Published online Oct 26, 2019. doi: 10.12998/wjcc.v7.i20.3347
Peer-review started: June 23, 2019
First decision: July 31, 2019
Revised: August 31, 2019
Accepted: September 11, 2019
Article in press: September 11, 2019
Published online: October 26, 2019
Processing time: 127 Days and 13.6 Hours
Breast cancer (BCa) is one of the most common malignancies in women; however, ureteral metastasis of BCa has rarely been reported in the literature.
A 55-year-old Chinese woman with an 8-year history of BCa presented with lower back pain that had persisted for 3 mo. The patient underwent bilateral modified radical mastectomy and subclavian and submandibular clearance, and received systemic treatment, including chemotherapy, radiotherapy, and targeted therapy during treatment. Ureteroscopy did not acquire a satisfactory biopsy. Thus, laparoscopic nephroureterectomy was performed, and ureteral metastases of BCa were pathologically confirmed. As suggested by her oncologist, she continued to receive apatinib. Postoperative 3-mo follow-up indicated further progression of axillary lymph node metastases.
Ureteral metastasis of BCa shows nonspecific symptoms. Diagnosing ureter metastasis from BCa can be established by histopathology and immunohistochemistry.
Core tip: Ureteral metastasis from non-urinary system tumors, such as breast cancer (BCa), has rarely been reported. Herein, we present a case of pathologically confirmed ureteral metastases of BCa.
- Citation: Zhou ZH, Sun LJ, Zhang GM. Ureter - an unusual site of breast cancer metastasis: A case report. World J Clin Cases 2019; 7(20): 3347-3352
- URL: https://www.wjgnet.com/2307-8960/full/v7/i20/3347.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i20.3347
Breast cancer (BCa) is one of the most common malignancies in women, with over 1.5 million new cases diagnosed annually worldwide[1,2]. Approximately 12% of BCa patients develop metastatic disease after surgery, with the most common metastatic sites being the bone, liver, brain, spinal cord, and lungs. Other sites of metastatic BCa colonization include the stomach, spleen, ovary, uterus, pituitary, and kidney[3]. Ureteral metastasis from non-urinary system tumors, such as BCa, has rarely been reported[4]. Herein, we present a case of pathologically confirmed ureteral metastases of BCa, providing clinical experience for its diagnosis and treatment.
A 55-year-old Chinese woman was admitted to the Department of Urology of The Affiliated Hospital of Qingdao University, complaining of lower back pain for 3 mo.
The patient’s symptoms started 3 mo ago with lower back pain. She reported no obvious gross hematuria.
Eight years prior, the patient was diagnosed with BCa and underwent left modified radical mastectomy. Histopathological results revealed infiltrating ductal carcinoma and axillary lymph node metastasis (12/15). Immunohistochemical examination revealed the following characteristics: estrogen receptor (ER) (2+), progestin receptor (PR) (3+), and HER2 (-). The tumor was defined as T2N2M0, and the patient received four cycles of the EC protocol [epirubicin: 180 mg/m3 (d1), 70 mg/m3 (d2), cyclophosphamide: 800 mg/m3 (d1)] and four cycles of the T protocol (docetaxel: 75 mg/m3), followed by radiotherapy (50 Gy; 25×). Then, the patient began to take toremifene citrate tablets (60 mg qd) and regularly revisited the hospital. Four years ago, she received subclavian and submandibular clearance when palpable masses were found on physical examination. Immunohistochemical results demonstrated that these masses were BCa metastases: ER (2+), PR (1+), HER2 (0), and P53 (3+), which were treated with six cycles of the DP protocol [docetaxel: 120 mg/m3 (d1), cisplatin: 60 mg/m3 (d1–2)] and radiotherapy (50 Gy; 20×). Then, one year ago, once again a mass was found in her right breast. She underwent right modified radical mastectomy and axillary lymph node dissection. Immunohistochemistry showed: ER (2+) and PR (2+), and she received another round of the EC and T protocols. Three months ago, she felt a mild lower back pain. A positron-emission tomography/computed tomography scan indicated progression of the axillary lymph node metastases, so the patient received targeted therapy (apatinib, 500 mg qd). After 3 mo of targeted therapy, the patient revisited the hospital for further evaluation.
The patient had no personal or family history.
No positive signs were found during physical examination.
Three consecutive urine cytological examinations found no malignant cells on smears. Several tumor markers were elevated: CEA: 6.46 ng/mL (normal 0-3.4 ng/mL), CA15-3: 38.41 U/mL (normal 0-25 U/mL), CA19-9: 105.60 U/mL (normal 0-39 U/mL), and CA125: 19.56 U/mL (normal 0.35 U/mL).
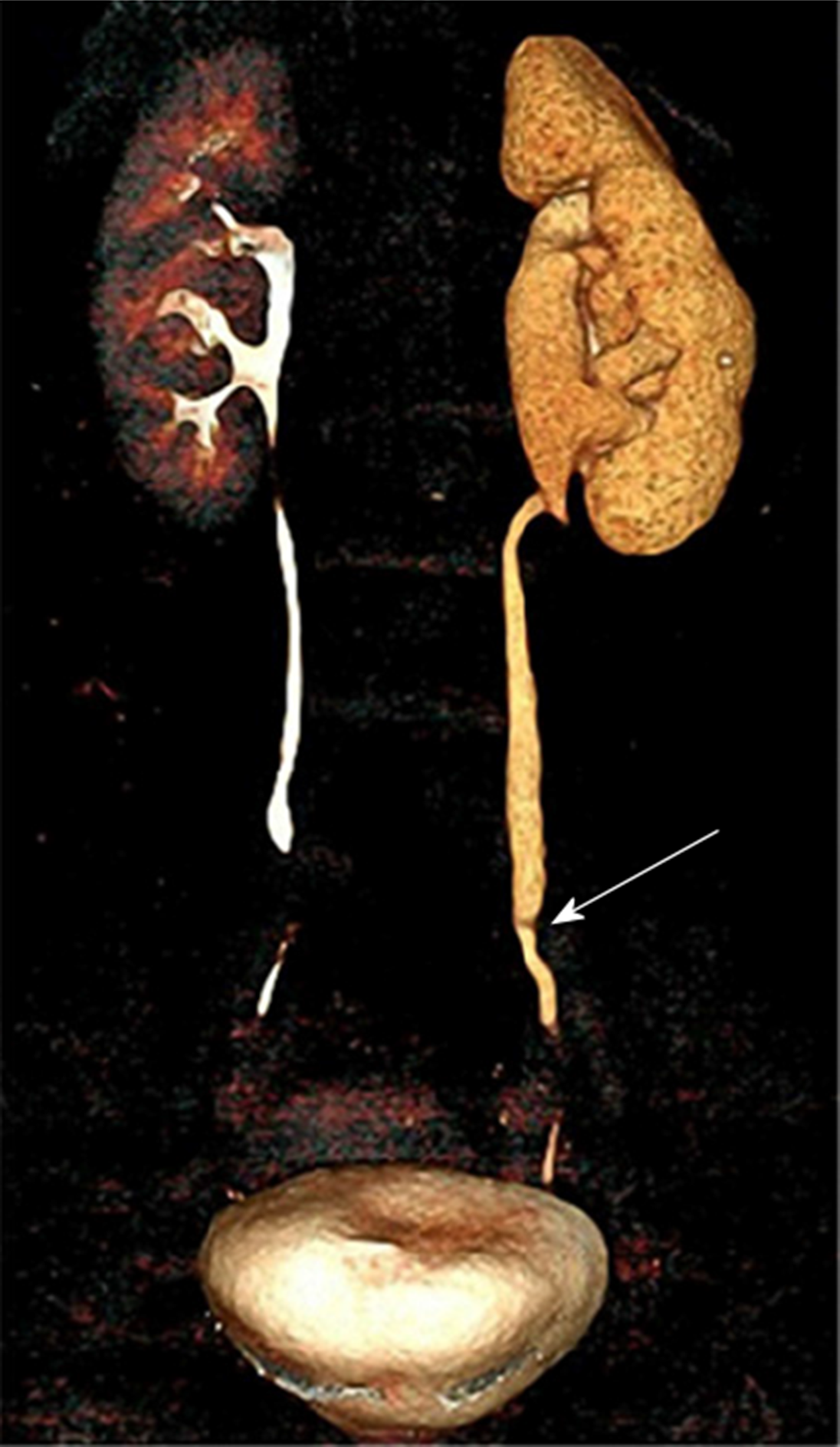
A computed tomography urography scan reported a severe obstruction in the lower left ureter segment along with left hydronephrosis (Figure 1).
The final diagnosis of the present case was ureteral urothelial carcinoma.
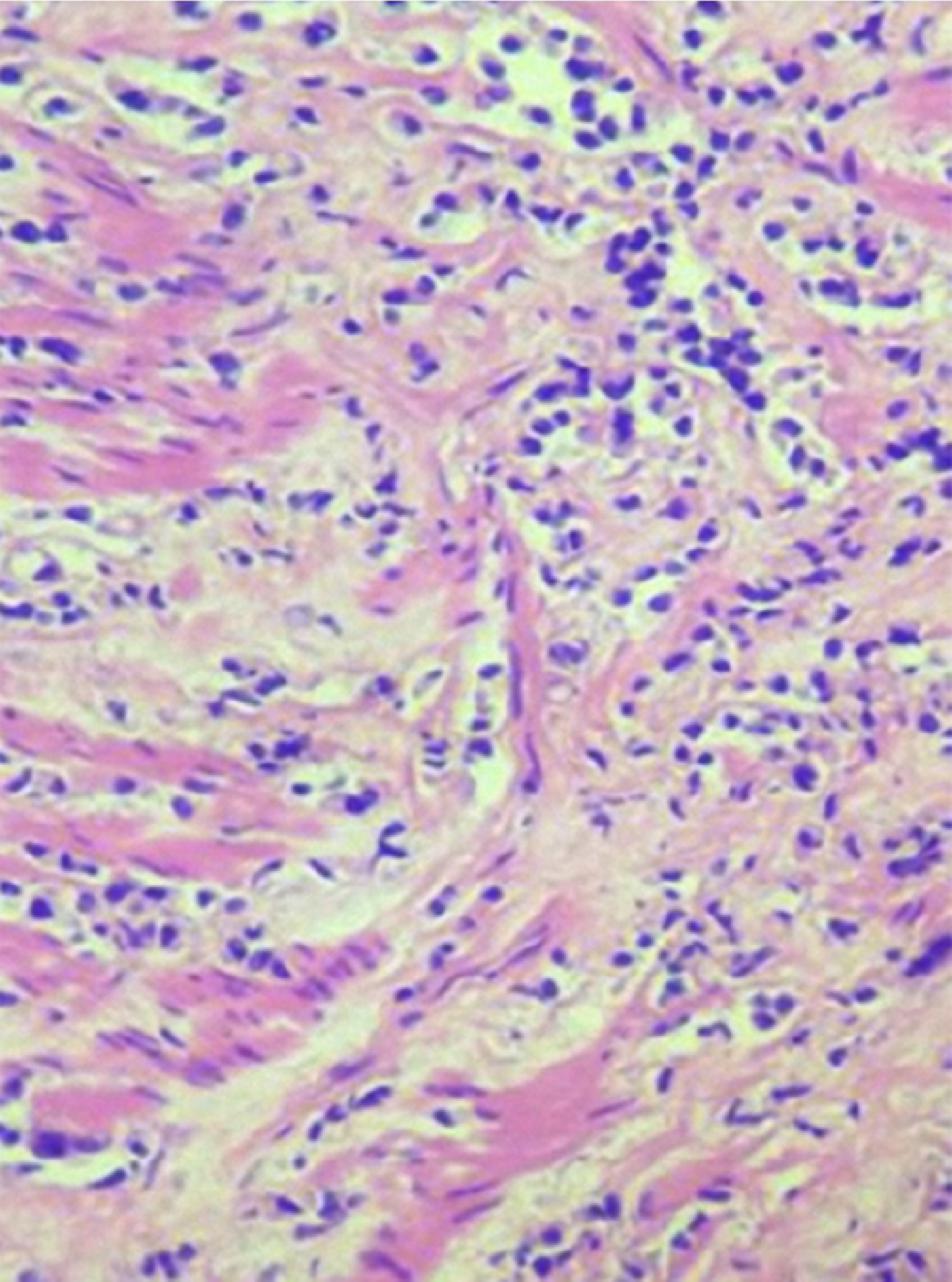
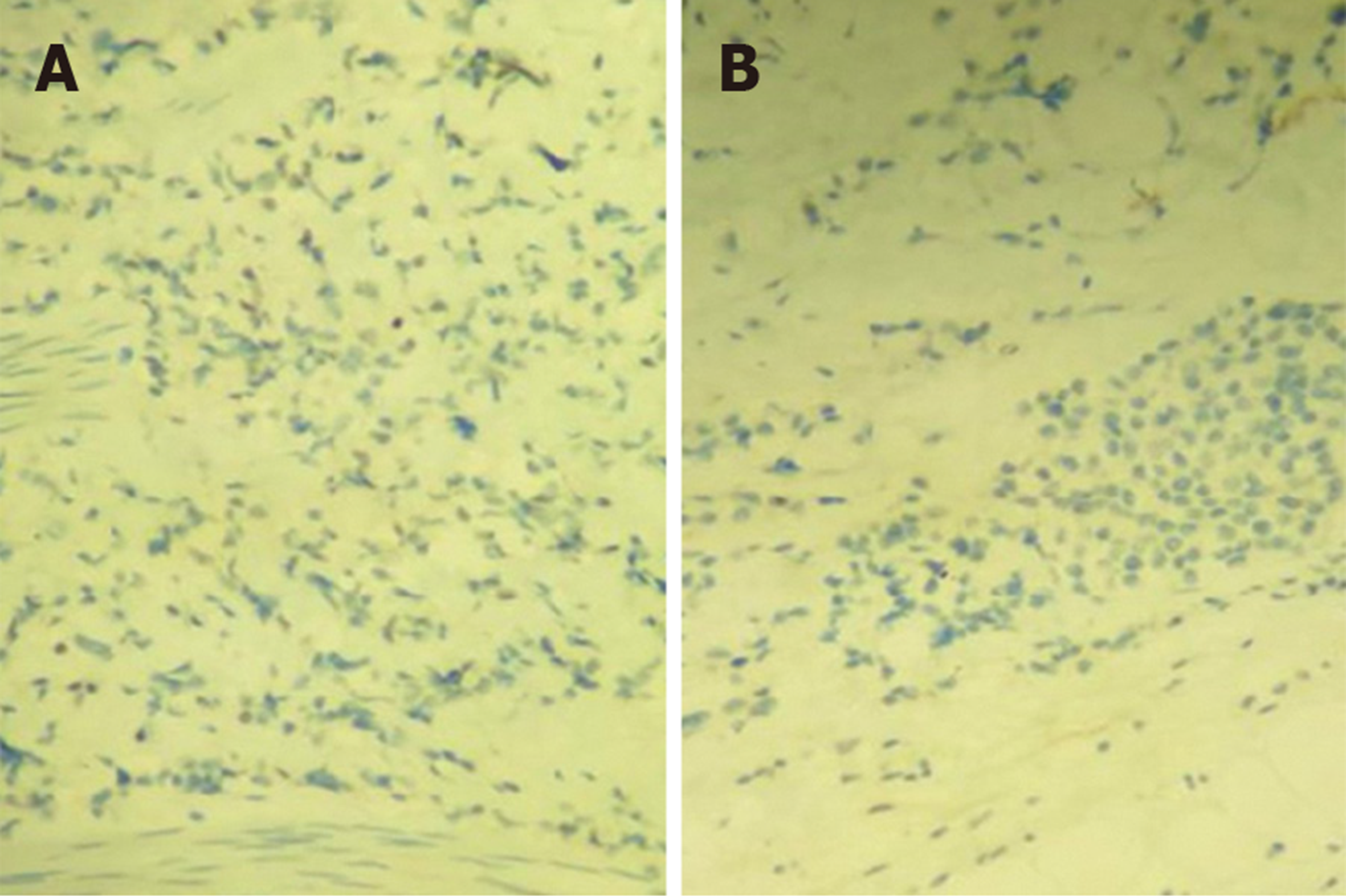
Upon admission, we first performed an ureteroscopy, and observed a stenosis (approximately 1.5 cm) that was approximately 3 cm in length from the left ureteral orifice. The wall was thick and stiff, without cauliflower-like or corpora mammillaria neoplasms, thus we did not take a biopsy. One week later, the patient underwent a laparoscopic exploratory laparotomy. During the operation, a ureteral lesion was resected for frozen histopathology, which showed that the muscular layer and tunica adventitia of the ureter were infiltrated by poorly-differentiated cancer cells. Then, a laparoscopic nephroureterectomy was performed, removing out the whole kidney and ureter. Histopathological evaluation of the resected specimen revealed that the muscular layer and tunica adventitia of the left ureter were locally infiltrated (4 mm in diameter under the microscope), without infiltration into the mucous layer of the ureter (Figure 2). There were no malignant tumors in the kidney pelvis or parenchyma. Infiltration was also found within the fibrous and adipose tissue around the porta renis (4 mm in diameter under the microscope). Immunohistochemical examination revealed the following: ER (weakly +, 10%) (Figure 3A), PR (−) (Figure 3B), HER2 (1+), Ki-67 (30%), E-Cad (+), P120 (+), GATA3 (+), GCDFP-15 (−), Mammaglobin (−), and P63 (−). Based on her medical history and these histopathological findings, the postoperative diagnosis of ureteral metastases from BCa was confirmed.
The patient had an uneventful postoperative clinical course and was discharged from hospital 6 d after the operation. As suggested by her oncologist, she continued to receive apatinib. Postoperative 3-mo follow-up indicated progression of the axillary lymph node metastases.
First reported in 1909, ureteral metastasis of any prior tumor is extremely rare[4,6]. In 1999, a total of 342 cases of ureteral metastases were collected and reviewed by Haddad et al[4]. Stomach, prostate, and bladder cancers are the most common primary malignancies to develop ureteral metastases, and BCa accounts for 7.8% of all cases[4,6]. Only a few new cases have been reported over the past 18 years[7-13].
In this case, the patient complained of a 3-mo history of lower back pain, but had no history of hematuria. Most ureteral metastases are asymptomatic, and only 36% of cases presented nonspecific systemic symptoms such as lumbar pain, nausea, urinary tract infection, or weight loss[4,14], among which, pain due to ureteral obstruction is the most frequent symptom. Hematuria is not commonly seen, because the primary tumor usually metastasizes beneath the mucosa or invades from surrounding tissues[15].
It is difficult to distinguish metastatic ureteral tumors from ureteral urothelial carcinoma. Clinical histories may provide hints; however, they are usually insufficient. Metastatic ureteral tumors tend not to adhere to the mucosa; thus, urine cytology offers little help. Presman et al[16] reported that metastatic ureteral cancers often present with several characteristics: Tumor cells in the lymph nodes and vessels around the ureter, or the same type of cells in the ureteral wall without direct invasion. Biopsy under ureteroscopy may facilitate obtaining a precise diagnosis, but it should be pointed out that because of the limited sample size, pathological diagnoses are sometimes indistinct. In this case, ureteroscopy only observed a stenosis of the ureter without a proper biopsy. Thus, exploratory laparotomy is recommended, and further clinical decisions should be made according to the pathological section when it is difficult to make a clear diagnosis by ureteroscopy.
Currently, there is no cure for metastatic BCa[3]. Surgical resection of the primary tumor or isolated metastatic lesions may be an effective therapeutic strategy. Radiotherapy can be performed to target the tumor or postsurgical tumor site[17,18]. Systemic treatment is normally added to those treatments and is based on the primary tumor or metastatic sites[19]. Chemotherapy is the most commonly used systemic treatment, and alternatives to chemotherapy include hormonal therapy, molecular-targeted therapy, immunotherapy, and recently nanotechnology and gene therapy[20].
The median survival of metastatic patients has been reported to range from 24 to 30 mo with a small percentage of them surviving a few months or a few years. With regard to metastatic site, organ diffusion, especially liver and/or soft tissues, is reported to be a predictor of poor survival[21]. In this case, the patient received targeted therapy after the progression of axillary lymph node metastases. Three months later, ureteral metastases from BCa were confirmed. Then, the metastatic lesions were resected, and postoperative 3-mo follow-up indicated further progression of the axillary lymph node metastases, indicating a relatively poor oncological outcome.
Herein, we report a rare case of ureteral metastases from BCa. Such a diagnosis is usually established by histopathology and immunohistochemistry. The nonspecific symptoms of this condition add to the difficulties of making the diagnosis. We emphasize the importance of histopathology by ureteroscopy and frozen histopathology during operation when making clinical decisions.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ghoch ME, Markic D S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Global Burden of Disease Cancer Collaboration. Fitzmaurice C, Dicker D, Pain A, Hamavid H, Moradi-Lakeh M, MacIntyre MF, Allen C, Hansen G, Woodbrook R, Wolfe C, Hamadeh RR, Moore A, Werdecker A, Gessner BD, Te Ao B, McMahon B, Karimkhani C, Yu C, Cooke GS, Schwebel DC, Carpenter DO, Pereira DM, Nash D, Kazi DS, De Leo D, Plass D, Ukwaja KN, Thurston GD, Yun Jin K, Simard EP, Mills E, Park EK, Catalá-López F, deVeber G, Gotay C, Khan G, Hosgood HD 3rd, Santos IS, Leasher JL, Singh J, Leigh J, Jonas JB, Sanabria J, Beardsley J, Jacobsen KH, Takahashi K, Franklin RC, Ronfani L, Montico M, Naldi L, Tonelli M, Geleijnse J, Petzold M, Shrime MG, Younis M, Yonemoto N, Breitborde N, Yip P, Pourmalek F, Lotufo PA, Esteghamati A, Hankey GJ, Ali R, Lunevicius R, Malekzadeh R, Dellavalle R, Weintraub R, Lucas R, Hay R, Rojas-Rueda D, Westerman R, Sepanlou SG, Nolte S, Patten S, Weichenthal S, Abera SF, Fereshtehnejad SM, Shiue I, Driscoll T, Vasankari T, Alsharif U, Rahimi-Movaghar V, Vlassov VV, Marcenes WS, Mekonnen W, Melaku YA, Yano Y, Artaman A, Campos I, MacLachlan J, Mueller U, Kim D, Trillini M, Eshrati B, Williams HC, Shibuya K, Dandona R, Murthy K, Cowie B, Amare AT, Antonio CA, Castañeda-Orjuela C, van Gool CH, Violante F, Oh IH, Deribe K, Soreide K, Knibbs L, Kereselidze M, Green M, Cardenas R, Roy N, Tillmann T, Li Y, Krueger H, Monasta L, Dey S, Sheikhbahaei S, Hafezi-Nejad N, Kumar GA, Sreeramareddy CT, Dandona L, Wang H, Vollset SE, Mokdad A, Salomon JA, Lozano R, Vos T, Forouzanfar M, Lopez A, Murray C, Naghavi M. The Global Burden of Cancer 2013. JAMA Oncol. 2015;1:505-527. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1945] [Cited by in RCA: 2051] [Article Influence: 205.1] [Reference Citation Analysis (0)] |
| 2. | Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53206] [Cited by in RCA: 55623] [Article Influence: 7946.1] [Reference Citation Analysis (131)] |
| 3. | Peart O. Metastatic Breast Cancer. Radiol Technol. 2017;88:519M-539M. [PubMed] |
| 4. | Haddad FS. Metastases to the ureter. Review of the world literature, and three new case reports. J Med Liban. 1999;47:265-271. [PubMed] |
| 5. | Stow B. IX. Fibrolymphosarcomata of Both Ureters Metastatic to a Primary Lymphosarcomata of the Anterior Mediastinum of Thymus Origin. Ann Surg. 1909;50:901-906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | López-Martínez RA, Stock JA, Gump FE, Rosen JS. Carcinoma of the breast metastatic to the ureter presenting with flank pain and recurrent urinary tract infection. Am Surg. 1996;62:748-752. [PubMed] |
| 7. | Pastore AL, Pelleschi G, Tubaro A, De Nunzio C, Stoppaciaro A, Silvestri L, Serafini GM, Stagnitti F, Carbone A. Synchronous urinary tract metastases from breast cancer. Urologia. 2009;76:66-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Nair RR, Conroy MD, Jeyarajah AR. Obstructive uropathy secondary to parametrial metastasis: an unusual presentation of breast carcinoma. Eur J Gynaecol Oncol. 2009;30:214-215. [PubMed] |
| 9. | Mondaini N, Giubilei G, Nesi G, Bongini A, Girardi LR, Ponchietti R. Carcinoma of the breast metastatic to the ureter seven years later. Int J Urol. 2005;12:763-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Hudolin T, Nola N, Milas I, Nola M, Juretic A. Ureteral metastasis of occult breast cancer. Breast. 2004;13:530-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Gialas I, Petsis D, Bogdanos I, Milathianakis K, Tsintavis A. Endoscopic diagnosis of ureteral obstruction secondary to metastatic breast carcinoma. J BUON. 2002;7:283-285. [PubMed] |
| 12. | Han LZ, Pu DM, Jin RS. Ureteral metastasis of breast cancer. Zhongguo Nongcun Weisheng. 2015;21:79. |
| 13. | Liang MJ, Zu L, Yang KR, Yang DY, Zhou Q. Ureteral metastasis of breast cancer:Case report. Zhongguo Yixue Yingxiang Jishu. 2011;27:2034. |
| 14. | Rigondet G, Salé JM, Lautier A. [Secondary tumor of the ureter. Metastasis of breast carcinoma]. Ann Urol (Paris). 1988;22:301-302. [PubMed] |
| 15. | Zhang D, Li H, Gan W. Hydronephrosis associated with ureteral metastasis of prostate cancer: A rare case report. Mol Clin Oncol. 2016;4:597-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Presman D, Ehrlich L. Metastatic tumors of the ureter. J Urol. 1948;59:312-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 71] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Lin NU, Thomssen C, Cardoso F, Cameron D, Cufer T, Fallowfield L, Francis PA, Kyriakides S, Pagani O, Senkus E, Costa A, Winer EP; European School of Oncology-Metastatic Breast Cancer Task Force. International guidelines for management of metastatic breast cancer (MBC) from the European School of Oncology (ESO)-MBC Task Force: Surveillance, staging, and evaluation of patients with early-stage and metastatic breast cancer. Breast. 2013;22:203-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Pagani O, Senkus E, Wood W, Colleoni M, Cufer T, Kyriakides S, Costa A, Winer EP, Cardoso F; ESO-MBC Task Force. International guidelines for management of metastatic breast cancer: can metastatic breast cancer be cured? J Natl Cancer Inst. 2010;102:456-463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 287] [Cited by in RCA: 283] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 19. | Sharma GN, Dave R, Sanadya J, Sharma P, Sharma KK. Various types and management of breast cancer: an overview. J Adv Pharm Technol Res. 2010;1:109-126. [PubMed] |
| 20. | Amar S, Roy V, Perez EA. Treatment of metastatic breast cancer: looking towards the future. Breast Cancer Res Treat. 2009;114:413-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Nicolini A, Giardino R, Carpi A, Ferrari P, Anselmi L, Colosimo S, Conte M, Fini M, Giavaresi G, Berti P, Miccoli P. Metastatic breast cancer: an updating. Biomed Pharmacother. 2006;60:548-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 91] [Article Influence: 4.8] [Reference Citation Analysis (0)] |