Published online Sep 26, 2019. doi: 10.12998/wjcc.v7.i18.2823
Peer-review started: June 19, 2019
First decision: August 1, 2019
Revised: August 7, 2019
Accepted: August 20, 2019
Article in press: August 20, 2019
Published online: September 26, 2019
Processing time: 106 Days and 0.4 Hours
Diverse presentations of dens invaginatus (DI) and root canal treatment with an immature open apex often pose challenges to dentists. Adequate treatment planning for DI is the main reason for successful approach, i.e., we should consider the shape and depth of the concave folding, the condition of the original pulp, and the growth stage of the root formation.
A 9-year-old girl complained of severe pain of the right maxillary incisor (tooth 12) when chewing for two weeks. Following clinical and radiographic examinations, Oehlers type III DI of tooth 12, with an immature open apical foramen and a symptomatic periapical pathosis, was diagnosed. Cone-beam computed tomography verified the specific spatial and stereoscopic data regarding the communication between the main root canal and pseudo root canal of the involved tooth. After removing the source of infection, a mineral trioxide aggregate was selected to fill and seal the pseudo root canal; additionally, pulp capping of the main canal was performed through the interconnections between the root canals in the middle segment to preserve pulp vitality and enable continual root formation and eventual root apex closure.
We propose to conduct main root canal pulp capping for DI with communication between the main and pseudo root canals.
Core tip: The present case report is the first paper describing a case of dens invaginatus with an apical lesion and communication between the main root canal and pseudo root canal managed using nonsurgical endodontic treatment of the infected pseudo root canal, and only employing pulp capping on the main root canal to retain pulp vitality, thus enabling continual root formation with closure of the open root apex.
- Citation: Lee HN, Chen YK, Chen CH, Huang CY, Su YH, Huang YW, Chuang FH. Conservative pulp treatment for Oehlers type III dens invaginatus: A case report. World J Clin Cases 2019; 7(18): 2823-2830
- URL: https://www.wjgnet.com/2307-8960/full/v7/i18/2823.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i18.2823
Dens invaginatus (DI) is a rare dental malformation resulting from invagination of the tooth crown. In most cases, it occurs when the enamel organ invaginates into the surrounding dental papilla prior to its calcification[1]. Various terminologies have been used to describe this dental anomaly, including tooth inclusion, dens in dente, invaginated odontoma, dentoid in dente, and dilated composite odontoma[2]. The incidence of DI reportedly varies between 0.04% and 10%, and the most commonly affected tooth is the maxillary lateral incisor[3-5]. The Oehlers classification has widely been adopted to verify the extent of malformation due to tooth invagination[6]. With respect to the Oehlers classification, type I DI is the most frequent (65.9%), followed by type II (29.5%), with type III being the least common (4.6%)[7].
Previously, Kramer[8] demonstrated that invagination plays a key role in causing the structural deformity that is observed in the enamel layer, thereby resulting in the underlying dentin layer being exposed. The structure of the dentin that surrounds the invagination is irregular, with connective tissue inclusions and communication towards the pulp. Without enamel, microbes spread easily via the dentin tubules, leading to pulpal infection.
The variable appearance of DI and its root canal treatment in an immature tooth are challenges often encountered by dentists. Adequate treatment planning and prognosis evaluations of DI should take into consideration the shape and depth of the concave folding, the condition of the original pulp, and the growth stage of the root formation[9]. Here, we report the case of a patient with type III DI in the right maxillary lateral incisor (tooth 12), with vital pulp, necrotic invagination, an open apex, a large periapical lesion, and communication between the main root canal and pseudo root canal, which was managed successfully using an innovative conservative approach, resulting in a shortened therapy procedure and maintenance of pulp vitality of the main root canal. To the best of our knowledge, the present case report is the first to describe a case of DI with an apical lesion and communication between the main root canal and pseudo root canal that was managed using nonsurgical endodontic treatment of the infected pseudo root canal and employing pulp capping on the main root canal to retain pulp vitality, thus enabling continual root formation with closure of the open root apex.
A 9-year-old girl who complained of severe pain over tooth 12 during chewing for two weeks was referred to the Department of Conservative Dentistry of our Institution.
The patient had fair oral hygiene.
Neither a history of trauma nor a significant past dental and medical history was noted.
Intraoral examination revealed a peg-shaped clinical crown of tooth 12 with a talon cusp, depression, and a pit on the occlusal side (Figure 1A and 1B) without intraoral swelling or a sinus tract. Severe tenderness on palpation and percussion of tooth 12 was noted.
The involved tooth 12 responded normally to thermal (cold) and electric pulp testing (Parkell pulp vitality tester, Farmingdale, NY, United Stated), and was free of caries and restoration; grade 1 tooth mobility and < 2 mm periodontal probing depths were also observed. Moreover, teeth 11 and 13 showed normal responses to both cold and electrical pulp sensitivity testing.
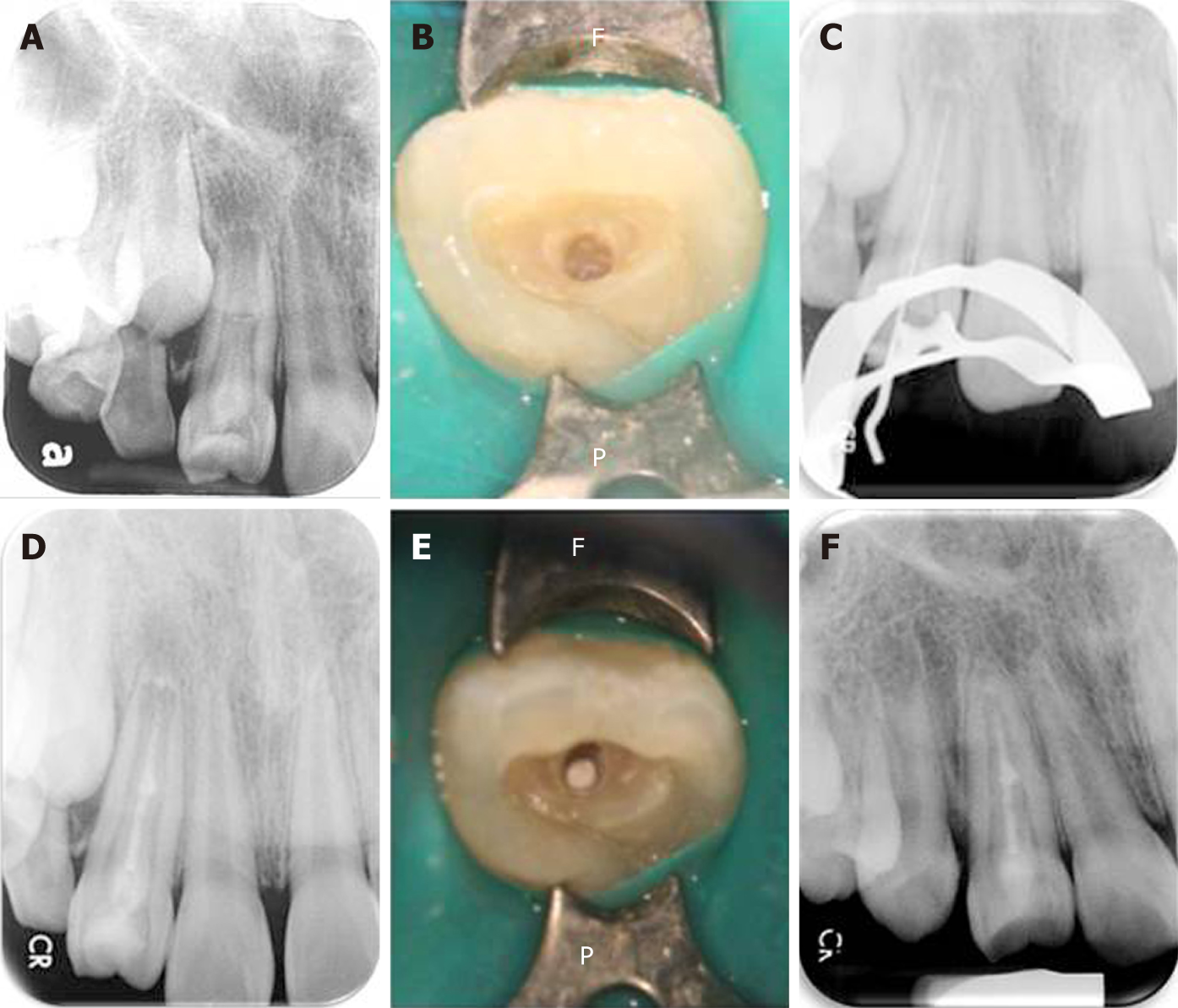
A periapical radiograph of tooth 12 revealed a large elliptical space within the invagination; the invagination of dentin lined by enamel extended into the main canal space with spreading into the apical part of the tooth root. Thus, tooth 12 seemed to be associated with a large periapical radiolucent lesion around an immature root apex (Figure 2).
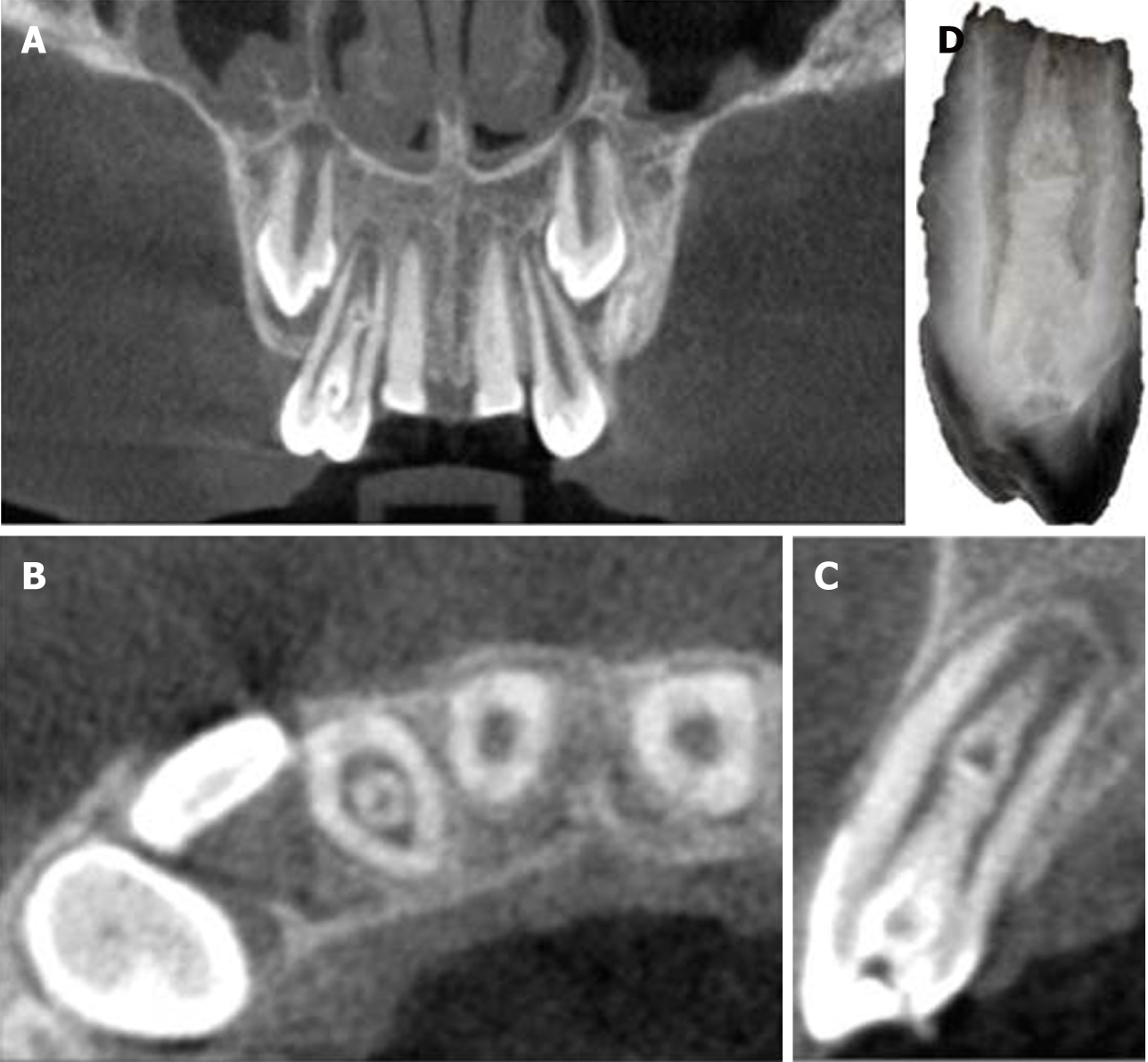
Cone-beam computed tomography (CBCT) (EPX-Impla; E-Woo Technology, Yongin, South Korea) revealed a type III invagination extending from the crown to the root apex, with an enlarged root canal space and communication with the main root canal in the middle part. A well-defined unilocular periapical radiolucent lesion measuring about 6 mm (mesio-distal) × 7 mm (labio-palatal) × 8 mm (cranio-caudal) was observed around the open apex of tooth 12 (Figure 3A, 3B, and 3C). The three-dimensional structure of the DI was reconstructed using OsiriX MD software (Figure 3D; Supplementary material).
A diagnosis of Oehlers type III DI with pulp necrosis of the pseudo root canal and symptomatic apical periodontitis was rendered.
After discussion with the patient and her parents, a treatment plan consisting of vital pulp therapy of the main root canal followed by nonsurgical endodontic treatment for the pseudo root canal of tooth 12 was suggested. Informed consent was obtained from the parents of the patient. The treatment was conducted in full accordance with the ethical principles of the World Medical Association Declaration of Helsinki.
The pseudo root canal is generally regarded as the usual site of origin of infection in DI[10]. In the present case, the central portion of the pulp was considered to be the pseudo root canal based on a periapical image of tooth 12 (Figure 4A), and the adjacent bilateral sides were the entrances to the main root canal. Therefore, the tooth chamber was opened at the central portion of the tooth to treat the pseudo root canal as an emergency measure to relieve the symptoms.
Local anesthesia with 2% lidocaine was administered around tooth 12 and the access cavity of the invagination was carefully prepared with rubber dam isolation. A surgical operating microscope (OPMI® pico, Carl Zeiss, Oberkochen, Germany) was used to explore the main root canal carefully to prevent any potential damage to the main root canal. Moreover, with respect to the information provided by CBCT imaging, the extent, position, and pulpal involvement of the invagination of the pseudo root canal of tooth 12 were accurately assessed (Figure 4B).
With the assistance of periapical radiographic imaging (Figure 4C) and an electronic apex locator, a 19-mm working length was confirmed when the patient visited the clinic for the second appointment. The pseudo root canal that appeared to be invaginated was instrumented with K-files of international standardization organization (ISO) size 40 (master apical file), which were then stepped back towards size 60. The pseudo root canal was irrigated well with 3% sodium hypochlorite solution after each instrumentation. Once the instrumentation was finished, pseudo root canal dressing was conducted with calcium hydroxide, and the entrance of the operated cavity was covered with 3-mm-thick Cavit (3M ESPE United States, Norristown, PA, United States) for half a month.
The patient was completely asymptomatic upon the third appointment. The temporary restorative materials were removed under rubber dam isolation. Irrigation with 3% sodium hypochlorite solution, ISO size 30 stainless steel hand files, and passive ultrasonic irrigation (Obtura Spartan, Algonquin, IL, United States) were used to remove the calcium hydroxide paste. The tooth was examined under a microscope to ensure that no remnants of the paste remained.
Root canal filling of the pseudo root canal was subsequently performed, as the infection had been controlled successfully. Notably, the main root canal was still vital, with an open apex, and had a complicated structure. Considering the interconnections between the root canals in the middle segment, a mineral trioxide aggregate (MTA) (Dentsply Tulsa Dental, Tulsa, OK, United States), which has good bio-compatibility, was selected to fill and seal the pseudo root canal, and was used for pulp capping in the main root canal.
After a final irrigation with normal saline, paper points were used to dry the pseudo root canal. The MTA was mixed according to the manufacturer’s instructions and condensed following the recommended steps[11] incrementally until the cemento-enamel junction was reached (Figure 4D and 4E). Moistened cotton was placed into the pulp chamber, and the access cavity was sealed with Cavit for an entire day to allow complete setting of the MTA. Tooth 12 was then restored with a composite resin (3M ESPE, St. Paul, MN, United States) at the next visit. Pulp capping of the main root canal with the MTA was completed to preserve pulp vitality.
The patient was asymptomatic when followed a week later. Tooth 12 was not tender on percussion or palpation. A periapical radiograph of tooth 12 that was acquired after 6 mo revealed resolution of the periapical radiolucency. Additionally, an increase in the root wall thickness with a reduced root canal space was noted. At one year after pulp capping, the periapical area showed a normal bone density with a closed root apex (Figure 4F). Moreover, the tooth still responded normally to electric pulp testing and Laser Doppler Flowmetry, and the patient remained asymptomatic after follow-up for a further 3 years.
In concurrence with the study by Goel et al[10], the pseudo root canal of the DI in the current case was found to be the site of origin of infection, which may be due to the fact that the invagination acts as a region of stagnation for organic substances and provides a favorable surrounding for microbe proliferation. The invagination of enamel into the dental papilla results in a tunnel lined by dentin and enamel invaginating into the pulp[12].
Teeth with DI are susceptible to early caries and subsequent pulp necrosis requiring root canal treatment. Reviewing the literature, we found that treatment options for DI include preventive sealing or filling of the invagination, root canal treatment[13,14], endodontic periapical surgery[15], intentional replantation, and extraction. In certain cases, endodontic treatment techniques may involve apexification, removal of the invagination from the root canal[16], and obturation of the invagination alone while maintaining pulp vitality[17].
The diagnosis of and root canal treatment for DI are challenging in view of the complicated root canal morphology. Due to the limitations of conventional radiographic imaging, it is difficult to clearly visualize the morphology of the root canal in DI, which in turn affects the treatment outcome. CBCT, as demonstrated in the present case, provides accurate three-dimensional images that enable assessment of the root canal morphology in DI, and helps the dentist to determine the grade of the pathology and the optimum treatment modality[18].
In a previous study[19], DI with an open apical foramen was treated using calcium hydroxide or an MTA to create a hard tissue barrier followed by placement of gutta-percha on the filling. Occasionally, dentists combine apical surgery with conventional root canal therapy, which still requires advanced techniques[20]. In a study by Yang et al[17], the pseudo root canal was filled with gutta-percha, but revascularization was employed for the necrotic main canal with an open apex to induce blood flow to the coronal portion and to reduce the surgical difficulty. Pulp regeneration therapy appeared to facilitate root development; however, based on an animal study, the apposition material-induced thickening of root walls may be of different nature dentin, cementum, or even bone[21]. Furthermore, this therapeutic modality has the potential drawbacks of involving relatively complicated procedures, as well as being time-consuming and expensive. In the present case, much of the real pulp tissue was preserved through pulp capping.
Recently, Ceyhanli et al[22] preserved the main root canal vitality without applying any treatment, and non-surgical endodontic treatment was performed only on the invaginated canal of tooth 22 with type III DI and peri-invagination pathosis in a 17-year-old female patient. CBCT did not reveal intersection of the pseudo root canal with the main root canal. In comparison with the case of Ceyhanli et al[22], the DI in the current case was more complicated, presenting with not only the infected pseudo root canal, but also an open root apex. In the current case, we adopted conservative vital pulp therapy on the vital main root canal. MTA was selected to fill and seal the pseudo root canal, and for pulp capping of the main root canal through the interconnection between the root canals in the middle segment. Once the source of the infection is eliminated, the abundant blood supply of the main root canal from the open apical foramen, as well as the induction and formation mechanisms of the vital pulp, can facilitate root development. Therefore, appropriate conservative procedures, as shown in the current case, can be considered as an alternative management modality for complicated cases of DI with an open root apex and communication between the main root canal and pseudo root canal.
Although the complicated internal structure of the root canal in DI hinders mechanical debridement, the use of CBCT for accurate diagnosis (as shown in our case, and in the case reported by Ceyhanli et al[22]), and treatment with copious chemical irrigation, ultrasound equipment, and intracanal medication can improve the outcome of debridement. Moreover, appropriate repair of the immature tooth using microscopic assistance and bio-compatible filling materials can maintain the dental pulp activity, and acceptable results can be achieved even in complicated DI cases.
We thank the staff of Kaohsiung Medical University Chung-Ho Memorial Hospital and Kaohsiung Municipal CiJin Hospital for their help and support during this case.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Taiwan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gorseta K S-Editor: Zhang L L-Editor: Wang TQ E-Editor: Liu JH
| 1. | Alani A, Bishop K. Dens invaginatus. Part 1: classification, prevalence and aetiology. Int Endod J. 2008;41:1123-1136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 2. | Hülsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30:79-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 94] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 3. | Hovland EJ, Block RM. Nonrecognition and subsequent endodontic treatment of dens invaginatus. J Endod. 1977;3:360-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 88] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Ruprecht A, Batniji S, Sastry KA, el-Neweihi E. The incidence of dental invagination. J Pedod. 1986;10:265-272. [PubMed] |
| 5. | Kirzioğlu Z, Ceyhan D. The prevalence of anterior teeth with dens invaginatus in the western Mediterranean region of Turkey. Int Endod J. 2009;42:727-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | OEHLERS FA. Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol. 1957;10:1204-18 contd. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 283] [Cited by in RCA: 273] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Capar ID, Ertas H, Arslan H, Tarim Ertas E. A retrospective comparative study of cone-beam computed tomography versus rendered panoramic images in identifying the presence, types, and characteristics of dens invaginatus in a Turkish population. J Endod. 2015;41:473-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | KRAMER IR. The pathology of pulp death in non-carious maxillary incisors with minor palatal invaginations. Proc R Soc Med. 1953;46:503-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Forghani M, Moghim Farooji E, Abuchenari J, Bidar M, Eslami N. Conservative Treatment of an Invaginated Maxillary Lateral Incisor with a C-shaped Canal Using Cone-Beam Computed Tomography. Iran Endod J. 2015;10:281-283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 10. | Goel S, Nawal RR, Talwar S. Management of Dens Invaginatus Type II Associated with Immature Apex and Large Periradicular Lesion Using Platelet-rich Fibrin and Biodentine. J Endod. 2017;43:1750-1755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Friedl CC, Williamson AE, Dawson DV, Gomez MR, Liu W. Comparison of Mechanical and Indirect Ultrasonic Placement Technique on Mineral Trioxide Aggregate Retrofill Density in Simulated Root-end Surgery. J Endod. 2016;42:650-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Greenfeld RS, Cambruzzi JV. Complexities of endodontic treatment of maxillary lateral incisors with anomalous root formation. Oral Surg Oral Med Oral Pathol. 1986;62:82-88. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Tsurumachi T. Endodontic treatment of an invaginated maxillary lateral incisor with a periradicular lesion and a healthy pulp. Int Endod J. 2004;37:717-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Rani N, Sroa RB. Nonsurgical endodontic management of dens invaginatus with open apex: A case report. J Conserv Dent. 2015;18:492-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Ozbas H, Subay RK, Ordulu M. Surgical retreatment of an invaginated maxillary central incisor following overfilled endodontic treatment: a case report. Eur J Dent. 2010;4:324-328. [PubMed] |
| 16. | Girsch WJ, McClammy TV. Microscopic removal of dens invaginatus. J Endod. 2002;28:336-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Yang J, Zhao Y, Qin M, Ge L. Pulp revascularization of immature dens invaginatus with periapical periodontitis. J Endod. 2013;39:288-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Sponchiado EC, Ismail HA, Braga MR, de Carvalho FK, Simões CA. Maxillary central incisor with two root canals: a case report. J Endod. 2006;32:1002-1004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Vidal K, Martin G, Lozano O, Salas M, Trigueros J, Aguilar G. Apical Closure in Apexification: A Review and Case Report of Apexification Treatment of an Immature Permanent Tooth with Biodentine. J Endod. 2016;42:730-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Zoya A, Ali S, Alam S, Tewari RK, Mishra SK, Kumar A, Andrabi SM. Double Dens Invaginatus with Multiple Canals in a Maxillary Central Incisor: Retreatment and Managing Complications. J Endod. 2015;41:1927-1932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 21. | Namour M, Theys S. Pulp revascularization of immature permanent teeth: a review of the literature and a proposal of a new clinical protocol. ScientificWorldJournal. 2014;2014:737503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Ceyhanli KT, Celik D, Altintas SH, Taşdemir T, S Sezgin O. Conservative treatment and follow-up of type III dens invaginatus using cone beam computed tomography. J Oral Sci. 2014;56:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |