Published online Oct 26, 2019. doi: 10.12998/wjcc.v7.i20.3358
Peer-review started: July 21, 2019
First decision: August 2, 2019
Revised: August 11, 2019
Accepted: September 11, 2019
Article in press: September 11, 2019
Published online: October 26, 2019
Processing time: 101 Days and 17.6 Hours
Sister Mary Joseph’s nodule (SMJN) is rare and may occur independently or simultaneously with malignant tumors in the abdominal cavity. It has a poor prognosis. Endometrial carcinoma is the most common malignant tumor in the upper segment of the female reproductive tract; however, it rarely occurs with SMJN. We here report a case of endometrial carcinoma with SMJN.
A 75-year-old woman was diagnosed with endometrial cancer > 2 years ago. After multiple cycles of chemotherapy, an obvious but painless umbilical mass was detected 2 wk before admission. The patient did not undergo surgical treatment but received chemotherapy, which was different from previous chemotherapy, for three consecutive cycles after discovery of umbilical metastases. Currently, the umbilical metastatic tumor has reduced, and the quality of life of the patient has significantly improved.
Once the umbilical mass is found, the possibility of SMJN should be considered. We should also take into account the poor prognosis of endometrial carcinoma complicated with umbilical metastasis, especially in patients with advanced tumors, and it is important to choose an appropriate treatment.
Core tip: We report a rare case of endometrial carcinoma with Sister Mary Joseph’s nodule (SMJN). After three cycles of systemic chemotherapy, the umbilical metastatic tumor was reduced, and the quality of life of the patient was significantly improved. We emphasized the poor prognosis of endometrial carcinoma complicated with umbilical metastasis, especially in patients with advanced tumors. The pathway of umbilical metastasis of malignant tumor was discussed. Combined with other reports, we also analyzed the appropriate treatment of malignant tumors with SMJN.
- Citation: Li Y, Guo P, Wang B, Jia YT. Sister Mary Joseph’s nodule in endometrial carcinoma: A case report. World J Clin Cases 2019; 7(20): 3358-3363
- URL: https://www.wjgnet.com/2307-8960/full/v7/i20/3358.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i20.3358
Sister Mary Joseph’s nodule (SMJN) is a metastatic nodule of the navel caused by a malignant tumor in the abdominal cavity[1]. Originally, it was named by Sir Hamilton Bailey in 1949 after Sister Mary Joseph first noted the association between umbilical nodules and intra-abdominal or pelvic malignancy. SMJN is rare and may occur independently or simultaneously with malignant tumors in the abdominal cavity. It has a poor prognosis. The most common primary tumors of SMJN are gastric and ovarian cancer, and SMJN caused by endometrial cancer is relatively infrequent[2]. Here, we report a case of endometrial carcinoma with SMJN and review the related literature.
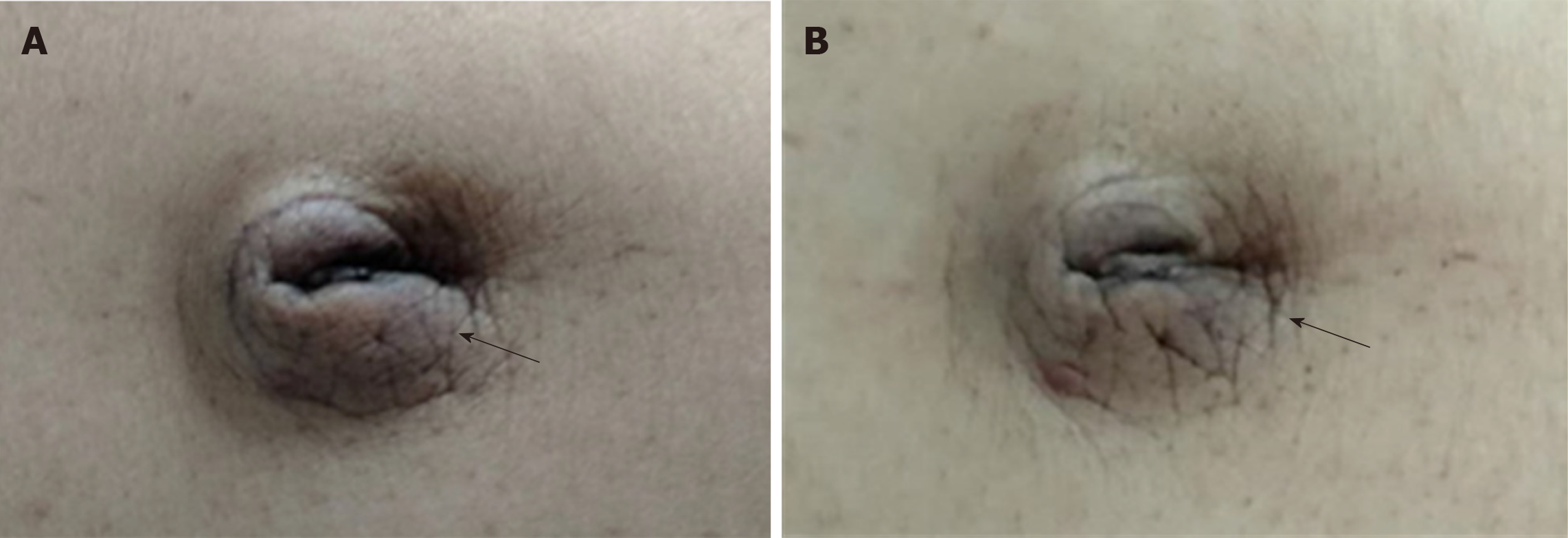
A 75-year-old woman was diagnosed with endometrial adenocarcinoma > 2 years ago and received multiple cycles of chemotherapy. The umbilical mass was found 2 wk before admission, without obvious cause (Figure 1A).
Two years before, the patient had been diagnosed with endometrial adenocarcinoma and received multiple cycles of chemotherapy. About 2 wk before admission, she found the umbilical mass by herself, whose size was similar to a broad bean, and no symptoms such as pain or ulceration were present. At that time, no attention was paid to it, and the umbilical mass grew progressively. When the umbilical mass was detected, it was already the size of a quail egg.
The patient has a history of hypertension for > 20 years. There was no particular history of trauma, blood transfusion, or allergy.
Non-apparent abnormality.
Physical examination revealed an umbilical mass measuring approximately 30 mm × 30 mm. The mass was firm, immovable, nontender, and well demarcated. There were no obvious symptoms of any discomfort, such as pain or ulceration.
We examined the patient’s tumor markers and found that her carbohydrate antigen (CA) 125 and CA153 levels were 449.90 and 73.24 U/mL, respectively (normal reference values are 35.0 and 25.0 U/mL, respectively).
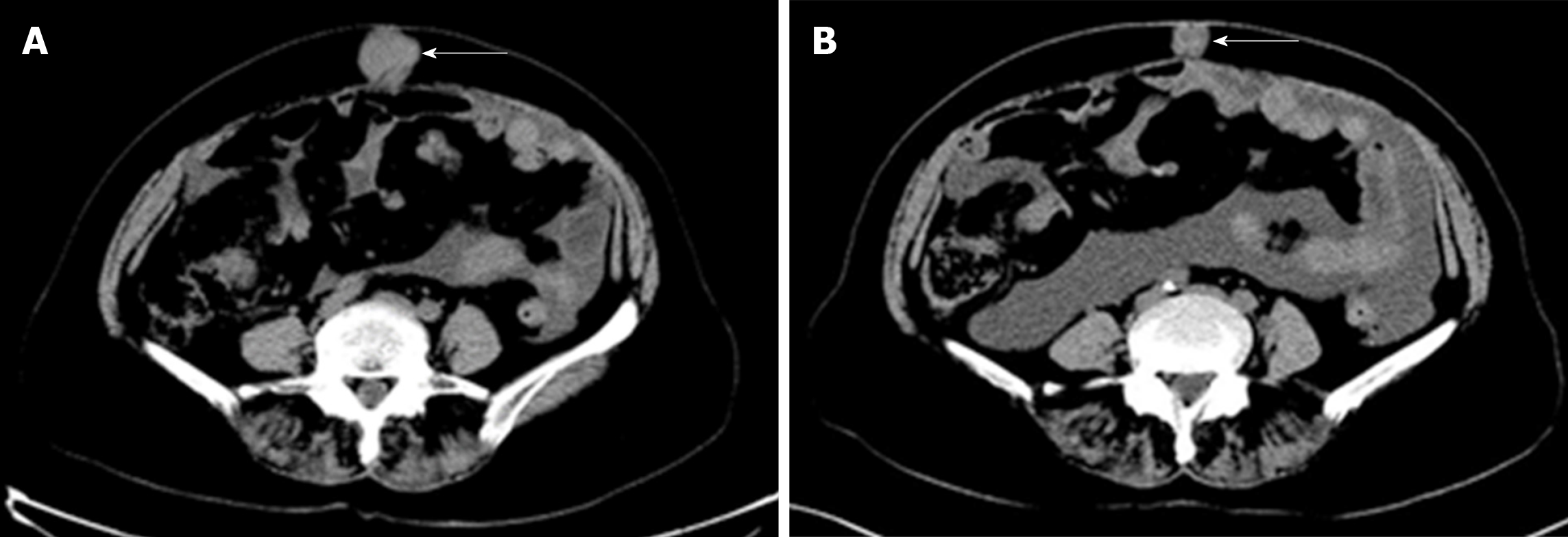
Computed tomography (CT) showed that there were multiple metastases in the abdomen and pelvis, and a circular soft tissue density shadow with a clear boundary and size of about 32 mm × 33 mm × 39 mm (Figure 2A). Moreover, there were many small nodules in the abdominal cavity, which could be tumor metastasis to the peritoneum. Her uterus was somewhat irregular and may have been the cause of the primary lesion. Beyond that, many small lymph nodes were also seen in the retroperitoneum, bilateral ilium vessels and inguinal area, and the patient also had a small amount of abdominal and pelvic fluid.
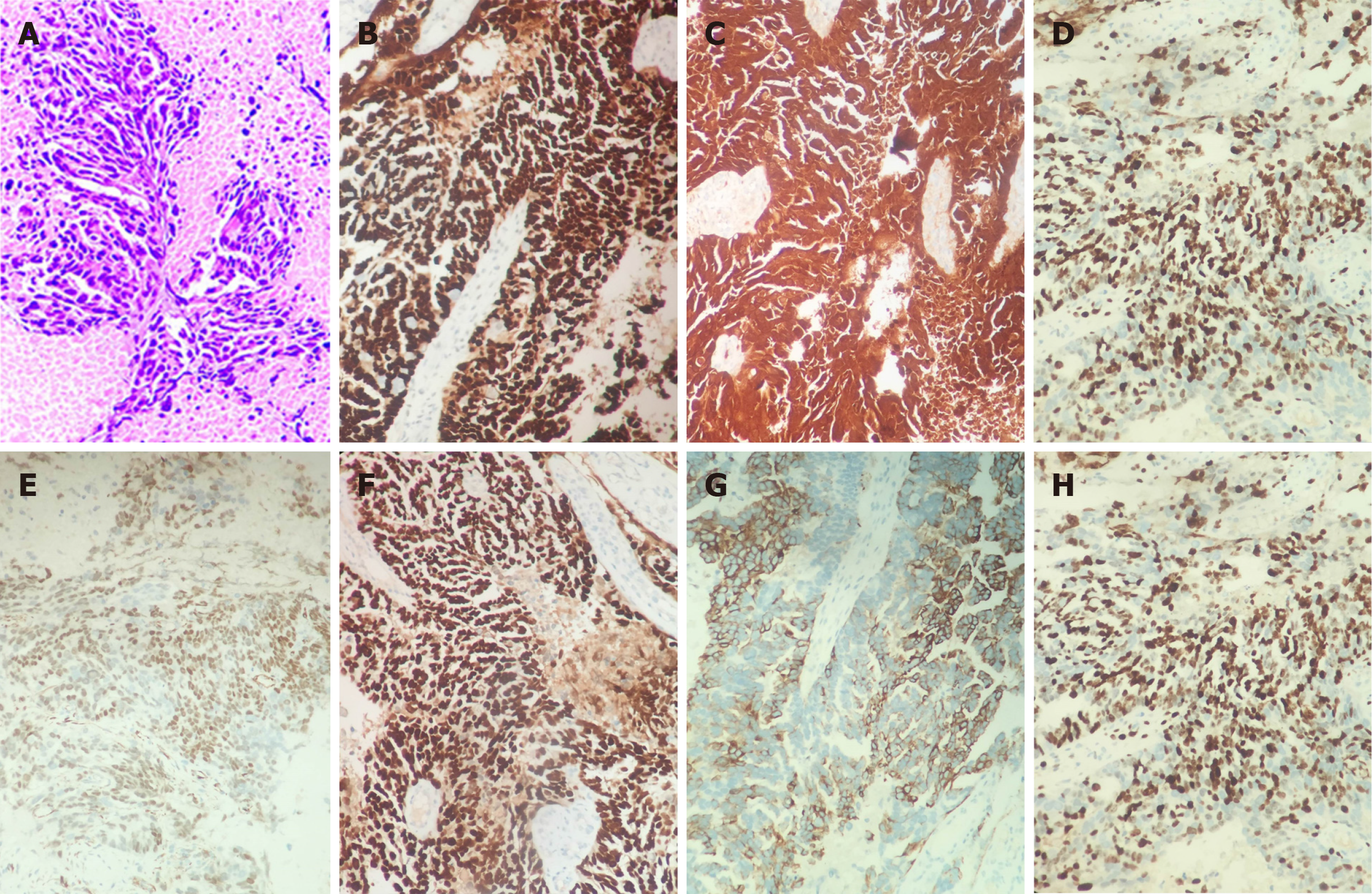
To determine the origin of the umbilical mass, we performed a puncture biopsy under ultrasound guidance. The pathological results suggested invasive adenocarcinoma (Figure 3A). We further performed immunohistochemistry, which showed a high-grade serous adenocarcinoma. The results of immunohistochemical staining were as follows: p53 (+++), p16 (+), ER (+++), PR (+), WT-1 (+), PAX-8 (+), TTF-1 (–), CDX-2 (–), CK7 (+), CK20 (–), and Ki-67 (+) (Figure 3B-H). We tested the patient for related genes and found no definite mutations in BRCA1 and BRCA2 genes.
Instead of administering olaparib, we administered systemic chemotherapy: Doxorubicin liposomes 40 mg on the first day, Nida platinum 100 mg on the second day, in a 21-d cycle.
After three cycles of systemic chemotherapy, the size of the umbilical mass was markedly reduced, and the quality of life of the patient was significantly improved. The patient continued to receive systemic chemotherapy (Figures 1B and 2B).
Umbilical tumors can be divided into primary and metastatic tumors[1]. SMJN is a rare tumor formed by metastasis of a malignant tumor of the abdominal or pelvic organs to the umbilical cord, accounting for about 1% and 3%[3]. Some patients are first diagnosed with palpable masses at the umbilicus, while others are clinically diagnosed with umbilical masses after they are known to have a malignant tumor. Some patients with umbilical masses may experience pain, ulceration or empyema. On the contrary, although the umbilical metastasis of this patient was visible to the naked eye, there were no obvious symptoms of any discomfort, such as pain or ulceration. The most common primary tumors in SMJN include the stomach, ovary, and colon cancers[4]. According to the current study, there is a relationship between the location of the primary tumor of SMJN and the sex of the patient. Men are more likely to develop gastric cancer, while women develop ovarian cancer. Many studies have explored the association between SMJN and other cancers such as pancreatic and ovarian cancer[5]. This female patient, whose primary tumor was endometrial cancer, still had a rare SMJN after multiple cycles of chemotherapy.
Pathology is the gold standard for the diagnosis of tumors. It includes fine needle puncture, rough needle puncture, biopsy, and surgical resection. SMJN primary and secondary lesions cannot be distinguished using imaging. Therefore, puncture can be considered to confirm the pathological diagnosis of umbilical masses of unknown nature and origin. Fine needle aspiration cytology can be used to observe the changes in cell structure and morphology, but sometimes the source may not be determined. In contrast, tissue punctured by a rough needle can be used for immunohistochemistry, and then determine the source of the tumor, which can help with diagnosis. Nevertheless, rough needle puncture of an umbilical mass can lead to unexpected results. For example, if the umbilical mass is an umbilical hernia, the rough needle puncture may lead to a rupture of the intestinal wall. Therefore, we need to puncture the umbilical mass under CT or ultrasound guidance to ensure safety.
The route of transfer of SMJN has not yet been clarified. From an anatomical point of view, a variety of pathways may lead to umbilical metastasis[6]. There is not only a rich supply of blood and lymphatic vessels around the umbilicus, but it is also the meeting point of multiple peritoneal folds. Theoretically, malignant tumors should be easily transferred to the umbilicus through these blood vessels or lymphatic vessels, but in practice, umbilical metastasis of malignant tumors is rare. We speculate that this may be due to the fact that the blood and lymphatic vessels in the umbilicus are atretic in physiological state. After the malignant tumor has extensive abdominal metastasis, the tumor cells oppress the blood and lymph vessels and make them dilate. This causes the metastasis channel to the umbilicus to be opened. This explains why umbilical metastasis is rare, and the most common pathway of metastasis is direct peritoneal diffusion[7]. The abdominal CT scan of the patient showed thickening of the peritoneum and enlarged lymph nodes. We speculate that it was also tumor metastasis. The umbilical metastasis in this patient may have been caused by direct peritoneal diffusion. However, it does not rule out metastasis to the umbilicus through the blood and lymph vessels.
There is no clear conclusion about the treatment of SMJN. SMJN generally occurs in patients with advanced tumors and extensive abdominal metastasis, even at the end stage[8]. In this case of SMJN, we applied a standardized treatment for an advanced tumor and achieved good results. In contrast, for patients who have undergone surgery, the prognosis is not necessarily superior to that with systemic chemotherapy. Wu et al reported that a patient with colon cancer complicated with SMJN underwent surgical resection of the primary site without postoperative intervention and died 4 mo later[9]. Rahman et al[10] reported a patient with endometrial squamous cell carcinoma complicated with SMJN who underwent endometrial curettage and resection of the umbilical metastasis. The patient received standardized chemotherapy after the operation, but still died 13 mo after diagnosis[10]. The primary tumor of this patient was found, followed by abdominal metastasis and SMJN. Considering that the patient had an advanced malignant tumor, we adopted standard systemic chemotherapy. SMJN was significantly smaller than before, and the quality of life was also improved after three cycles of standard chemotherapy (Figures 1B and 2B).
Once the umbilical mass is found, the possibility of SMJN should be considered. The necessary differential diagnosis should also be made. For safety reasons, it is best to determine a pathological diagnosis and the source of the tumor under the guidance of CT or ultrasound. If SMJN is determined, extensive abdominal implantation may have been found at the time, as we shared in the present case. However, it remains to be explored whether surgery or chemotherapy should be the first choice for SMJN, or whether it should be combined with radiotherapy. In our case, systemic chemotherapy was effective, and she expressed her willingness to continue with it. We are currently closely following her up.
We express our thanks to the patient and her family for permission to publish this case report.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Katuchova J S-Editor: Gong ZM L-Editor: Filipodia E-Editor: Qi LL
| 1. | Sethi K, Shareef N, Bloom S. The Sister Mary Joseph nodule. Br J Hosp Med (Lond). 2018;79:C27-C29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Chalya PL, Mabula JB, Rambau PF, McHembe MD. Sister Mary Joseph's nodule at a University teaching hospital in northwestern Tanzania: a retrospective review of 34 cases. World J Surg Oncol. 2013;11:151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Sengupta S, Church E, Chia KV. Sister Mary Joseph's nodule: recurrent endometrial adenocarcinoma presenting as an umbilical metastasis. J Obstet Gynaecol. 2009;29:170-171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Poparic S, Prohic A, Kuskunovic-Vlahovljak S, Guso E, Kapetanovic A. Sister Mary Joseph Nodule in an Ovary Adenocarcinoma. Med Arch. 2017;71:154-157. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Yendluri V, Centeno B, Springett GM. Pancreatic cancer presenting as a Sister Mary Joseph's nodule: case report and update of the literature. Pancreas. 2007;34:161-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Patel KS, Watkins RM. Recurrent endometrial adenocarcinoma presenting as an umbilical metastasis (Sister Mary Joseph's nodule). Br J Clin Pract. 1992;46:69-70. [PubMed] |
| 7. | Shetty MR. Metastatic tumors of the umbilicus: a review 1830-1989. J Surg Oncol. 1990;45:212-215. [PubMed] |
| 8. | Haruki T, Nakamura H, Kubouchi Y, Taniguchi Y, Miwa K, Adachi Y, Fujioka S, Ito H. Sister Mary Joseph's nodule that originated from lung adenocarcinoma. Gen Thorac Cardiovasc Surg. 2011;59:212-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 9. | Wu YY, Xing CG, Jiang JX, Lu XD, Feng YZ, Wu HR. Carcinoma of the right side colon accompanied by Sister Mary Joseph's nodule and inguinal nodal metastases: a case report and literature review. Chin J Cancer. 2010;29:239-241. [PubMed] |
| 10. | Rahman MT, Nakayama K, Rahman M, Nakayama N, Ishikawa M, Katagiri A, Katagiri H, Ishibashi T, Iida K, Miyazaki K. Sister Mary Joseph's nodule associated with rare endometrial squamous cell carcinoma. Arch Gynecol Obstet. 2012;286:711-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |