Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2899
Peer-review started: March 28, 2019
First decision: May 13, 2019
Revised: July 23, 2019
Accepted: July 27, 2019
Article in press: July 27, 2019
Published online: September 26, 2019
Processing time: 182 Days and 12.7 Hours
Pleomorphic lipoma (PL) is a rare benign mesenchymal tumor occurring predominantly in middle-aged and elderly men. It is typically found in the subcutaneous tissue of the posterior neck, back, and shoulders. There have also been a few reported cases in the face, scalp, and upper extremities. Currently, there is no report on its occurrence in the anterior mediastinum.
Herein, we report the case of a 67-year-old woman diagnosed with PL in the anterior mediastinum. The tumor was removed by thoracoscopic surgery. There was no recurrence during the 24-mo follow-up period, and the prognosis was good. Most PL are located on the skin surface. However, they may also occur within the body, even in the mediastinum.
PL occurring in the anterior mediastinum is rare, and it may be differentiated from other tumors.
Core tip: Pleomorphic lipoma (PL) primarily occur in the superficial subcutaneous compartments of the neck, shoulders, and back. This unusual neoplasm has also been documented in the tongue, orbit, bulbar conjunctiva, parotid gland, oral cavity, dermis, scalp, and breasts. Currently, there is no report on its occurrence in the anterior mediastinum. Therefore, the clinical features and treatment of anterior mediastinal PL are limited.
- Citation: Mao YQ, Liu XY, Han Y. Pleomorphic lipoma in the anterior mediastinum: A case report. World J Clin Cases 2019; 7(18): 2899-2904
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2899.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2899
Pleomorphic lipoma (PL) is clinically similar to spindle-cell lipoma, with diameters ranging from 1 to 13 cm. Most PL are generally slow-growing, but a short-term growth spurt may occur in some cases. Although both pleomorphic and spindle-cell lipomas show aberrations in nuclear chromosome 16q, PL with such a change are still considered benign[1]. Histopathologically, there are well-defined borders between the tumor and surrounding tissues. Tumor cells are highly pleomorphic. Although areas of mature adipocytes are present, most adipocytes vary in sizes, and lipoblasts or vacuolated cells are present in approximately half of the tumors. They exist in small amounts in the myxoid stroma that is traversed by a large amount of dense, interlacing collagen bundles. The tumor cells may have multiple overlapping nuclei or may be arranged into floret-like giant cells, mitosis is rare, and there is no necrosis. A diagnosis can be made based on the clinical manifestations, characteristics of skin lesions, and histopathology. Surgical tumor resection is associated with a good prognosis[2]. Herein, we report a case of PL that occurred in the anterior mediastinum.
Multiple joint swelling for 10 years, which was aggravated for 1 year.
The patient was a 67-year-old woman who experienced bilateral knee swelling and pain 10 years ago without apparent cause and was diagnosed with rheumatoid arthritis at a local hospital. She treated herself with over-the-counter oral anti-rheumatic drugs. In the past year, the joint swelling and pain gradually worsened and affected the entire body, mainly involving the bilateral joints of the hands, knees, wrists, and shoulders. The swelling and pain were slightly more serious on bilateral shoulder joints and right knee. In addition, the patient had dry eyes and mouth and should drink water when eating dried food. She was then presented to Division of Rheumatology and Immunology. According to laboratory testing results, she was diagnosed with rheumatoid arthritis. Computed tomography (CT) revealed an anterior mediastinal tumor. She was subsequently transferred to the Department of Thoracic Surgery for surgical treatment.
Ten years of hypertension, without any medical treatment; systolic blood pressure 150 -160 mmHg, and diastolic blood pressure 95-105 mmHg.
There was no remarkable family history of related diseases.
Multiple joint swelling.
Laboratory testing results were as follows: SS-A, weakly positive; erythrocyte sedimentation rate, 39 mm/h; antinuclear antibody, 1:320 (+); immunoglobulin G, 17.10 g/L; immunoglobulin M, 2.58 g/L; C-reactive protein, 11.10 mg/L; and rheumatoid factor, 941 IU/mL.
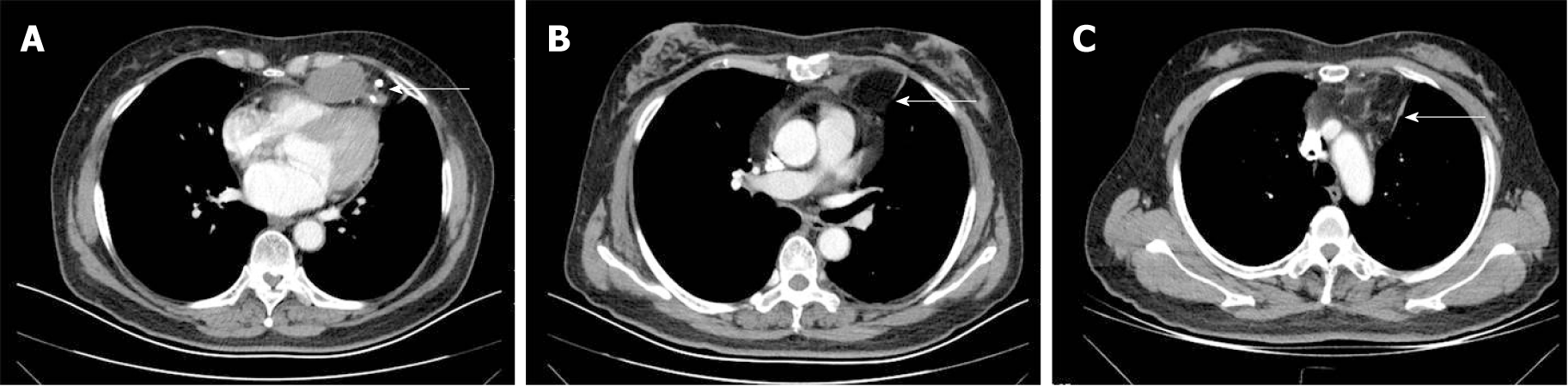
Chest CT showed a shadow of dense fat visible in the anterior mediastinum. Multiple fat-dense nodules of varying sizes were observed, with a maximum diameter of 44 mm × 28 mm. Calcification was observed around some nodules. No enhancement was seen on enhanced CT (Figure 1).
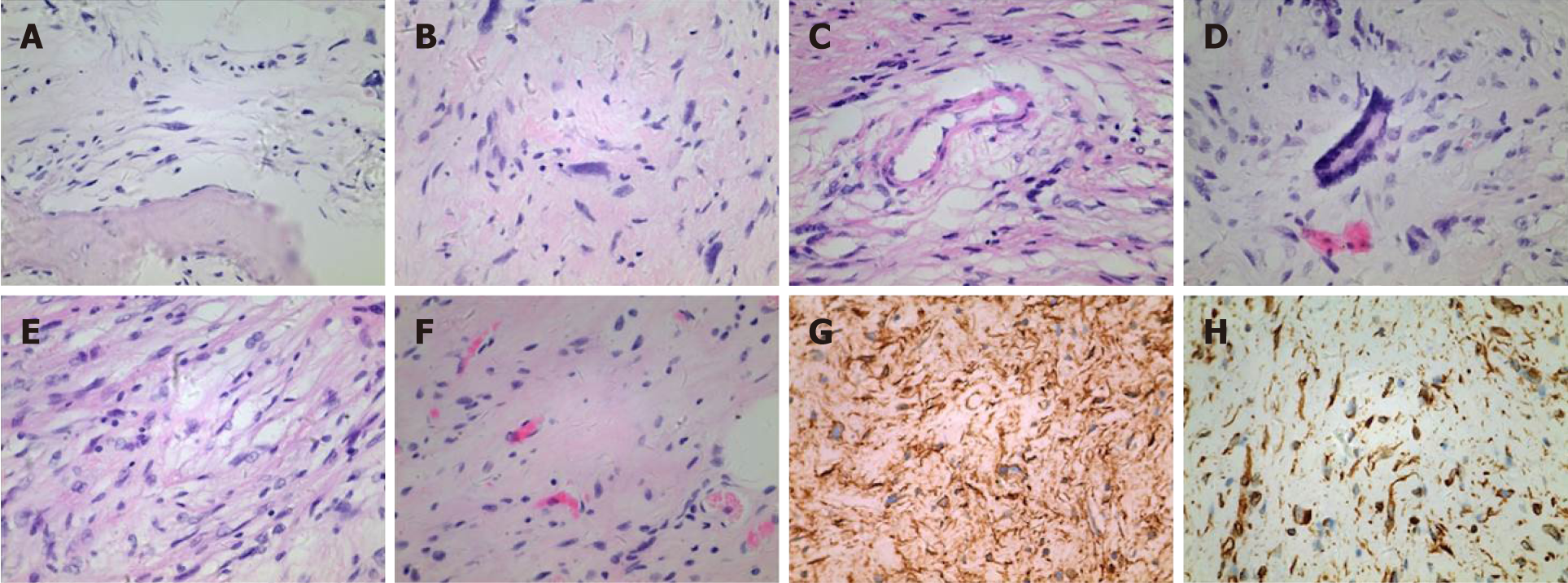
The border of the tumor and tissue was well-defined. The cut surface was grayish white or grayish yellow. The tumor had a soft to firm texture depending on the fat contents. Microscopically, the tumor cells were highly pleomorphic. Mature adipocyte areas admixed with spindle cells were observed. Some nuclei were mildly atypical. Floret-like giant cells were observed, and focal calcification was present. Thick-walled blood vessels were visible. Spindle cells with mild nuclear atypia and hyperchromatic nuclei were observed. The results of immunohistochemical analysis were CD117 (-), Dog-1 (-), S-100 (partial +), SMA (partial +), CK (-), desmin (-), vimentin (+), Ki67 (5%), CD34 (+), and CD68 (-) (Figure 2).
Anterior mediastinal PL.
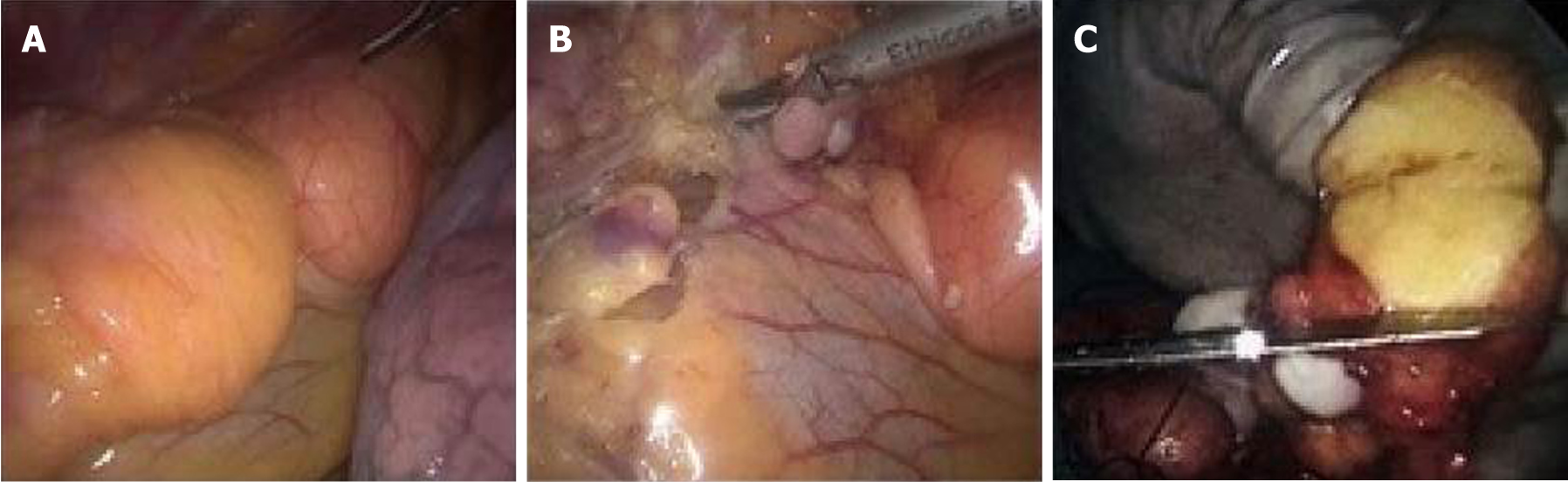
The tumor was resected by right thoracoscopic surgery assisted by artificial pneumothorax under single-lumen endotracheal tube anesthesia. Multiple solid and cystic mixed masses were visible during intraoperative examination of the anterior middle mediastinum in front of the pericardium. The larger mass was almost 44 mm in diameter. The surface was covered with fats, and the mass was well encapsulated. However, it adhered to the pericardium, and the adhesion was excessively dense for complete resection. When an ultrasonic scalpel was used to separate the tumor from the pericardium, part of the pericardium had to be removed because of severe adhesion. The tumors in the anterior superior mediastinum contained more fats that facilitated the separation. The pathology of the intraoperative frozen section was “mesenchymal tumor”. The tumor was well encapsulated, and the surface was smooth. The tumor was moderately soft. The cut surface was grayish yellow or grayish white and free from hemorrhage and necrosis (Figure 3). The drainage tube was removed 3 d after surgery, and the patient was discharged 5 d later. Postoperative pathology report indicated (mediastinal) PL.
She was followed by chest CT every 3 mo. There was no recurrence in the 24-mo follow-up period.
PL is a benign mesenchymal tumor that was first reported by Shmookler et al[3] in 1981. In the 2013 World Health Organization classification of tumors of bone and soft tissue, PL and spindle cell lipoma were classified as the same type of adipocytic tumor[4,5]. Both tumor types show aberrations in nuclear chromosome 16q. Their clinical manifestations are also similar: The male-to-female incidence ratio is approximately 4:1, age at onset is 50 years or above, and they primarily occur in the superficial subcutaneous compartments of the neck, shoulders, and back. This unusual neoplasm has also been documented in the tongue, orbit, bulbar conjunctiva, parotid gland, oral cavity, dermis, scalp, and breasts[6]. In the present case, the patient discovered the disease a year ago, and there was no change in the tumor during the 1-year follow-up period. There is currently no report of PL in the anterior mediastinum. The presented case showed findings consistent with the characteristics of benign mediastinal tumors. The tumor grew slowly toward the direction of the thorax, and the patient did not display any symptoms even if the tumor had grown into a considerable size.
PL generally have well-defined borders. They are mostly round, oval, or nodular and are fully encapsulated. The cut surfaces appear yellow, grayish yellow, or grayish white. The texture in some focal areas may be firmer and rubberier than the usual lipomas. In the present case, the three main tumors were 1.5 cm to 4.5 cm in diameter and were well encapsulated. The cut surfaces were grayish white and grayish yellow. The texture varied from soft to rubbery because of the differences in fat contents. Focal mass exhibited a firm texture, which is consistent with the focal calcification of the tumor edge observed in the preoperative chest CT. However, the adhesion of the tumor to the pericardium during surgery is inconsistent with previous reports, which described well-defined borders between the tumor and tissues. This might be related to the calcification of the tumor[4]. The tumor cells were highly pleomorphic. Although areas of mature adipocytes were present, most adipocytes varied in sizes, and lipoblasts or vacuolated cells were present in approximately half of the tumors. They existed in small amounts in the myxoid stroma that was traversed by a large amount of dense, interlacing collagen bundles. The most characteristic feature of the tumor cells was large, multinucleated, bizarre giant cells with their nuclei densely arranged along the periphery of the cells with “floret-like” morphology. These giant cells were interspersed in the fibrous septa or myxoid matrix. In addition, a large number of interlacing, rope-like, matured collagen fiber bundles were also observed[3]. The history of the present case also showed a typical “floret-like” change. Immunophenotypically, spindle cells admixed with the tumor cells expressed CD34, and cells with significant differentiation toward adipocytes expressed the S-100 protein[7].
Differential diagnoses mainly concluded liposarcoma; of the 48 patients reported by Shmookler et al[3], 31 were diagnosed with or suspected to have liposarcoma. Liposarcoma has been reported to occur in the thoracic cavity[8]. From the imaging perspective, the deeper areas of a fat-dense mass in liposarcoma may appear as a septal or higher-than-muscle-dense mass, with enhancement observed by enhanced CT. However, PL remains as a fat-dense shadow even with an enhanced scan, and no enhancement can be observed.
Although focally pleomorphic liposarcoma (PLS) is similar to PL in that it contains large portions of giant cells (floret-like cells), atypical lipoblasts are also present at each developmental stage of PLS. Furthermore, PLS tumors are basically free from mucous components. On the contrary, PL presents with almost no mitosis, hemorrhage, or necrosis, which is significantly different from PLS[9].
In the present case, the tumor occurred in the anterior mediastinum. Enhanced CT is an important method for diagnosing mediastinal tumors. The most common tumors of the anterior mediastinum are thymomas, teratomas, and substernal goiters, which are usually enhanced in enhanced CT. In the present case, the PL displayed variably sized, soft-tissue-dense nodules in the anterior mediastinum. No enhancement from the enhanced CT was observed. The mean CT value was 27, which could be identified by imaging[10].
In conclusion, the lipoma reported here occurred in multiple sites in the mediastinum, which might be due to the relatively large space and loose tissue organization of the anterior mediastinum. Although PL chiefly occurs in superficial compartments, there is no report of malignant transformation and metastasis of PL. However, in this case, some of the mature adipocytes were slightly atypical, and the tumors were located in deep tissues. In addition, ki67 index was 5%. Thoracoscopy was used to resect the tumors. Moreover, the anterior mediastinal fat surrounding the tumors was removed according to the surgical criteria for low-grade malignant tumors. There was no recurrence in the 24-mo follow-up period. Furthermore, long-term follow-up is required to monitor for the possibility of relapse.
We thank the Department of Thoracic Surgery of Shengjing Hospital of China Medical University for technical assistance.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anand A, Peitsidis P S-Editor: Cui LJ L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Hinds B, Agulló Pérez AD, LeBoit PE, McCalmont TH, North JP. Loss of retinoblastoma in pleomorphic fibroma: An immunohistochemical and genomic analysis. J Cutan Pathol. 2017;44:665-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Shi BJ, Jiang X, Xiao YJ, Wang SP, Hao J, Diao QC. Intradermal spindle cell/pleomorphic lipoma: Case report and review of the literature. Indian J Dermatol Venereol Leprol. 2017;83:692-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Shmookler BM, Enzinger FM. Pleomorphic lipoma: a benign tumor simulating liposarcoma. A clinicopathologic analysis of 48 cases. Cancer. 1981;47:126-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Weiss SW, Goldblum JR. Enzinger and Wei ss' s soft ti ssue tumors. Elsevier Science: Health Science Asia 2002; 597-601. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Eggleston PA, Kagey-Sobotka A, Lichtenstein LM. A comparison of the osmotic activation of basophils and human lung mast cells. Am Rev Respir Dis. 1987;135:1043-1048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 505] [Cited by in RCA: 669] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 6. | Wang L, Liu Y, Zhang D, Zhang Y, Tang N, Wang EH. A case of 'fat-free' pleomorphic lipoma occurring in the upper back and axilla simultaneously. World J Surg Oncol. 2013;11:145. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Suster S, Fisher C. Immunoreactivity for the human hematopoietic progenitor cell antigen (CD34) in lipomatous tumors. Am J Surg Pathol. 1997;21:195-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 116] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Lin F, Pu Q, Ma L, Liu C, Mei J, Liao H, Guo C, Liu L. Successful resection of a huge mediastinal liposarcoma extended to the bilateral thorax. Thorac Cancer. 2016;7:373-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Lin XY, Wang Y, Liu Y, Sun Y, Miao Y, Zhang Y, Yu JH, Wang EH. Pleomorphic lipoma lacking mature fat component in extensive myxoid stroma: a great diagnostic challenge. Diagn Pathol. 2012;7:155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Romeo V, Esposito A, Maurea S, Camera L, Mainenti PP, Palmieri G, Buonerba C, Salvatore M. Correlative Imaging in a Patient with Cystic Thymoma: CT, MR and PET/CT Comparison. Pol J Radiol. 2015;80:22-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |