Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2879
Peer-review started: April 8, 2019
First decision: June 19, 2019
Revised: June 23, 2019
Accepted: July 20, 2019
Article in press: July 20, 2019
Published online: September 26, 2019
Processing time: 171 Days and 7.3 Hours
Laparoscopic pancreatoduodenectomy (LPD) has been developed gradually with the advances in surgical laparoscopic techniques. It is technically challenging to perform LPD with portal vein resection and reconstruction.
A 71-year-old female patient was diagnosed with distal cholangiocarcinoma. After preoperative examination and rigorous preoperative preparation, the patient underwent LPD using 3D laparoscopy on July 17, 2018. During the surgery, we found that the tumor invaded the right wall of the portal vein; thus, pancreaticoduodenectomy combined with partial portal vein wall resection was performed. The defect of the portal vein wall was approximately 2.5 cm × 1.0 cm. The hepatic ligamentum teres was excised by laparoscopy and then recanalized in vitro. Following recanalization, the hepatic ligamentum teres was cut longitudinally and then trimmed into vascular patches that were then used to reconstruct the defect of the portal vein through 3D laparoscopy. The operative time was 560 min, and intraoperative blood loss was 100 mL. The duration of the blood occlusion time was 63 min. No blood transfusion was required. The patient underwent enhanced recovery after surgery procedures after the operation. The patient was discharged on postoperative day 11. Follow-up for 6 months after discharge showed no stenosis of the portal vein and good patency of blood flow.
It is safe and feasible to use the hepatic ligamentum teres patch to repair portal vein in LPD. However, the long-term patency of this technique for venous reconstruction requires further investigation.
Core tip: We report a patient with distal cholangiocarcinoma that invaded the portal vein who was treated by laparoscopic pancreatoduodenectomy and using the hepatic ligamentum teres patch to repair the portal vein by laparoscopy. Use of the hepatic ligamentum teres patch to repair and reconstruct the portal vein/superior mesenteric vein by laparoscopy is difficult and complicated. It was confirmed that laparoscopic treatment of tumors that invade the portal vein or superior mesenteric vein is safe and feasible. Furthermore, the application of the hepatic ligamentum teres patch in the reconstruction of abdominal blood vessels was further expanded and reduced the incidence of transabdominal operation.
- Citation: Wei Q, Chen QP, Guan QH, Zhu WT. Repair of the portal vein using a hepatic ligamentum teres patch for laparoscopic pancreatoduodenectomy: A case report. World J Clin Cases 2019; 7(18): 2879-2887
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2879.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2879
Pancreatoduodenectomy (PD) is an operative method for the treatment of distal cholangiocarcinoma, pancreatic head cancer, and periampullary carcinoma, as well as other diseases. In recent years, laparoscopic pancreatoduodenectomy (LPD) has been developed gradually with the advances in surgical laparoscopic techniques. When the tumor invades the portal vein or superior mesenteric vein, LPD with vascular resection can also be safely performed to achieve radical resection. However, few cases have been reported concerning this technique, due to the lack of experience. Recently, we successfully performed LPD combined with portal vein resection and repaired the vessel using the hepatic ligamentum teres patch for a patient with distal cholangiocarcinoma that invaded the portal vein.
A 71-year-old female patient was admitted to the hospital for 6 d with upper abdominal discomfort and loss of appetite.
The patient’s symptoms started 6 d previously; she described the abdominal discomfort located in the right upper abdominal, and loss of appetite. On admission, she denied any fever, nausea, vomit, chest pain, or shortness of breath.
In the past, the woman was in good health.
The patient had no relevant personal or family history.
The skin and sclera showed mild jaundice, the abdomen was soft, and no abdominal tenderness was felt. The liver was touched at the end of the inferior margin, the gallbladder could be reached, the size was approximately 3 cm × 2 cm, and no tenderness was felt. The Murphy sign was negative.
Initial laboratory testing included a complete blood count, biochemistry index, and urinalysis. The patient had high levels of ALT (185.60 U/L), AST (58.90 U/L), DBIL (12.70 μmol/L), ALP (326.80 U/L), and CA19-9 (81.70 U/mL), but WBC, HGB, PTL, and GLU were in the range of normal values.
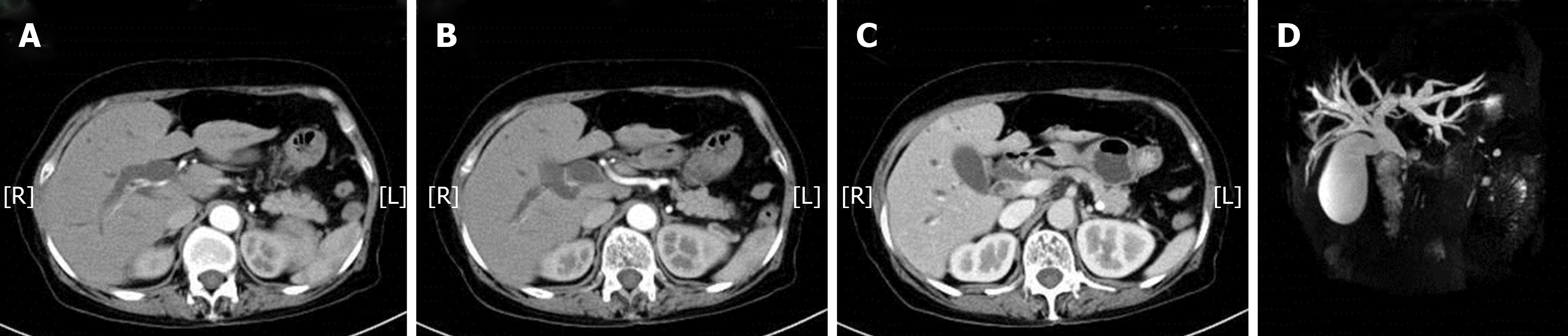
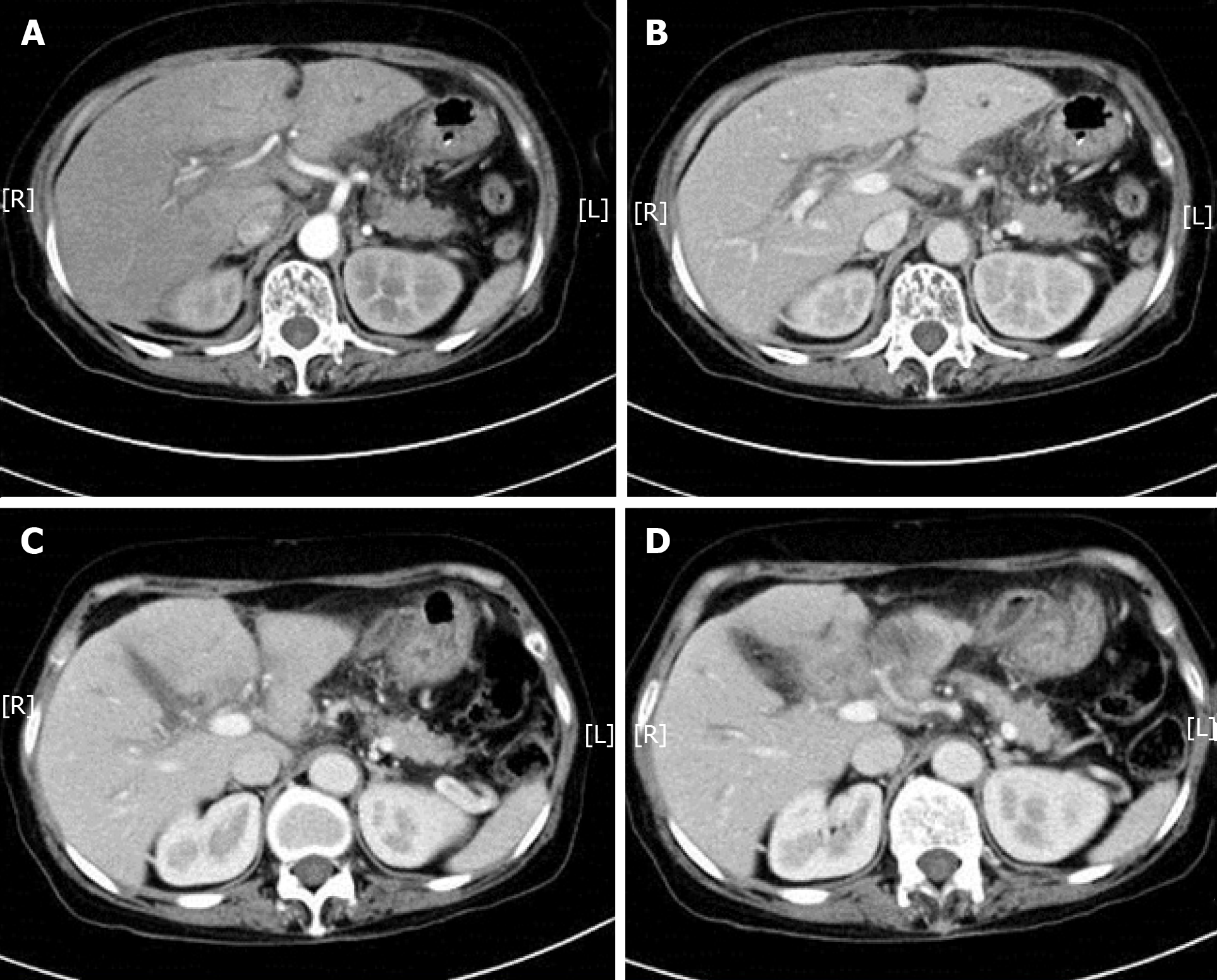
The upper computed tomography (CT) plain scan and enhanced scan showed the following aspects: the lower common bile duct wall was thickened, and the lumen was narrow. The upper common bile duct and intrahepatic bile duct were dilated, the gallbladder was enlarged, and there was no obvious shadow with abnormal density in the upper part of the common bile duct. Magnetic resonance cholangiopancreato-graphy showed that the lumen of the pancreatic segment of the common bile duct was obviously narrow, resulting in dilatation of the upper intrahepatic and extrahepatic bile ducts, and the gallbladder volume was larger (Figure 1). The diagnosis of obstructive jaundice was based on analysis of the medical history, symptoms and signs of the patient, as well as the auxiliary examination report. Considering the high possibility of cholangiocar-cinoma, the indications for operative treatment was also highly probable.
Before the operation, magnesium isoglycyrrhizinate was administered to protect the liver, enteral nutritional supplements were also orally administered, and other related procedures of the enhanced recovery after surgery (ERAS) were carried out at our hospital during the perioperative period. After the active preoperative preparation, the patient underwent 3D laparoscopy on July 17, 2018. The operation was performed using five trocars.
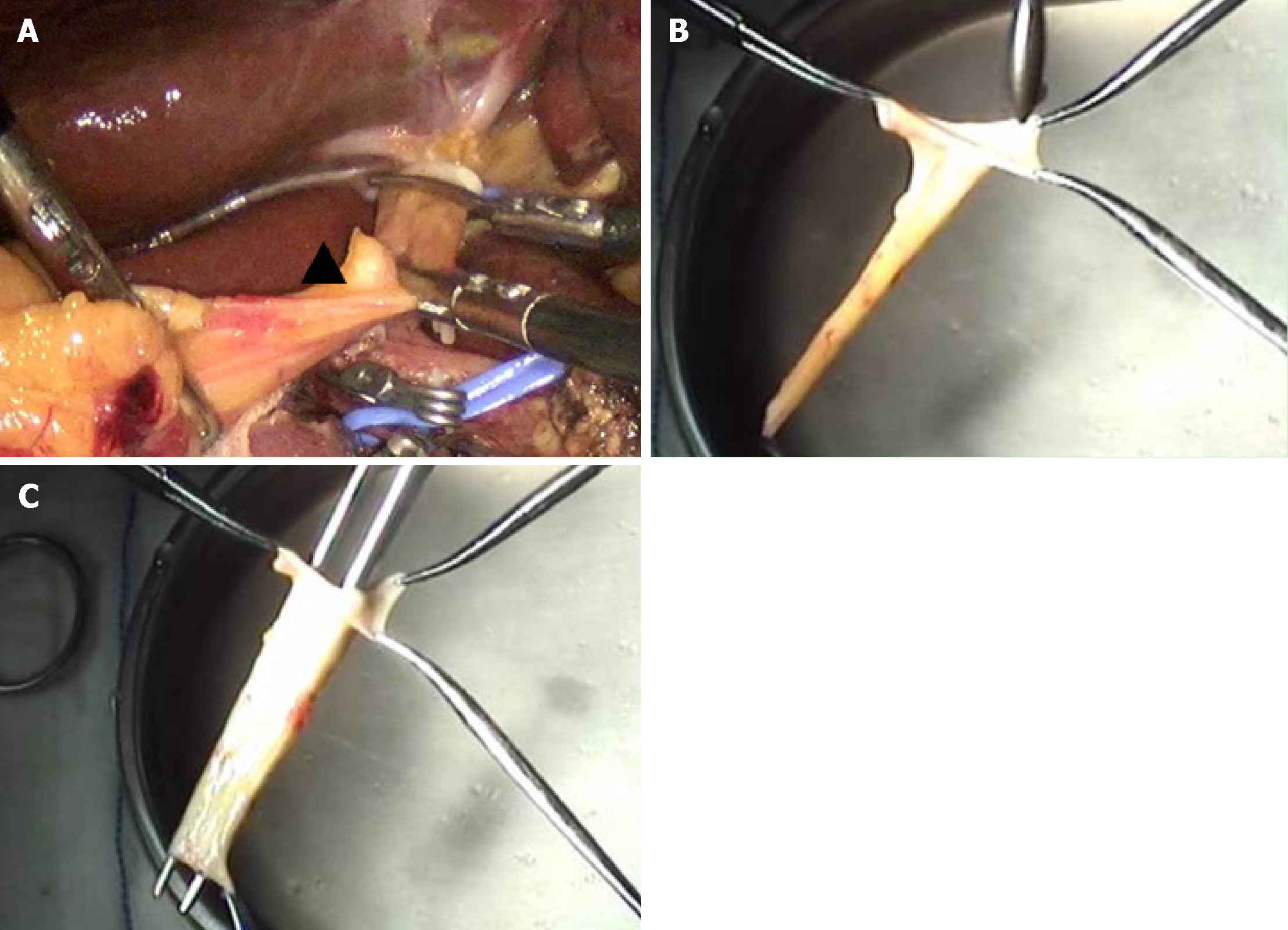
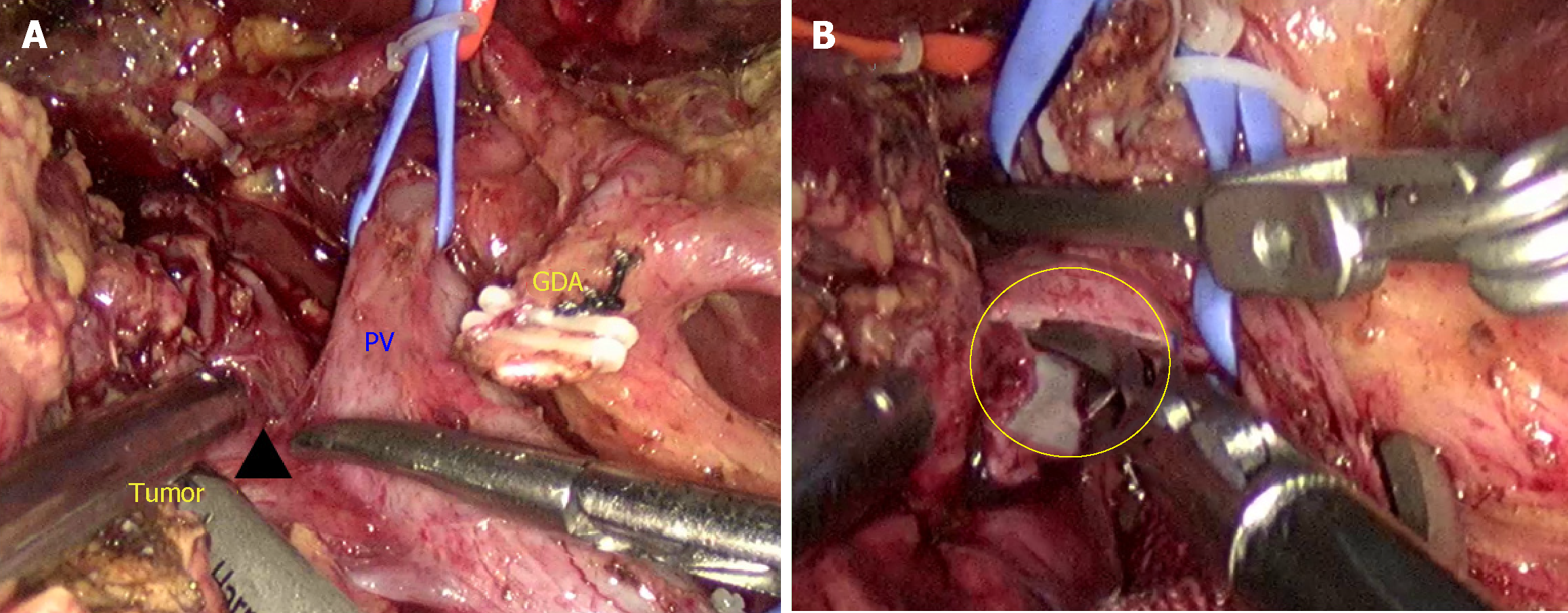
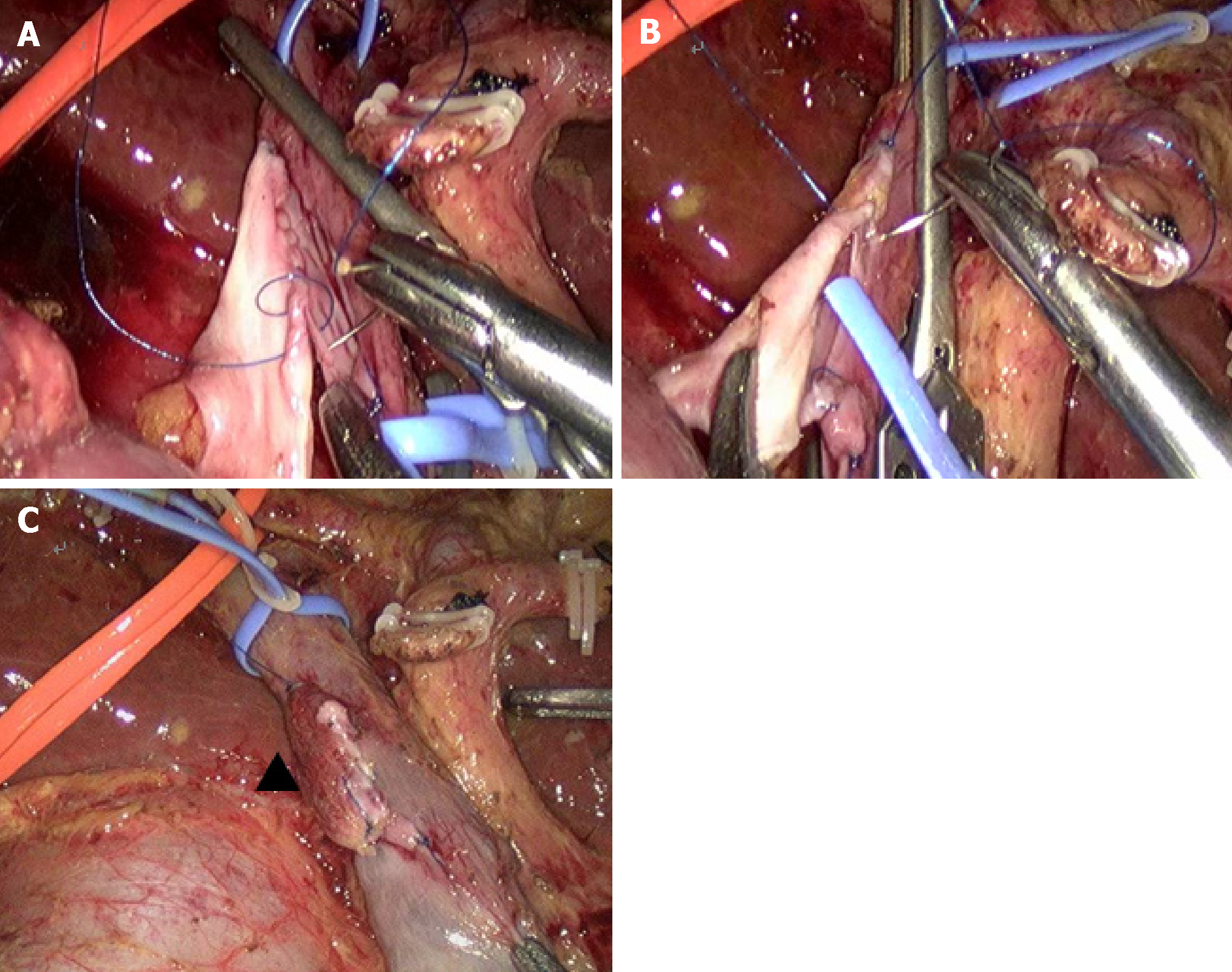
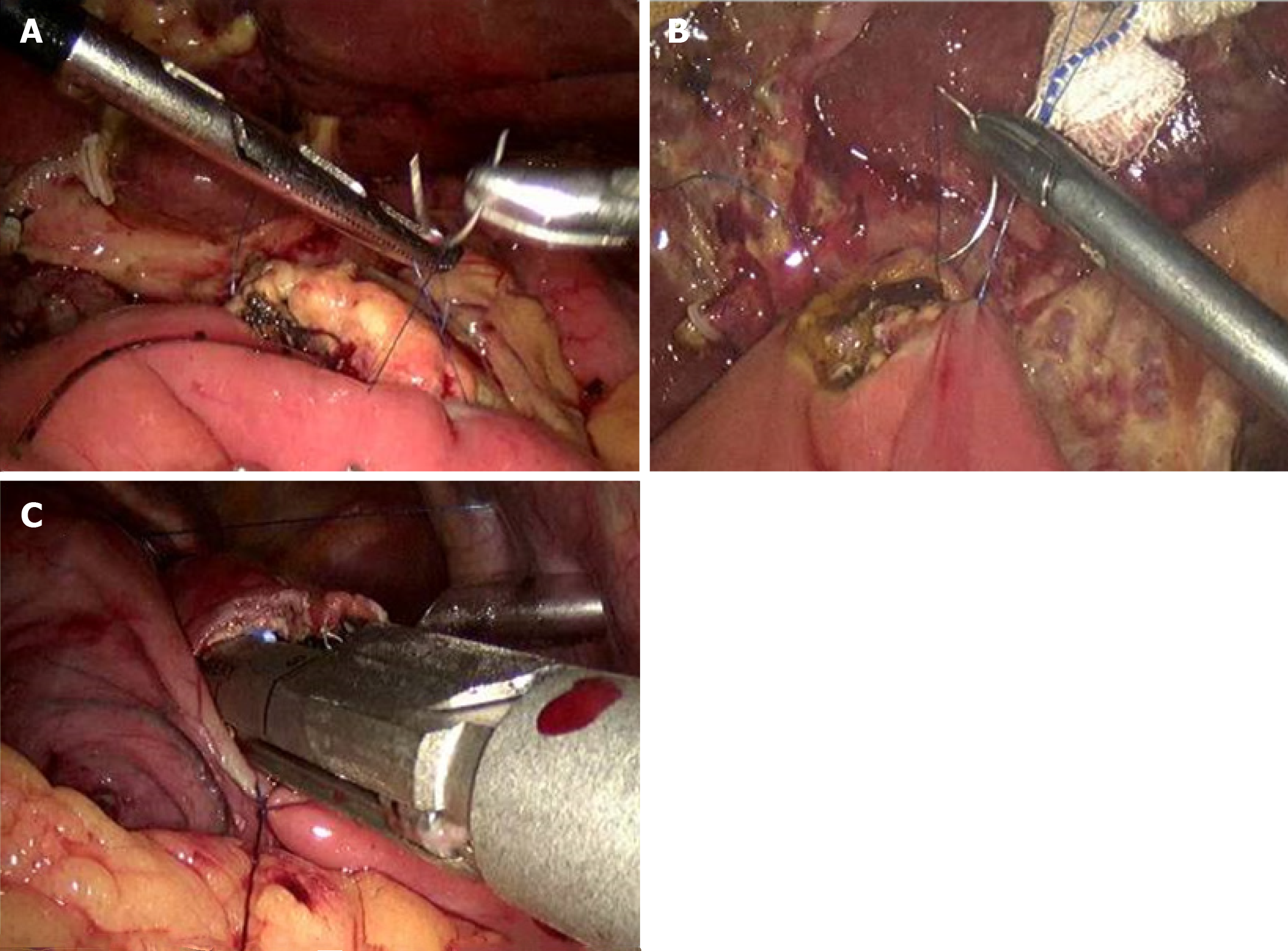
Intraoperative exploration revealed that the liver showed slight sclerosis changes and blunted margin, and fibrosis changes of the phrenic surface of the liver at the gallbladder bed appeared, with a size of approximately 4 cm × 3 cm. The gallbladder swelled to a size of approximately 12 cm × 6 cm × 6 cm. Bile duct obstruction was caused by the tumor and the bile duct above the obstructed area was dilated to approximately 2.5 cm in diameter. Thus, we attempted LPD. Thereafter, the gastrocolonic ligament was dissected. Additionally, we performed a Kocher maneuver to show the second and third portions of the duodenum and then revealed the inferior vena cava (IVC), pancreas, superior mesenteric vein (SMV), and ligament of Treitz. A postpancreatic tunnel was created. The gastroduodenal artery was identified and clipped with Hem-o-lock. The right gastric vein and artery and right gastroepiploic vein and artery were dissected. Thirty percent of the distal stomach was dissected. The jejunum was transected at 15 cm away from the ligament of Treitz. The ligament of Treitz was totally removed, and the proximal jejunum was passed through the tunnel of transverse mesentery. The pancreatic neck was transected with an ultrasonic dissector, and the main pancreatic duct was transected with scissors. The gallbladder was dissected, and the common bile duct was transected. The uncinate process of the pancreas was also dissected. It was found that the tumor was approximately 3 cm × 1.5 cm × 1.5 cm in size through the intraoperative separation exploration, invading the right wall of the portal vein. Considering the condition of the intraoperative situation, a large part of the portal vein wall was removed, and the direct suture led to portal vein stenosis. Pancreaticoduodenectomy combined with portal vein resection as well as repair and reconstruction of the hepatic ligamentum teres, was performed. Under the laparoscope, the hepatic ligamentum teres was excised, taken out through the disposable laparoscopic trocar, and then recanalized in vitro with a bougie step by step. The recanalized hepatic ligamentum teres was cut longitudinally and trimmed into vascular patches that were prepared to reconstruct the defect of the portal vein (Figure 2). Additionally, the portal vein was shut using clamps, and the right wall of the invaded portal vein was resected, approximately 2.5 cm × 1 cm in size (Figure 3). The patch of the hepatic ligamentum teres was placed at the defect of the portal vein and then was repaired and sutured. The patch was sutured to the defect of the portal vein with 5-0 prolene line to remove the clamps of blood vessels and open the portal vein. Patency of the blood flow of the portal vein was observed, no bleeding was found in the repair site, and reconstruction of the portal vein was successful (Figure 4). The digestive tract was reconstructed through the Child procedure (Figure 5). The operative time was 560 min, and intraoperative blood loss was 100 mL. The duration of the blood occlusion time was 63 min, and no blood transfusion was required.
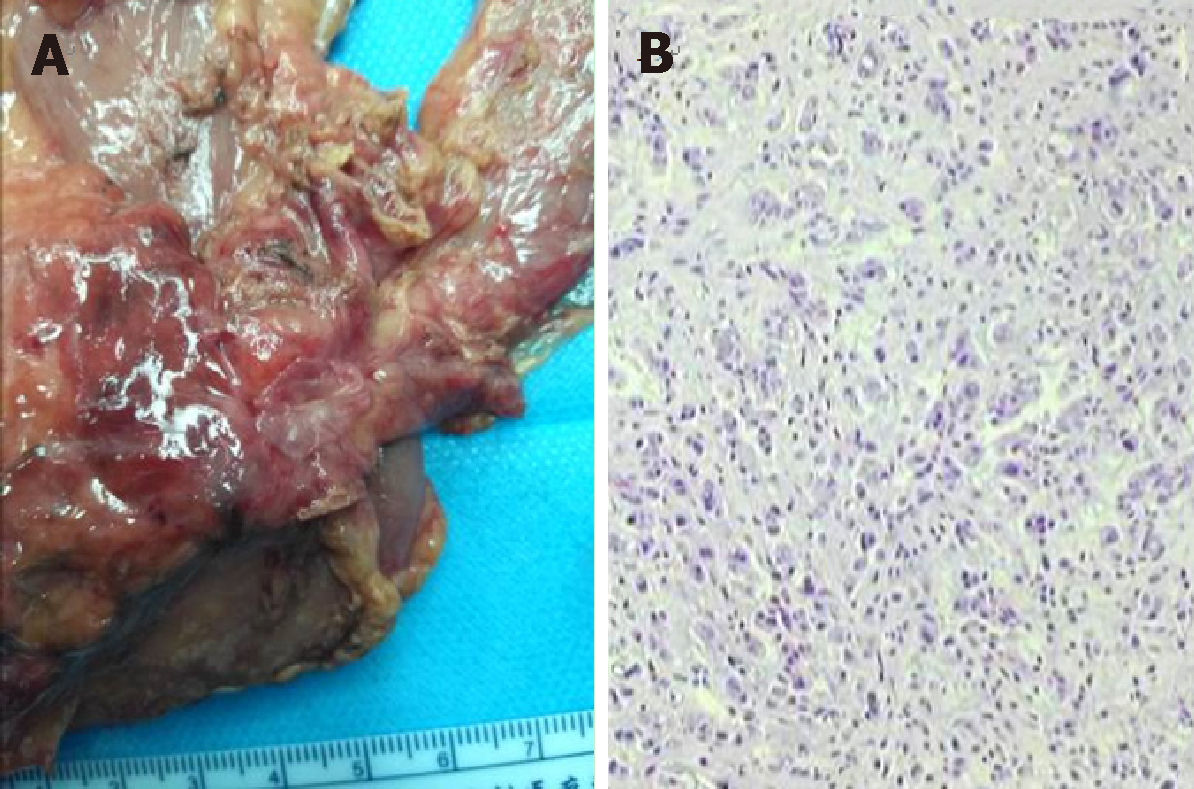
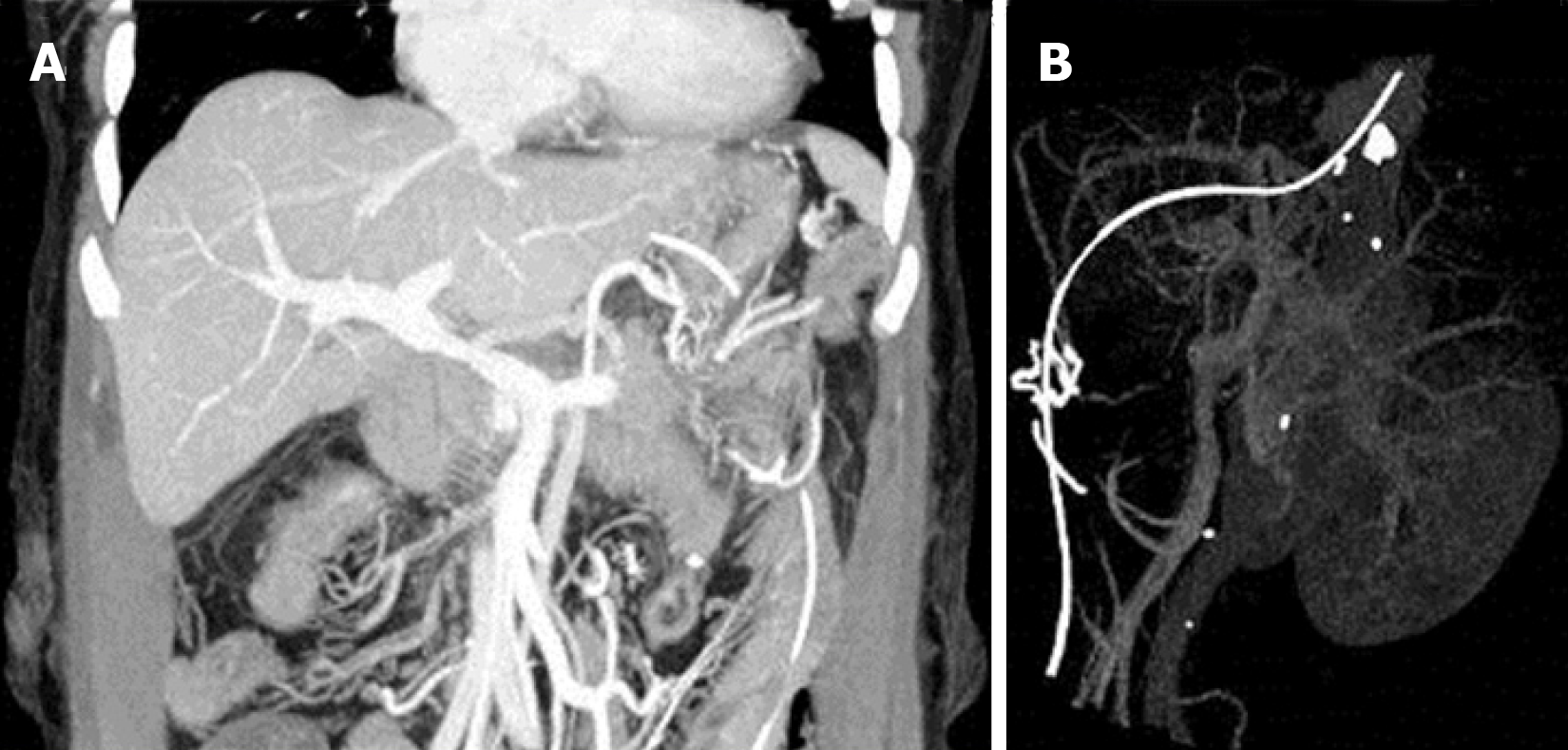
The patient continued to undergo ERAS procedures after the operation. At the same time, the application of liver protection, anticoagulant therapy, and prophylactic use of antibiotics, as well as other treatments, were also administered. The patient began bedside activities 8 h after the operation. The levels of liquid amylase and bilirubin extracted from the peritoneal drainage tube on the 3rd and 5th day after the operation, respectively, were not high. The pathological results after the operation showed poorly differentiated adenocarcinoma of the common bile duct that invaded the whole layer of the bile duct wall and lateral wall of the portal vein, with no metastasis in the lymph nodes (Figure 6). The patient was administered with oral Polyvir 75 mg qd as antithrombotic treatment from the 9th day after the operation. CT of the portal vein was conducted after the operation, indicating that the portal vein was smooth with no thrombosis (Figure 7). There were no complications such as pancreatic fistula and hemorrhage during hospitalization. The patient was cured and discharged 11 days after the operation. Follow-up for 6 months after discharge showed no stenosis of the portal vein and good patency of blood flow (Figure 8).
3D laparoscopy has the advantage of providing a better visual field, facilitating more precise operation and more definite observation of the anatomical structure, which is helpful to shorten the operation time and reduce intraoperative bleeding. This is the first LPD case in which the hepatic ligamentum teres patch was used to repair the portal vein to treat distal cholangiocarcinoma.
When the tumor invades the portal vein or superior mesenteric vein, some vessels should be removed according to the situation. In PD, cases of combined reconstruction involving the portal vein and SMV have been reported[1-3]. The main materials used for vascular reconstruction are artificial blood vessels, which have good strength and mechanical fatigue resistance, but are expensive and facilitate the formation of thrombi; problems such as histocompatibility may also occur. Additionally, materials such as the internal jugular vein, great saphenous vein, and other autologous vascular materials make the operation steps relatively more complex. We began to study the histology of the hepatic ligamentum teres as early as in 2003 at our medical center. It was found that the wall of the hepatic ligamentum teres after recanalization was divided into three layers—the intima, media, and adventitia—and the smooth surface of the lumen was covered with complete endothelial cells. Verhoeff staining showed that the tube wall of the hepatic ligamentum teres is composed of elastic fibers, collagen fibers, and smooth muscle, and its structure is similar to that of the normal veins. Thus, it has the anatomical and histological basis for vascular transplantation materials and could be used to replace and repair the abdominal veins[4]. The use of hepatic ligamentum teres as a substitute material for autogenous blood vessels has the advantages of low cost, convenient material selection, and good biocompatibility, making it have a good application prospect. Moreover, the application of the hepatic ligamentum teres has successfully repaired important abdominal vessels such as the portal vein and SMV[5]. Studies on the hepatic ligamentum teres solved the problem of vascular repair and reconstruction materials after the hepatobiliary and pancreatic combined vascular resection[6]. Previous studies and successful cases have provided a theoretical and practical basis for the laparoscopy-based recanalization of the autologous ligamentum teres hepatis followed by repair of the portal vein lateral wall in this study.
The hepatic ligamentum teres is mainly used as follows: to repair perforation of the gastroduodenal ulcer or biliary duct; to repair and reconstruct the abdominal vasculature; in the coverage and hemostasis of wounds of the liver, pancreas, and spleen; and to wrap around the gastroduodenal artery in abdominal surgery[7-10]. Depending on our experience, using the hepatic ligamentum teres patch to repair the portal vein may follow the steps as: (1) The hepatic ligamentum teres is excised and then recanalized in vitro using a bougie step by step; (2) Following recanalization, the hepatic ligamentum teres is cut longitudinally and trimmed into vascular patches that are prepared to reconstruct the defect of the portal vein; (3) The portal vein is closed using clamps, followed by resection of the invaded portal vein. The patch of hepatic ligamentum teres is placed at the defect of the portal vein and is then repaired and sutured. The patch is sutured to the defect of the portal vein with 5-0 prolene line; (4) The clamps of the blood vessels are removed, and the portal vein is opened; and (5) Patency of the blood flow of the portal vein indicates successful reconstruction of the portal vein.
The control of postoperative complications is an important factor affecting the recovery of patients after pancreaticoduodenectomy. The incidences of incision, infection, and anastomotic complications after traditional pancreaticoduodenectomy are high[11-13]. In recent years, studies from multiple centers have shown that, compared with PD, the incidences of intraoperative bleeding, postoperative incision-related complications, and hospital stay in LPD are lower, while the incidences of severe complications, such as hemorrhage and pancreatic fistula, are not significantly higher. The value of LPD in practical application has been confirmed[14-16]. For patients with tumor invasion of the portal vein/SMV, the range of LPD resection and dissection can reach the standard PD level[16-18]. The incidence of postoperative complications and mortality are not significantly increased, giving LPD a certain advantage over PD[19]. The possibilities of complications, such as portal vein stenosis and portal vein thrombosis, were found after the operation. CT venography and other examinations of the portal vein were performed after the operation in our study. No thrombus formation or vascular stenosis was found.
In this case, the concept and measures of ERAS were carried out at our hospital during the perioperative period. ERAS embodies the idea of fine management for surgical patients and has positive significance in improving the safety and shortening the hospitalization time of patients, and good clinical results were obtained. Thus, ERAS measures can also be performed in patients with LPD during the perioperative period[20].
It is safe and feasible to use the hepatic ligamentum teres patch to repair the portal vein in LPD. However, the long-term efficacy of this technique for venous reconstruction requires further investigation.
Manuscript source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Rabago LR S-Editor: Cui LJ L-Editor: Wang TQ E-Editor: Zhou BX
| 1. | Khatkov IE, Izrailov RE, Khisamov AA, Tyutyunnik PS, Fingerhut A. Superior mesenteric-portal vein resection during laparoscopic pancreatoduodenectomy. Surg Endosc. 2017;31:1488-1495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Takahashi M, Saiura A, Takahashi Y. The Usefulness of Patch Repair Using the Repermeabilized Umbilical Vein of the Round Ligament for Hepatobiliary Malignancies. World J Surg. 2017;41:2813-2816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Kauffmann EF, Napoli N, Menonna F, Vistoli F, Amorese G, Campani D, Pollina LE, Funel N, Cappelli C, Caramella D, Boggi U. Robotic pancreatoduodenectomy with vascular resection. Langenbecks Arch Surg. 2016;401:1111-1122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | Zhu WT, Chen QP, Zhang CX, Guan QH, Zhang F, Huang Q. Anatomical and histological observation of the ligmentum teres hepatis for adults. Chin J Clinicians. 2011;5:2078-2080. [DOI] [Full Text] |
| 5. | Chen QP, Ou K, Guan QH, Zhang F, Lin XT. Feasibility study on reconstruction of portal vein/superior mesenteric vein using ligmentum teres hepatis.. Shandong Med J. 2006;46:7-8. [DOI] [Full Text] |
| 6. | Zhu WT, Chen QP, Guan QH, Zhang F, Zhang CX, Huang Q, Wang HT. Comparative study of the length and diameter in recanalized adult ligamentum teres hepatic and their auto-portal vein and superior mesenteric vein. Chin Arch Gene Surg. 2012;6:386-393. [DOI] [Full Text] |
| 7. | Dokmak S, Aussilhou B, Ragot E, Tantardini C, Cauchy F, Ponsot P, Belghiti J, Sauvanet A, Soubrane O. Reconstruction of Bile Duct Injury and Defect with the Round Ligament. J Gastrointest Surg. 2017;21:1540-1543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Banerjee JK, Bharathi RS, Rao PP. Buttressing hepaticojejunostomy's with hepatic round ligament flap may be beneficial. Pol Przegl Chir. 2017;89:5-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Toshima T, Ikegami T, Matsumoto Y, Yoshiya S, Harimoto N, Yamashita Y, Yoshizumi T, Ikeda T, Shirabe K, Maehara Y. One-step venous reconstruction using the donor's round ligament in right-lobe living-donor liver transplantation. Surg Today. 2015;45:522-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Mech K, Wysocki Ł, Guzel T, Słodkowski M. Can round ligament of the liver patch decrease the rate and the grade of postoperative pancreatic fistula? Pol Przegl Chir. 2016;88:63-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 11. | Ahmad SA, Edwards MJ, Sutton JM, Grewal SS, Hanseman DJ, Maithel SK, Patel SH, Bentram DJ, Weber SM, Cho CS, Winslow ER, Scoggins CR, Martin RC, Kim HJ, Baker JJ, Merchant NB, Parikh AA, Kooby DA. Factors influencing readmission after pancreaticoduodenectomy: a multi-institutional study of 1302 patients. Ann Surg. 2012;256:529-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 201] [Cited by in RCA: 231] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 12. | Okano K, Hirao T, Unno M, Fujii T, Yoshitomi H, Suzuki S, Satoi S, Takahashi S, Kainuma O, Suzuki Y. Postoperative infectious complications after pancreatic resection. Br J Surg. 2015;102:1551-1560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 95] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 13. | Fong ZV, McMillan MT, Marchegiani G, Sahora K, Malleo G, De Pastena M, Loehrer AP, Lee GC, Ferrone CR, Chang DC, Hutter MM, Drebin JA, Bassi C, Lillemoe KD, Vollmer CM, Fernández-Del Castillo C. Discordance Between Perioperative Antibiotic Prophylaxis and Wound Infection Cultures in Patients Undergoing Pancreaticoduodenectomy. JAMA Surg. 2016;151:432-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 96] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 14. | Palanivelu C, Rajan PS, Rangarajan M, Vaithiswaran V, Senthilnathan P, Parthasarathi R, Praveen Raj P. Evolution in techniques of laparoscopic pancreaticoduodenectomy: a decade long experience from a tertiary center. J Hepatobiliary Pancreat Surg. 2009;16:731-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 15. | Kim SC, Song KB, Jung YS, Kim YH, Park DH, Lee SS, Seo DW, Lee SK, Kim MH, Park KM, Lee YJ. Short-term clinical outcomes for 100 consecutive cases of laparoscopic pylorus-preserving pancreatoduodenectomy: improvement with surgical experience. Surg Endosc. 2013;27:95-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 143] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 16. | Palanisamy S, Deuri B, Naidu SB, Vaiyapurigoundar Palanisamy N, Natesan AV, Palanivelu PR, Parthasarathy R, Palanivelu C. Major venous resection and reconstruction using a minimally invasive approach during laparoscopic pancreaticoduodenectomy: One step forward. Asian J Endosc Surg. 2015;8:468-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Croome KP, Farnell MB, Que FG, Reid-Lombardo KM, Truty MJ, Nagorney DM, Kendrick ML. Pancreaticoduodenectomy with major vascular resection: a comparison of laparoscopic versus open approaches. J Gastrointest Surg. 2015;19:189-194; discussion 194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 127] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 18. | Nakamura M, Nakashima H. Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? A meta-analysis of laparoscopic pancreatectomy. J Hepatobiliary Pancreat Sci. 2013;20:421-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 112] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 19. | Pang L, Kong J, Wang Y, Zhang Y. Laparoscopic versus open pylorus-preserving pancreatoduodenectomy. The first meta-analyse of retrospective matched cases. Acta Cir Bras. 2018;33:40-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Lassen K, Coolsen MM, Slim K, Carli F, de Aguilar-Nascimento JE, Schäfer M, Parks RW, Fearon KC, Lobo DN, Demartines N, Braga M, Ljungqvist O, Dejong CH; ERAS® Society; European Society for Clinical Nutrition and Metabolism; International Association for Surgical Metabolism and Nutrition. Guidelines for perioperative care for pancreaticoduodenectomy: Enhanced Recovery After Surgery (ERAS®) Society recommendations. Clin Nutr. 2012;31:817-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 338] [Cited by in RCA: 355] [Article Influence: 27.3] [Reference Citation Analysis (0)] |