Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2905
Peer-review started: April 12, 2019
First decision: August 1, 2019
Revised: August 13, 2019
Accepted: August 26, 2019
Article in press: August 26, 2019
Published online: September 26, 2019
Processing time: 166 Days and 22.2 Hours
Bortezomib is a first-line drug approved for patients with multiple myeloma (MM) and has significantly increased their overall survival. However, bortezomib-induced peripheral neuropathy (PN) remains a significant side effect that has led to its discontinuation in some patients. Guillain-Barré syndrome (GBS) is recognized as an immune-mediated PN characterized by the involvement of multiple nerve roots and peripheral nerves and albuminocytologic dissociation in cerebrospinal fluid (CSF) tests. Intravenous immunoglobulin (IVIG) and plasmapheresis are effective.
A 45-year-old man diagnosed with stage III MM (λ type) was treated with bortezomib and dexamethasone. Fourteen days after the second course, he complained of intense burning sensation in the lower limbs and hands, loss of tactile sensation, and pain in the distal area of both thighs and in the distal part of both wrist joints. Neurological examination revealed absence of knee and ankle reflexes. CSF examination revealed albuminocytologic dissociation. Nerve conduction studies indicated sensory nerve action potential amplitudes, conduction velocity decrease, and F wave latency prolongation. He was diagnosed as MM complicated with GBS. Subsequently, he was treated with high-dose IVIG (400 mg/kg/d for five days). His symptoms fully resolved without relapse at the 6-month follow-up.
Our case highlights the differential diagnosis and management of complications after bortezomib treatment in MM.
Core tip: Multiple myeloma (MM) is a malignant clonal disease, which shortens the survival time of the patients. Bortezomib, a first-line drug for the treatment of MM, has prolonged patient survival. Therefore, the adverse reactions have become a hot topic. We can have a better understanding of its complications and treatment through this case.
- Citation: Xu YL, Zhao WH, Tang ZY, Li ZQ, Long Y, Cheng P, Luo J. Guillain-Barré syndrome in a patient with multiple myeloma after bortezomib therapy: A case report. World J Clin Cases 2019; 7(18): 2905-2909
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2905.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2905
Multiple myeloma (MM) is a malignant neoplasm with abnormal proliferation of clonal plasma cells, accounting for 10% of hematologic malignancies[1]. Chemotherapy and autologous transplantation are the major therapeutic tools for MM. Bortezomib, a first-line drug approved for patients with MM, has reduced the risk of progression or death and prolonged patient survival. A common side effect of bortezomib is peripheral neuropathy (PN). Nearly half of the patients treated with bortezomib had PN of varying degrees, and 30% had moderate to severe PN. In some patients, the symptoms did not improve after treatment. Therefore, about 10% of patients have to discontinue bortezomib treatment because they cannot tolerate the pain caused by PN[2]. About three months after withdrawal, 85% of patients did experience full relief. During follow-up after drug withdrawal, up to 30% of patients failed to have complete remission[3].
Guillain-Barré syndrome (GBS) is recognized as an immune-mediated PN characterized by involvement of multiple nerve roots and peripheral nerves, usually associated with infection. The clinical features are characterized by an acute onset, rapid progression, symmetric muscle weakness, and unstable gait. The weakness is predominantly distal, and many patients feel neuropathic pain. However, there are a number of variants in which sensory abnormalities are the main feature. Cyto-albuminological dissociation in the cerebrospinal fluid (CSF) is seen, and intravenous immunoglobulin (IVIG) therapy or plasmapheresis is effective[4,5].
In addition to bortezomib-induced PN, other factors may cause numbness in patients with MM. Herein, we present the case of a patient with MM who developed GBS after two courses of bortezomib therapy.
A 45-year-old man was hospitalized for intense burning sensation in the lower limbs and hands.
A 45-year-old man was hospitalized at the First Affiliated Hospital of Guangxi Medical University for pain in the sternum and ribs. According to the International Staging System, the patient was diagnosed with stage II MM (λ type) and stage III disease according to the Durie-Salmon Staging system. A chemotherapy protocol was followed, consisting of bortezomib (1.3 mg/m2 on days 1, 4, 8, and 11, and every 21 d thereafter), cyclophosphamide, and dexamethasone. Numbness of limbs began on the fourteenth day after the second cycle of chemotherapy. The patient began to complain of intense painful and burning sensation in the lower limbs and hands, loss of tactile sensation, and pain bilaterally in the distal parts of the thighs and bilaterally in the distal parts of the wrist joint. Gabapentin and pregabalin did not improve his symptoms.
Nothing to declare.
He have been smoking 20 cigarettes a day for more than 20 years.
The pain and tactile sensation of distal wrist joints of both upper limbs and ankle joints of both lower limbs had decreased. Knee-jerk and ankle reflexes were absent.
The blood testing results were: Hemoglobin, 139.8 g/L (normal range, 130-175.00); creatinine, 54 µmol/L (59-104); creatinine clearance, 81 mL/min (85-125); calcium, 2.13 mmol/L (2.080-2.600); albumin, 40.7 g/L, and globulin, 24.3 g/L. The 24-h urine analysis showed a total protein of 84.6 mg/24 h (0.0-120.0). Serum lactate dehydrogenase was 247 U/L (109-245) and beta-2 microglobulin was 3.03 µg/mL (0.0-120.0). Serum immunoelectrophoresis showed no M protein band. Serum free light chain assay showed free light chain κ of 11.11 mg/L and free light chain λ of 21.69 mg/L. Folic acid and vitamin B12 levels were normal. Bone marrow had 3% plasma cells.
CSF pressure was 124 mmH2O, CSF protein was 931.1 mg/L (150-450), and CSF cell count was 0 × 106/L. CSF syphilis antibody and Cryptococcus neoformans were negative. Paraneoplastic antibodies in CSF and serum were negative, which included anti-Hu, Yo, Ri, CV2, Ma2/Ta, amphiphysin, ANNA3, Tr, PCA2, and GAD.
Nerve conduction studies: The sensory conduction velocity and amplitude of the median nerve and ulnar nerve were normal bilaterally, and the motor conduction velocity and amplitude were also normal. The latency and occurrence rate of F wave in the median nerve and bilateral ulnar nerve were normal bilaterally. The latency of F wave in the tibial nerve was prolonged bilaterally and the rate of occurrence was normal. The tibial nerve H reflex could not be induced bilaterally. The sensory potentials of both superficial peroneal nerves and both sural nerves could not be induced. The conduction velocity and amplitude of the common peroneal nerve and the tibial nerve were normal. No spontaneous potential was found in the right anterior tibial electromyography. The time limit was prolonged, the amplitude was increased, and the multiple waves were normal. No spontaneous potential was found in the left anterior tibial muscle, bilateral gastrocnemius muscle, or right medial femoral head muscle. The time limit, amplitude, and multiple waves were normal, and the maximum force was mixed. There was no spontaneous potential in the EMG of the right first interphalangeal muscle and the right biceps brachii. The time limit, amplitude, and multiple waves were normal, and the maximum force was mixed.
Mild to moderate multiple sensory neuron damage could be considered.
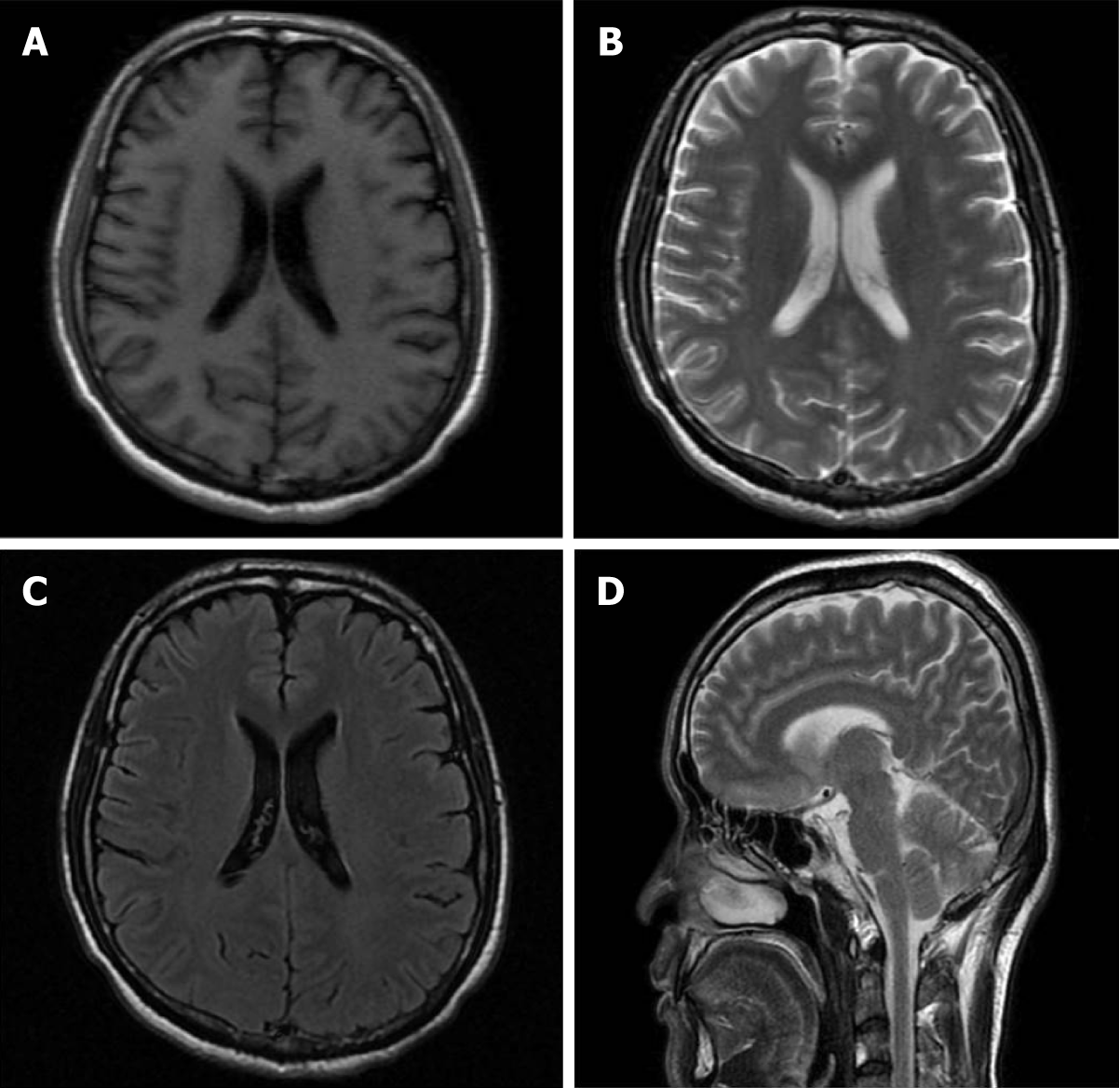
The imaging findings are presented in Figure 1.
MM complicated with GBS.
The patient was treated with high-dose IVIG (400 mg/kg/d for five days).
The symptoms improved partially, and CSF proteins returned to normal after four weeks. At the 6-mo follow-up, he had complete symptom remission.
GBS is one of the most common causes of acute flaccid paralysis, characterized by symmetrical limb weakness and sensory abnormalities. These usually begin at the distal end and appear in a symmetrical pattern, causing decreased or absent reflexes, and usually reach the peak within four weeks. The most common subtypes are acute inflammatory demyelinating polyneuropathy and acute motor axonal neuropathy, among other variants. The pathogenesis of GBS is mainly related to immune-mediated demyelination or axonal degeneration[5,6]. The pathogenesis is still not clear.
In fact, PN can occur before and after bortezomib treatment. Our patient was diagnosed with MM. Since PN ensued only after two cycles of bortezomib treatment, the following aspects were considered. First, polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, and skin changes (POEMS) syndrome caused by MM is a possibility. In our case, after two cycles of chemotherapy, the burden of myeloma and bone marrow plasma cells were reduced, there were no skin lesions or hepatosplenomegaly, endocrine tests were negative, and M protein was not detected; therefore, POEMS syndrome was excluded. The second possibility is paraneoplastic syndrome caused by MM, which refers to the production of paraneoplastic antibodies in tumor patients, mediating the destruction of peripheral nerve lesions. Plasma cell tumors are closely associated with PN caused by paraneoplastic syndrome, especially in MM. Research shows that about 20% of patients with MM have neuropathy before treatment, which may be related to a primary disease[2]. Paraneoplastic antibodies were negative and myeloma burden was relieved, so PN caused by paraneoplastic syndrome was not considered. Finally, it may be PN caused by bortezomib, or other neurological diseases. The patient developed numbness and pain at the end of the second course of treatment. No significant improvement was found after analgesic treatment and the patient continued to complain about intolerable pain and poor quality of life. A combination of elevated protein levels and normal cell counts in the CSF was indicative of GBS. Fortunately, the patient experienced relief after IVIG treatment.
In 1987, the first case of MM with kappa light chain combined with GBS was reported[7]. In 2008, Iqbal et al[8] also reported five patients with MM complicated by GBS, three of whom developed GBS after transplantation, one received dexamethasone combined with lenalidomide treatment, and one developed GBS without treatment. Subsequently, MM combined with GBS was reported after bone-marrow transplantation[9,10].
Although bortezomib associated GBS is rare, MM with GBS after bortezomib therapy has been reported. Philippe Moreau et al[11] in 2017 compared the safety and efficacy of venetoclax plus bortezomib and dexamethasone in relapsed/refractory MM. Before enrollment, a patient with MM complicated by GBS was considered, which was possibly related to bortezomib.
With the emergence of bortezomib, the prognosis of patients with MM has been improved. In addition, more and more attention has been paid to adverse drug reactions and treatment. This case report suggests that the treatment of MM with bortezomib can simultaneously aggravate GBS.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mesquita J S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Moreau P, Chanan-Khan A, Roberts AW, Agarwal AB, Facon T, Kumar S, Touzeau C, Punnoose EA, Cordero J, Munasinghe W, Jia J, Salem AH, Freise KJ, Leverson JD, Enschede SH, Ross JA, Maciag PC, Verdugo M, Harrison SJ. Promising efficacy and acceptable safety of venetoclax plus bortezomib and dexamethasone in relapsed/refractory MM. Blood. 2017;130:2392-2400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 179] [Cited by in RCA: 214] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 2. | Park SB, Goldstein D, Krishnan AV, Lin CS, Friedlander ML, Cassidy J, Koltzenburg M, Kiernan MC. Chemotherapy-induced peripheral neurotoxicity: a critical analysis. CA Cancer J Clin. 2013;63:419-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 458] [Cited by in RCA: 512] [Article Influence: 42.7] [Reference Citation Analysis (0)] |
| 3. | Argyriou AA, Cavaletti G, Bruna J, Kyritsis AP, Kalofonos HP. Bortezomib-induced peripheral neurotoxicity: an update. Arch Toxicol. 2014;88:1669-1679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 4. | van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA. Guillain-Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol. 2014;10:469-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 525] [Cited by in RCA: 679] [Article Influence: 61.7] [Reference Citation Analysis (2)] |
| 5. | Willison HJ, Jacobs BC, van Doorn PA. Guillain-Barré syndrome. Lancet. 2016;388:717-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 778] [Cited by in RCA: 893] [Article Influence: 99.2] [Reference Citation Analysis (0)] |
| 6. | Yuki N, Hartung HP. Guillain-Barré syndrome. N Engl J Med. 2012;366:2294-2304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 786] [Cited by in RCA: 774] [Article Influence: 59.5] [Reference Citation Analysis (0)] |
| 7. | Mactier RA, Khanna R. Guillain-Barré syndrome in kappa light chain myeloma. South Med J. 1987;80:1054-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Iqbal AN, Le Q, Motiwala R, Clay LJ, Motiwala T, Lendvai N, Siegel DS, Goldberg SL. Guillain-Barre syndrome complicating multiple myeloma. Blood. 2008;112:5135. |
| 9. | Biran N, Rowley SD, Vesole DH, Zhang S, Donato ML, Richter J, Skarbnik AP, Pecora A, Siegel DS. A Phase I/II Study of Escalating Doses of Bortezomib in Conjunction with High-Dose Melphalan as a Conditioning Regimen for Salvage Autologous Peripheral Blood Stem Cell Transplantation in Patients with Multiple Myeloma. Biol Blood Marrow Transplant. 2016;22:2165-2171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Zhang L, Arrington S, Keung YK. Guillain-Barré syndrome after transplantation. Leuk Lymphoma. 2008;49:291-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Moreau P, San Miguel J, Sonneveld P, Mateos MV, Zamagni E, Avet-Loiseau H, Hajek R, Dimopoulos MA, Ludwig H, Einsele H, Zweegman S, Facon T, Cavo M, Terpos E, Goldschmidt H, Attal M, Buske C; ESMO Guidelines Committee. Multiple myeloma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28:iv52-iv61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 500] [Cited by in RCA: 478] [Article Influence: 59.8] [Reference Citation Analysis (0)] |