Greece; 14 September -3 October 2005[44] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 5 | Ventilator-Associated Pneumonia (VAP) |
| 2008 | Serres, Greece; April 2005 - March 2007[45] | Acinetobacter baumanni | General Hospital | ICU patients | 31 | All patients from ICU |
| 2008 | Piraeus, Greece; 2005-2006[46] | Acinetobacter baumannii | General Hospital | ICU and Other Wards | 6 | 4 ICU patients |
| 2008 | Genoa, Italy; September 2004 - March 2005[47] | Klebsiella pneumoniae | Tertiary Care Hospital | ICU and Other Wards | 9 | Bloodstream infections |
| 2008 | Athens, Greece; February 2004 - March 2006[48] | Klebsiella pneumoniae | three hospitals in Athens | ICU and Other Wards | 67 | 77% ICU patients |
| 2008 | Thessaloniki, Greece; November 2006 - April 2007[49] | Klebsiella pneumoniae | Tertiary Care Hospital | Wards | 9 | Patients hospitalized in different medical and surgical wards |
| 2008 | Nantes, France; April 1996 - July 2004[50] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 59 | Mostly urinary tract infections and pneumonia |
| 2008 | UK; November 2003-November 2007[51] | Pseudomonas aeruginosa | 12 UK Hospital | ICU patients | 32 | 15 cases from same hospital |
| 2009 | Greece; February 2008 - December 2008[52] | Klebsiella pneumoniae | 21 Greek hospitals | ICU patients | 52 | All patients from ICU |
| 2009 | Thessaloniki, Greece; November 2004 - December 2005[53] | Pseudomonas aeruginosa | University Hospital | ICU patients | 29 | All patients from ICU |
| 2010 | Zonguldak, Turkey; 2003–2006[54] | Acinetobacter baumannii | University Hospital | ICU and Other Wards | 116 | Tracheal aspirates (32%), wound swabs (22%), blood (14%), bronchoalveolar specimens (11%) and urine, sterile fluids, catheter tips, abscess and sputum (each < 5%). |
| 2010 | Texas, USA; February-June 2008/March-June2009[55] | Enterobacter cloacae | Children’s Hospital | Children ICU and Other Wards | 3 | Fecal colonization |
| 2010 | France; 2003-2004[56] | Klebsiella pneumoniae | care centre for abdominal surgery | ICU and Other Wards | 8 | Rectal swab, urine culture, blood culture, tracheal aspirates |
| 2010 | Athens, Greece; February - December 2009[57] | Klebsiella pneumoniae | University Hospital | ICU and Other Wards | 42 | Hospital-acquired infections |
| 2010 | Wuerzburg, Germany; November - December 2007[58] | Pseudomonas aeruginosa | retrograde urography associated infection | ICU and Other Wards | 11 | Strains from urine or urological infection |
| 2010 | Kobe, Japan; September 2007-July 2008[59] | Pseudomonas aeruginosa | Medical Center General Hospital | ICU patients | 35 | All patients from ICU |
| 2011 | Athens, Greece; March 2004 - November 2005[60] | Enterobacteriaceae | University Hospital | ICU patients | 23 | All patients from ICU |
| 2011 | Kasserine Tunisia; 2009 - June 2010[61] | Escherichia coli | University Hospital | ICU patients | 2 | Rectal swab |
| 2011 | Essen, Germany; July 2010 - January 2011[62] | Klebsiella pneumoniae | University Hospital | ICU and Other Wards | 7 | Perianal or rectal swabs |
| 2011 | Tunis, Tunisia; January - November 2008[63] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 16 | All patients of the kidney transplantation unit; 20 strains from urine, 3 from cutaneous pus, and 1 from blood |
| 2011 | Murcia, Spain; 11-25 May 2009[64] | Pseudomonas aeruginosa | Tertiary Care Hospital | ICU and Other Wards | 6 | 4 ICU patients; strains from blood and sputum |
| 2011 | Central Japan; January 2006 - June 2009[65] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 51 | Mainly detected by urine culture in the first half, whereas isolation from respiratory tract samples became dominant in the latter half of the outbreak |
| 2011 | Rooterdam, Netherlands; January 2008 - November 2009[66] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 35 | 161 carbapenemase-producing: 74 (70%) were isolated from respiratory tract specimens, 6 (6%) from urine, 5 (5%) from blood, 8 (8%) from soft tissue or bone, 7 (7%) from intra-abdominal specimens and 6 (6%) from various other specimens. |
| 2012 | Chosun, Korea; January 2004 - December 200[67] | Acinetobacter baumannii | University Hospital | ICU patients | 77 | All patients from ICU |
| 2012 | Madrid, Spain; January 2009 - December 2009[68] | Klebsiella pneumoniae | University Hospital | ICU patients | 28 | Fatality rate was 13/28 (46%) |
| 2012 | UK; 2005 – 2011[69] | Pseudomonas aeruginosa | Tertiary Care and University Hospitals | ICU and Other Wards | 89 | Fatality rate was 34/89 (38.2%) |
| 2012 | Cape Town, South Africa; January 2010 - April 2011[70] | Pseudomonas aeruginosa | Tertiary Care and University Hospitals | ICU patients | 15 | 10 strains from blood, 2 from stool, 1 from bile, 1 from urine and 1 from a catheter tip |
| 2013 | Bologna, Italy; 1-15 June 2012[71] | Citrobacter freundii | University Hospital | ICU patients | 8 | Rectal swab |
| 2013 | Abidjan, Ivory Coast; February 2009 - November 2011[72] | Pseudomonas aeruginosa | University Hospital | ICU patients | 12 | All patients from ICU |
| 2013 | Thessalia, Larissa, Greece; 2010-2012[73] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 49 | All patients from ICU |
| 2013 | Taiwan; 2003-2007[74] | Pseudomonas aeruginosa | Regional Hospital | ICU and Other Wards | 50 | 8 ICU patients |
| 2013 | Buenos Aires, Argentina; July–September 2011[19] | Serratia marcescens | Tertiary Care Neonatal University Hospital | Neonatal ward patients | 3 | Rectal swab; fatality rate was 1/2 (50%) and one lost at follow-up |
| 2014 | Split, Croatia; June - August 2012[75] | Enterobacter cloacae | University Hospital | ICU patients | 6 | Strains from lower respiratory tract, blood, abdominal cavity and rectum; fatality rate was 4/6 (66.6%) |
| 2014 | Greece; 2003-2007[76] | Klebsiella pneumoniae | Tertiary Care and University Hospitals | ICU patients | 21 | All patients from ICU |
| 2014 | Rome, Italy; 2011-2012[77] | Pseudomonas aeruginosa | Tertiary Care Paediatric Hospital | Children with onco-haematological diseases; | 27 | 12 cases of bacteraemia, 6 other infections and 9 colonized; mortality rate was 67% |
| 2014 | Leiden, Netherlands; 2004- January 2012[78] | Pseudomonas aeruginosa | University Hospital | ICU patients | 20 | All patients from ICU |
| 2014 | China; December 2006 - July 2008[79] | Pseudomonas aeruginosa | Tertiary Care Hospitals | ICU patients | 1 | All patients from ICU |
| 2015 | Madrid, Spain - January 2009 - February 2014[80] | Klebsiella pneumoniae | University Hospital | ICU and Other Wards | 37 | OXA-48 ST11 clone |
| 2015 | Athens, Greece; September–November 2011[81] | Providencia stuartii | Tertiary Care Hospital | ICU patients | 10/5 | Strains from blood/urine; fatality rate was 7/15 (46.6%) |
| 2015 | Rotterdam, Netherlands; January - April 2012[82] | Pseudomonas aeruginosa | University Hospital | ICU and Other Wards | 30 | 9 ICU patients; patients undergone ERCP using a specific duodenoscope (TJF-Q180V) |
| 2015 | UK, 2003 – 2012[83] | Pseudomonas aeruginosa | 89 Tertiary Care Hospitals | ICU and Other Wards | 267 | Strains from urine (24%), respiratory (18%), wounds (17%) and blood (13%) |
| 2016 | Patras, Greece, January 2005 December 2014[84] | Klebsiella pneumoniae | University Hospital | ICU and Other Wards | 45 | 1668 carbapenemase-producing isolates |
| 2016 | Athens, Greece; December 2012 - March 2013[85] | Providencia stuartii | Tertiary Care Hospital | ICU patients | 6 | Fatality rate was 3/6 (50%) |
| 2016 | China; August 2011-July 2012[86] | Pseudomonas aeruginosa | 27 Tertiary Care Hospitals | ICU and Other Wards | 49/44/42 | Strains from pus/blood/urine |
| 2017 | Norway; 2007-2014[87] | Enterobacteriacee | University Hospital | ICU and Other Wards | 14 | Klebsiella pneumoniae (n = 10) and E. coli (n = 4) |
| 2017 | Jalisco, Mexico; September 2014 - July 2015[88] | Enterobacteriacee | Hospital Civil | ICU and Other Wards | 3 | Klebsiella pneumoniae (n=2), C. freundii (n = 1) |
| 2017 | Madrid, Spain - February 2014[89] | Klebsiella oxytoca | Children hospital | NICU | 8 | 8 VIM-Kox/4 also had VIM-Serratia/3 patients VIM -Enterobacteriaceae. NICU, In neonates with any symptom of infection, urine, blood, broncho-alveolar lavages and other samples based on the most likely focus of infection |
| 2017 | UK; 2005-2011[90] | Pseudomonas aeruginosa | Two University Hospitals in London and South Coast | ICU and Other Wards | 85 | 31 ICU patients; fatality rate was 34/85 (40%) |
| 2018 | Thessaloniki, Greece; January 2013- January 2015[91] | Klebsiella pneumoniae | University Hospital | ICU and Other Wards | 25 | Strain producing both KPC-2 and VIM-1 carbapenemases |
| 2018 | Cairo, Egypt, March 2015 August 2015[18] | Serratia marcescens | University Teaching Hospital | NICU | 15 | Isolates obtained from blood stream infections |
| Year | City | Setting | Number of cases(Infection and/or colonization) | Comments |
| 1984 | Naples[22] | NICU and Nursery | 88 | Outbreak linked to contaminated mucus aspiration apparatus and other contaminated instruments. Case fatality rate: 19% |
| 1988 | Genoa[23] | Adult ICU and surgical ward | 11 | Ventilators for assisted breathing became contaminated from index patient |
| 1994 | Varese[24] | Adult ICU | 43 | Strains from the ICU outbreak were multidrug resistance. 23 isolates from 18 other patients from other wards showed wide range of antibiotic susceptibility |
| 2001 | Naples[25] | NICU | 14 | 56 cases of colonization by S marcescens over a 15-month period. Fourteen of the 56 colonized infants developed clinical infections, 50% of which were major (sepsis, meningitis, or pneumonia) |
| 2003 | Naples[26] | Adult ICU | 13 | Strain was multidrug resistant, inducible AmpC betalactamase producing. There were three cases of sepsis, nine pneumonia and one surgical wound infection. Mortality was 84.6% |
| 2005 | Modena[27] | NICU | 15 | Simultaneous outbreak of Serratia marcescens and Klebsiella pneumonia (11 cases). One preterm baby died in which both organisms were involved |
| 2007 | Pavia[9] | NICU | 21 | Occurred in two separate outbreaks in 10 mo interval |
| 2009 | Verona[28] | NICU | 16 | 6 patients developed clinical diseases which included bacteremia, UTI, conjunctivitis and umbilical wound infection |
| 2011 | Pescara[7] | NICU | 6 | 5 cases were linked toan index case hospitalised for S. marcescens sepsis. Mortality was 40% |
| 2013 | Modena[6] | NICU | 127 | Reported two long term outbreaks occurred over a period of 10 years. 43 developed infection and 3 died |
| 2015 | Floerence[5] | NICU | 14 | In the surveillance post outbreak, 18 out of 65 patients tested positive for S. marcescens |
We report the first European outbreak of VIM-producing Serratia marcescens in adult polyvalent ICUs. Two patients developed an infection (bacteremia and LRTI) while one had colonization. No effective therapy is available for the treatment of VIM-producing S. marcescens. Methods to detect expression of carbapenem resistance should be widely available in all health care units to prevent the spread of multi-drug organisms and to limit horizontal transfer of the genes associated with drug resistance. Such active surveillance methods will help in averting future outbreaks.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zhang ZH S-Editor: Wang JL L-Editor: A E-Editor: Xing YX
| 1. | Logan LK, Weinstein RA. The Epidemiology of Carbapenem-Resistant Enterobacteriaceae: The Impact and Evolution of a Global Menace. J Infect Dis. 2017;215:S28-S36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 749] [Cited by in RCA: 1049] [Article Influence: 131.1] [Reference Citation Analysis (0)] |
| 2. | Samonis G, Korbila IP, Maraki S, Michailidou I, Vardakas KZ, Kofteridis D, Dimopoulou D, Gkogkozotou VK, Falagas ME. Trends of isolation of intrinsically resistant to colistin Enterobacteriaceae and association with colistin use in a tertiary hospital. Eur J Clin Microbiol Infect Dis. 2014;33:1505-1510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Milisavljevic V, Wu F, Larson E, Rubenstein D, Ross B, Drusin LM, Della-Latta P, Saiman L. Molecular epidemiology of Serratia marcescens outbreaks in two neonatal intensive care units. Infect Control Hosp Epidemiol. 2004;25:719-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Arslan U, Erayman I, Kirdar S, Yuksekkaya S, Cimen O, Tuncer I, Bozdogan B. Serratia marcescens sepsis outbreak in a neonatal intensive care unit. Pediatr Int. 2010;52:208-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 5. | Montagnani C, Cocchi P, Lega L, Campana S, Biermann KP, Braggion C, Pecile P, Chiappini E, de Martino M, Galli L. Serratia marcescens outbreak in a neonatal intensive care unit: crucial role of implementing hand hygiene among external consultants. BMC Infect Dis. 2015;15:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Casolari C, Pecorari M, Della Casa E, Cattani S, Venturelli C, Fabio G, Tagliazucchi S, Serpini GF, Migaldi M, Marchegiano P, Rumpianesi F, Ferrari F. Serratia marcescens in a neonatal intensive care unit: two long-term multiclone outbreaks in a 10-year observational study. New Microbiol. 2013;36:373-383. [PubMed] |
| 7. | Polilli E, Parruti G, Fazii P, D'Antonio D, Palmieri D, D'Incecco C, Mangifesta A, Garofalo G, Del Duca L, D'Amario C, Scimia M, Cortesi V, Fortunato V. Rapidly controlled outbreak of Serratia marcescens infection/colonisations in a neonatal intensive care unit, Pescara General Hospital, Pescara, Italy, April 2011. Euro Surveill. 2011;16:19892. [PubMed] |
| 8. | Dessì A, Puddu M, Testa M, Marcialis MA, Pintus MC, Fanos V. Serratia marcescens infections and outbreaks in neonatal intensive care units. J Chemother. 2009;21:493-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Perotti G, Bernardo ME, Spalla M, Matti C, Stronati M, Pagani L. Rapid control of two outbreaks of Serratia marcescens in a Northern Italian neonatal intensive care unit. J Chemother. 2007;19 Suppl 2:56-60. [PubMed] |
| 10. | Fiore M, Taccone FS, Leone S. Choosing the appropriate pharmacotherapy for multidrug-resistant Gram positive infections. Expert Opin Pharmacother. 2018;19:1517-1521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Wheat RP, Zuckerman A, Rantz LA. Infection due to chromobacteria; report of 11 cases. AMA Arch Intern Med. 1951;88:461-466. [PubMed] |
| 12. | Mahlen SD. Serratia infections: from military experiments to current practice. Clin Microbiol Rev. 2011;24:755-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 393] [Article Influence: 30.2] [Reference Citation Analysis (0)] |
| 13. | Stock I, Grueger T, Wiedemann B. Natural antibiotic susceptibility of strains of Serratia marcescens and the S. liquefaciens complex: S. liquefaciens sensu stricto, S. proteamaculans and S. grimesii. Int J Antimicrob Agents. 2003;22:35-47. [PubMed] |
| 14. | Jacoby GA. AmpC beta-lactamases. Clin Microbiol Rev. 2009;22:161-182, Table of Contents. [PubMed] |
| 15. | Tsakris A, Voulgari E, Poulou A, Kimouli M, Pournaras S, Ranellou K, Kosmopoulou O, Petropoulou D. In vivo acquisition of a plasmid-mediated bla(KPC-2) gene among clonal isolates of Serratia marcescens. J Clin Microbiol. 2010;48:2546-2549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Cai JC, Zhou HW, Zhang R, Chen GX. Emergence of Serratia marcescens, Klebsiella pneumoniae, and Escherichia coli Isolates possessing the plasmid-mediated carbapenem-hydrolyzing beta-lactamase KPC-2 in intensive care units of a Chinese hospital. Antimicrob Agents Chemother. 2008;52:2014-2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 151] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 17. | Kazmierczak KM, Rabine S, Hackel M, McLaughlin RE, Biedenbach DJ, Bouchillon SK, Sahm DF, Bradford PA. Multiyear, Multinational Survey of the Incidence and Global Distribution of Metallo-β-Lactamase-Producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2015;60:1067-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 167] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 18. | Ghaith DM, Zafer MM, Ismail DK, Al-Agamy MH, Bohol MFF, Al-Qahtani A, Al-Ahdal MN, Elnagdy SM, Mostafa IY. First reported nosocomial outbreak of Serratia marcescens harboring bla IMP-4 and bla VIM-2 in a neonatal intensive care unit in Cairo, Egypt. Infect Drug Resist. 2018;11:2211-2217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Nastro M, Monge R, Zintgraff J, Vaulet LG, Boutureira M, Famiglietti A, Rodriguez CH. First nosocomial outbreak of VIM-16-producing Serratia marcescens in Argentina. Clin Microbiol Infect. 2013;19:617-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Leone S, Cascella M, Pezone I, Fiore M. New antibiotics for the treatment of serious infections in intensive care unit patients. Curr Med Res Opin. 2019;35:1331-1334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 21. | Gilbert DN, Chambers HF, Eliopoulos GM, Saag MS, Pavia AT, editors. Sanford guide to antimicrobial therapy. 48th edition. Sperryville: Antimicrobial Therapy, Inc., 2018. . |
| 22. | Montanaro D, Grasso GM, Annino I, De Ruggiero N, Scarcella A, Schioppa F. Epidemiological and bacteriological investigation of Serratia marcescens epidemic in a nursery and in a neonatal intensive care unit. J Hyg (Lond). 1984;93:67-78. [PubMed] |
| 23. | Arzese A, Botta GA, Gesu GP, Schito G. Evaluation of a computer-assisted method of analysing SDS-PAGE protein profiles in tracing a hospital outbreak of Serratia marcescens. J Infect. 1988;17:35-42. [PubMed] |
| 24. | Pagani L, Luzzaro F, Ronza P, Rossi A, Micheletti P, Porta F, Romero E. Outbreak of extended-spectrum beta-lactamase producing Serratia marcescens in an intensive care unit. FEMS Immunol Med Microbiol. 1994;10:39-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Villari P, Crispino M, Salvadori A, Scarcella A. Molecular epidemiology of an outbreak of Serratia marcescens in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 2001;22:630-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Bagattini M, Crispino M, Gentile F, Barretta E, Schiavone D, Boccia MC, Triassi M, Zarrilli R. A nosocomial outbreak of Serratia marcescens producing inducible Amp C-type beta-lactamase enzyme and carrying antimicrobial resistance genes within a class 1 integron. J Hosp Infect. 2004;56:29-36. [PubMed] |
| 27. | Casolari C, Pecorari M, Fabio G, Cattani S, Venturelli C, Piccinini L, Tamassia MG, Gennari W, Sabbatini AM, Leporati G, Marchegiano P, Rumpianesi F, Ferrari F. A simultaneous outbreak of Serratia marcescens and Klebsiella pneumoniae in a neonatal intensive care unit. J Hosp Infect. 2005;61:312-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 28. | Ligozzi M, Fontana R, Aldegheri M, Scalet G, Lo Cascio G. Comparative evaluation of an automated repetitive-sequence-based PCR instrument versus pulsed-field gel electrophoresis in the setting of a Serratia marcescens nosocomial infection outbreak. J Clin Microbiol. 2010;48:1690-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Cornaglia G, Mazzariol A, Lauretti L, Rossolini GM, Fontana R. Hospital outbreak of carbapenem-resistant Pseudomonas aeruginosa producing VIM-1, a novel transferable metallo-beta-lactamase. Clin Infect Dis. 2000;31:1119-1125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 98] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 30. | Tsakris A, Pournaras S, Woodford N, Palepou MF, Babini GS, Douboyas J, Livermore DM. Outbreak of infections caused by Pseudomonas aeruginosa producing VIM-1 carbapenemase in Greece. J Clin Microbiol. 2000;38:1290-1292. [PubMed] |
| 31. | Yan JJ, Ko WC, Tsai SH, Wu HM, Wu JJ. Outbreak of infection with multidrug-resistant Klebsiella pneumoniae carrying bla(IMP-8) in a university medical center in Taiwan. J Clin Microbiol. 2001;39:4433-4439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 32. | Scoulica EV, Neonakis IK, Gikas AI, Tselentis YJ. Spread of bla(VIM-1)-producing E. coli in a university hospital in Greece. Genetic analysis of the integron carrying the bla(VIM-1) metallo-beta-lactamase gene. Diagn Microbiol Infect Dis. 2004;48:167-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 33. | Crespo MP, Woodford N, Sinclair A, Kaufmann ME, Turton J, Glover J, Velez JD, Castañeda CR, Recalde M, Livermore DM. Outbreak of carbapenem-resistant Pseudomonas aeruginosa producing VIM-8, a novel metallo-beta-lactamase, in a tertiary care center in Cali, Colombia. J Clin Microbiol. 2004;42:5094-5101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 34. | Ikonomidis A, Tokatlidou D, Kristo I, Sofianou D, Tsakris A, Mantzana P, Pournaras S, Maniatis AN. Outbreaks in distinct regions due to a single Klebsiella pneumoniae clone carrying a bla VIM-1 metallo-{beta}-lactamase gene. J Clin Microbiol. 2005;43:5344-5347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 35. | Laupland KB, Parkins MD, Church DL, Gregson DB, Louie TJ, Conly JM, Elsayed S, Pitout JD. Population-based epidemiological study of infections caused by carbapenem-resistant Pseudomonas aeruginosa in the Calgary Health Region: importance of metallo-beta-lactamase (MBL)-producing strains. J Infect Dis. 2005;192:1606-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 83] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 36. | Lolans K, Queenan AM, Bush K, Sahud A, Quinn JP. First nosocomial outbreak of Pseudomonas aeruginosa producing an integron-borne metallo-beta-lactamase (VIM-2) in the United States. Antimicrob Agents Chemother. 2005;49:3538-3540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 37. | Zavascki AP, Gaspareto PB, Martins AF, Gonçalves AL, Barth AL. Outbreak of carbapenem-resistant Pseudomonas aeruginosa producing SPM-1 metallo-{beta}-lactamase in a teaching hospital in southern Brazil. J Antimicrob Chemother. 2005;56:1148-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 38. | Pournaras S, Markogiannakis A, Ikonomidis A, Kondyli L, Bethimouti K, Maniatis AN, Legakis NJ, Tsakris A. Outbreak of multiple clones of imipenem-resistant Acinetobacter baumannii isolates expressing OXA-58 carbapenemase in an intensive care unit. J Antimicrob Chemother. 2006;57:557-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 118] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 39. | Kassis-Chikhani N, Decré D, Gautier V, Burghoffer B, Saliba F, Mathieu D, Samuel D, Castaing D, Petit JC, Dussaix E, Arlet G. First outbreak of multidrug-resistant Klebsiella pneumoniae carrying blaVIM-1 and blaSHV-5 in a French university hospital. J Antimicrob Chemother. 2006;57:142-145. [PubMed] |
| 40. | Lagatolla C, Edalucci E, Dolzani L, Riccio ML, De Luca F, Medessi E, Rossolini GM, Tonin EA. Molecular evolution of metallo-beta-lactamase-producing Pseudomonas aeruginosa in a nosocomial setting of high-level endemicity. J Clin Microbiol. 2006;44:2348-2353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 41. | Libisch B, Muzslay M, Gacs M, Minárovits J, Knausz M, Watine J, Ternák G, Kenéz E, Kustos I, Rókusz L, Széles K, Balogh B, Füzi M. Molecular epidemiology of VIM-4 metallo-beta-lactamase-producing Pseudomonas sp. isolates in Hungary. Antimicrob Agents Chemother. 2006;50:4220-4223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 42. | Tato M, Coque TM, Ruíz-Garbajosa P, Pintado V, Cobo J, Sader HS, Jones RN, Baquero F, Cantón R. Complex clonal and plasmid epidemiology in the first outbreak of Enterobacteriaceae infection involving VIM-1 metallo-beta-lactamase in Spain: toward endemicity? Clin Infect Dis. 2007;45:1171-1178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 43. | Empel J, Filczak K, Mrówka A, Hryniewicz W, Livermore DM, Gniadkowski M. Outbreak of Pseudomonas aeruginosa infections with PER-1 extended-spectrum beta-lactamase in Warsaw, Poland: further evidence for an international clonal complex. J Clin Microbiol. 2007;45:2829-2834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 44. | Mentzelopoulos SD, Pratikaki M, Platsouka E, Kraniotaki H, Zervakis D, Koutsoukou A, Nanas S, Paniara O, Roussos C, Giamarellos-Bourboulis E, Routsi C, Zakynthinos SG. Prolonged use of carbapenems and colistin predisposes to ventilator-associated pneumonia by pandrug-resistant Pseudomonas aeruginosa. Intensive Care Med. 2007;33:1524-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 45. | Tsakris A, Ikonomidis A, Poulou A, Spanakis N, Vrizas D, Diomidous M, Pournaras S, Markou F. Clusters of imipenem-resistant Acinetobacter baumannii clones producing different carbapenemases in an intensive care unit. Clin Microbiol Infect. 2008;14:588-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 46] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 46. | Loli A, Tzouvelekis LS, Gianneli D, Tzelepi E, Miriagou V. Outbreak of Acinetobacter baumannii with chromosomally encoded VIM-1 undetectable by imipenem-EDTA synergy tests. Antimicrob Agents Chemother. 2008;52:1894-1896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 47. | Cagnacci S, Gualco L, Roveta S, Mannelli S, Borgianni L, Docquier JD, Dodi F, Centanaro M, Debbia E, Marchese A, Rossolini GM. Bloodstream infections caused by multidrug-resistant Klebsiella pneumoniae producing the carbapenem-hydrolysing VIM-1 metallo-beta-lactamase: first Italian outbreak. J Antimicrob Chemother. 2008;61:296-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 48. | Psichogiou M, Tassios PT, Avlamis A, Stefanou I, Kosmidis C, Platsouka E, Paniara O, Xanthaki A, Toutouza M, Daikos GL, Tzouvelekis LS. Ongoing epidemic of blaVIM-1-positive Klebsiella pneumoniae in Athens, Greece: a prospective survey. J Antimicrob Chemother. 2008;61:59-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 90] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 49. | Tokatlidou D, Tsivitanidou M, Pournaras S, Ikonomidis A, Tsakris A, Sofianou D. Outbreak caused by a multidrug-resistant Klebsiella pneumoniae clone carrying blaVIM-12 in a university hospital. J Clin Microbiol. 2008;46:1005-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 50. | Corvec S, Poirel L, Espaze E, Giraudeau C, Drugeon H, Nordmann P. Long-term evolution of a nosocomial outbreak of Pseudomonas aeruginosa producing VIM-2 metallo-enzyme. J Hosp Infect. 2008;68:73-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 51. | Woodford N, Zhang J, Kaufmann ME, Yarde S, Tomas Mdel M, Faris C, Vardhan MS, Dawson S, Cotterill SL, Livermore DM. Detection of Pseudomonas aeruginosa isolates producing VEB-type extended-spectrum beta-lactamases in the United Kingdom. J Antimicrob Chemother. 2008;62:1265-1268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 52. | Giakoupi P, Maltezou H, Polemis M, Pappa O, Saroglou G, Vatopoulos A; Greek System for the Surveillance of Antimicrobial Resistance. KPC-2-producing Klebsiella pneumoniae infections in Greek hospitals are mainly due to a hyperepidemic clone. Euro Surveill. 2009;14:19218. [PubMed] |
| 53. | Siarkou VI, Vitti D, Protonotariou E, Ikonomidis A, Sofianou D. Molecular epidemiology of outbreak-related pseudomonas aeruginosa strains carrying the novel variant blaVIM-17 metallo-beta-lactamase gene. Antimicrob Agents Chemother. 2009;53:1325-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 54. | Kulah C, Mooij MJ, Comert F, Aktas E, Celebi G, Ozlu N, Rijnsburger MC, Savelkoul PH. Characterisation of carbapenem-resistant Acinetobacter baumannii outbreak strains producing OXA-58 in Turkey. Int J Antimicrob Agents. 2010;36:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 55. | Oteo J, Hernández-Almaraz JL, Gil-Antón J, Vindel A, Fernández S, Bautista V, Campos J. Outbreak of vim-1-carbapenemase-producing Enterobacter cloacae in a pediatric intensive care unit. Pediatr Infect Dis J. 2010;29:1144-1146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 56. | Kassis-Chikhani N, Saliba F, Carbonne A, Neuville S, Decre D, Sengelin C, Guerin C, Gastiaburu N, Lavigne-Kriaa A, Boutelier C, Arlet G, Samuel D, Castaing D, Dussaix E, Jarlier V. Extended measures for controlling an outbreak of VIM-1 producing imipenem-resistant Klebsiella pneumoniae in a liver transplant centre in France, 2003-2004. Euro Surveill. 2010;15:19713. [PubMed] |
| 57. | Zioga A, Miriagou V, Tzelepi E, Douzinas E, Tsakiri M, Legakis NJ, Daikos GL, Tzouvelekis LS. The ongoing challenge of acquired carbapenemases: a hospital outbreak of Klebsiella pneumoniae simultaneously producing VIM-1 and KPC-2. Int J Antimicrob Agents. 2010;36:190-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 58. | Elias J, Schoen C, Heinze G, Valenza G, Gerharz E, Gerharz H, Vogel U. Nosocomial outbreak of VIM-2 metallo-β-lactamase-producing Pseudomonas aeruginosa associated with retrograde urography. Clin Microbiol Infect. 2010;16:1494-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 59. | Miki K, Takegawa H, Etoh M, Hayashi M, Haruta T, Yamane K, Arakawa Y. [First outbreak report of VIM-1 metallo-beta-lactamase producing Pseudomonas aeruginosa in Japan]. Kansenshogaku Zasshi. 2010;84:721-726. [PubMed] |
| 60. | Koratzanis E, Souli M, Galani I, Chryssouli Z, Armaganidis A, Giamarellou H. Epidemiology and molecular characterisation of metallo-β-lactamase-producing Enterobacteriaceae in a university hospital Intensive Care Unit in Greece. Int J Antimicrob Agents. 2011;38:390-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 61. | Chouchani C, Marrakchi R, Ferchichi L, El Salabi A, Walsh TR. VIM and IMP metallo-β-lactamases and other extended-spectrum β-lactamases in Escherichia coli and Klebsiella pneumoniae from environmental samples in a Tunisian hospital. APMIS. 2011;119:725-732. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 62. | Steinmann J, Kaase M, Gatermann S, Popp W, Steinmann E, Damman M, Paul A, Saner F, Buer J, Rath P. Outbreak due to a Klebsiella pneumoniae strain harbouring KPC-2 and VIM-1 in a German university hospital, July 2010 to January 2011. Euro Surveill. 2011;16:19944. [PubMed] |
| 63. | Hammami S, Boutiba-Ben Boubaker I, Ghozzi R, Saidani M, Amine S, Ben Redjeb S. Nosocomial outbreak of imipenem-resistant Pseudomonas aeruginosa producing VIM-2 metallo-β-lactamase in a kidney transplantation unit. Diagn Pathol. 2011;6:106. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 64. | Jimeno A, Alcalde MM, Blázquez A. [Epidemic outbreak of Pseudomonas aeruginosa carbepenem-resistant producing metallo-beta-lactamase]. Rev Clin Esp. 2011;211:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 65. | Tsutsui A, Suzuki S, Yamane K, Matsui M, Konda T, Marui E, Takahashi K, Arakawa Y. Genotypes and infection sites in an outbreak of multidrug-resistant Pseudomonas aeruginosa. J Hosp Infect. 2011;78:317-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 66. | Van der Bij AK, Van Mansfeld R, Peirano G, Goessens WH, Severin JA, Pitout JD, Willems R, Van Westreenen M. First outbreak of VIM-2 metallo-β-lactamase-producing Pseudomonas aeruginosa in The Netherlands: microbiology, epidemiology and clinical outcomes. Int J Antimicrob Agents. 2011;37:513-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 67. | Chaulagain BP, Jang SJ, Ahn GY, Ryu SY, Kim DM, Park G, Kim WY, Shin JH, Kook JK, Kang SH, Moon DS, Park YJ. Molecular epidemiology of an outbreak of imipenem-resistant Acinetobacter baumannii carrying the ISAba1-bla(OXA-51-like) genes in a Korean hospital. Jpn J Infect Dis. 2012;65:162-166. [PubMed] |
| 68. | Sánchez-Romero I, Asensio A, Oteo J, Muñoz-Algarra M, Isidoro B, Vindel A, Alvarez-Avello J, Balandín-Moreno B, Cuevas O, Fernández-Romero S, Azañedo L, Sáez D, Campos J. Nosocomial outbreak of VIM-1-producing Klebsiella pneumoniae isolates of multilocus sequence type 15: molecular basis, clinical risk factors, and outcome. Antimicrob Agents Chemother. 2012;56:420-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 69. | Breathnach AS, Cubbon MD, Karunaharan RN, Pope CF, Planche TD. Multidrug-resistant Pseudomonas aeruginosa outbreaks in two hospitals: association with contaminated hospital waste-water systems. J Hosp Infect. 2012;82:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 136] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 70. | Jacobson RK, Minenza N, Nicol M, Bamford C. VIM-2 metallo-β-lactamase-producing Pseudomonas aeruginosa causing an outbreak in South Africa. J Antimicrob Chemother. 2012;67:1797-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 71. | Gaibani P, Ambretti S, Farruggia P, Bua G, Berlingeri A, Tamburini MV, Cordovana M, Guerra L, Mazzetti M, Roncarati G, Tenace C, Moro ML, Gagliotti C, Landini MP, Sambri V. Outbreak of Citrobacter freundii carrying VIM-1 in an Italian Hospital, identified during the carbapenemases screening actions, June 2012. Int J Infect Dis. 2013;17:e714-e717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 72. | Jeannot K, Guessennd N, Fournier D, Müller E, Gbonon V, Plésiat P. Outbreak of metallo-β-lactamase VIM-2-positive strains of Pseudomonas aeruginosa in the Ivory Coast. J Antimicrob Chemother. 2013;68:2952-2954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 73. | Koutsogiannou M, Drougka E, Liakopoulos A, Jelastopulu E, Petinaki E, Anastassiou ED, Spiliopoulou I, Christofidou M. Spread of multidrug-resistant Pseudomonas aeruginosa clones in a university hospital. J Clin Microbiol. 2013;51:665-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 74. | Shu JC, Su LH, Chia JH, Huang SH, Kao YC, Lee SC, Wu TL. Identification of a hidden outbreak due to the spread of a VIM-3-producing, extensive drug-resistant Pseudomonas aeruginosa (XDRPA) clone at a regional hospital in Taiwan. Epidemiol Infect. 2013;141:1713-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 75. | Novak A, Goic-Barisic I, Andrasevic AT, Butic I, Radic M, Jelic M, Rubic Z, Tonkic M. Monoclonal outbreak of VIM-1-carbapenemase-producing Enterobacter cloacae in intensive care unit, University Hospital Centre Split, Croatia. Microb Drug Resist. 2014;20:399-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 76. | Hasan CM, Turlej-Rogacka A, Vatopoulos AC, Giakkoupi P, Maâtallah M, Giske CG. Dissemination of blaVIM in Greece at the peak of the epidemic of 2005-2006: clonal expansion of Klebsiella pneumoniae clonal complex 147. Clin Microbiol Infect. 2014;20:34-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 77. | Ciofi Degli Atti M, Bernaschi P, Carletti M, Luzzi I, García-Fernández A, Bertaina A, Sisto A, Locatelli F, Raponi M. An outbreak of extremely drug-resistant Pseudomonas aeruginosa in a tertiary care pediatric hospital in Italy. BMC Infect Dis. 2014;14:494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 78. | Knoester M, de Boer MG, Maarleveld JJ, Claas EC, Bernards AT, de Jonge E, van Dissel JT, Veldkamp KE. An integrated approach to control a prolonged outbreak of multidrug-resistant Pseudomonas aeruginosa in an intensive care unit. Clin Microbiol Infect. 2014;20:O207-O215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 79. | Qing Y, Cao KY, Fang ZL, Huang YM, Zhang XF, Tian GB, Huang X. Outbreak of PER-1 and diversity of β-lactamases among ceftazidime-resistant Pseudomonas aeruginosa clinical isolates. J Med Microbiol. 2014;63:386-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 80. | Brañas P, Villa J, Viedma E, Mingorance J, Orellana MA, Chaves F. Molecular epidemiology of carbapenemase-producing Klebsiella pneumoniae in a hospital in Madrid: Successful establishment of an OXA-48 ST11 clone. Int J Antimicrob Agents. 2015;46:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 81. | Douka E, Perivolioti E, Kraniotaki E, Fountoulis K, Economidou F, Tsakris A, Skoutelis A, Routsi C. Emergence of a pandrug-resistant VIM-1-producing Providencia stuartii clonal strain causing an outbreak in a Greek intensive care unit. Int J Antimicrob Agents. 2015;45:533-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 82. | Verfaillie CJ, Bruno MJ, Voor in 't Holt AF, Buijs JG, Poley JW, Loeve AJ, Severin JA, Abel LF, Smit BJ, de Goeij I, Vos MC. Withdrawal of a novel-design duodenoscope ends outbreak of a VIM-2-producing Pseudomonas aeruginosa. Endoscopy. 2015;47:493-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 83. | Wright LL, Turton JF, Livermore DM, Hopkins KL, Woodford N. Dominance of international 'high-risk clones' among metallo-β-lactamase-producing Pseudomonas aeruginosa in the UK. J Antimicrob Chemother. 2015;70:103-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 84. | Spyropoulou A, Papadimitriou-Olivgeris M, Bartzavali C, Vamvakopoulou S, Marangos M, Spiliopoulou I, Anastassiou ED, Christofidou M. A ten-year surveillance study of carbapenemase-producing Klebsiella pneumoniae in a tertiary care Greek university hospital: predominance of KPC- over VIM- or NDM-producing isolates. J Med Microbiol. 2016;65:240-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 85. | Oikonomou O, Liakopoulos A, Phee LM, Betts J, Mevius D, Wareham DW. Providencia stuartii Isolates from Greece: Co-Carriage of Cephalosporin (blaSHV-5, blaVEB-1), Carbapenem (blaVIM-1), and Aminoglycoside (rmtB) Resistance Determinants by a Multidrug-Resistant Outbreak Clone. Microb Drug Resist. 2016;22:379-386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 86. | Fan X, Wu Y, Xiao M, Xu ZP, Kudinha T, Bazaj A, Kong F, Xu YC. Diverse Genetic Background of Multidrug-Resistant Pseudomonas aeruginosa from Mainland China, and Emergence of an Extensively Drug-Resistant ST292 Clone in Kunming. Sci Rep. 2016;6:26522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 87. | Samuelsen Ø, Overballe-Petersen S, Bjørnholt JV, Brisse S, Doumith M, Woodford N, Hopkins KL, Aasnæs B, Haldorsen B, Sundsfjord A. Norwegian Study Group on CPE. Molecular and epidemiological characterization of carbapenemase-producing Enterobacteriaceae in Norway, 2007 to 2014. PLoS One. 2017;12:e0187832. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 55] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 88. | Bocanegra-Ibarias P, Garza-González E, Morfín-Otero R, Barrios H, Villarreal-Treviño L, Rodríguez-Noriega E, Garza-Ramos U, Petersen-Morfin S, Silva-Sanchez J. Molecular and microbiological report of a hospital outbreak of NDM-1-carrying Enterobacteriaceae in Mexico. PLoS One. 2017;12:e0179651. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 73] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 89. | Herruzo R, Ruiz G, Gallego S, Diez J, Sarria A, Omeñaca F. VIM-Klebsiella oxytoca outbreak in a Neonatal Intensive Care Unit. This time it wasn't the drain. J Prev Med Hyg. 2017;58:E302-E307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 90. | Kizny Gordon AE, Mathers AJ, Cheong EYL, Gottlieb T, Kotay S, Walker AS, Peto TEA, Crook DW, Stoesser N. The Hospital Water Environment as a Reservoir for Carbapenem-Resistant Organisms Causing Hospital-Acquired Infections-A Systematic Review of the Literature. Clin Infect Dis. 2017;64:1435-1444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 246] [Article Influence: 35.1] [Reference Citation Analysis (0)] |
| 91. | Protonotariou E, Poulou A, Politi L, Sgouropoulos I, Metallidis S, Kachrimanidou M, Pournaras S, Tsakris A, Skoura L. Hospital outbreak due to a Klebsiella pneumoniae ST147 clonal strain co-producing KPC-2 and VIM-1 carbapenemases in a tertiary teaching hospital in Northern Greece. Int J Antimicrob Agents. 2018;52:331-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |