Published online Aug 26, 2019. doi: 10.12998/wjcc.v7.i16.2367
Peer-review started: April 24, 2019
First decision: June 3, 2019
Revised: June 11, 2019
Accepted: June 26, 2019
Article in press: June 27, 2019
Published online: August 26, 2019
Processing time: 124 Days and 11.9 Hours
The association between primary hyperparathyroidism (PHPT) and acute pancreatitis is rarely reported. Here we describe the process of acute pancreatitis-mediated PHPT induced by hypercalcemia in a male patient. Hypercalcemia induced by undiagnosed PHPT may be the causative factor in recurrent acute pancreatitis.
We report a case of hypercalcemia-induced acute pancreatitis caused by a functioning parathyroid adenoma in a 57-year-old man. The patient initially experienced a series of continuous gastrointestinal symptoms including abdominal distension, abdominal pain, nausea, vomiting, electrolyte disturbance, renal dysfunction, and acute pancreatitis. Due to prolonged hypercalcemia, the patient subsequently underwent surgical resection of the parathyroid adenoma. Two weeks after surgery, his serum calcium, amylase, and lipase concentrations were normal. The patient had a good recovery after a series of other relevant therapies.
Acute pancreatitis as the first presentation is a rare clinical symptom caused by PHPT-induced hypercalcemia.
Core tip: Acute pancreatitis as the first presentation is a rare clinical symptom caused by primary hyperparathyroidism-induced hypercalcemia. Surgical
resection remains the only safe and curative treatment option available. Therefore, the possibility of hyperparathyroidism disease needs to be considered when acute pancreatitis occurs.
- Citation: Ma YB, Hu J, Duan YF. Acute pancreatitis connected with hypercalcemia crisis in hyperparathyroidism: A case report. World J Clin Cases 2019; 7(16): 2367-2373
- URL: https://www.wjgnet.com/2307-8960/full/v7/i16/2367.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i16.2367
Primary hyperparathyroidism (PHPT) is commonly characterized as an endocrine disorder with hypercalcemia attributable to overexpression of parathyroid hormone (PTH) from one or more parathyroid glands[1]. The occurrence of hypercalcemia crisis is usually associated with an elevation of PTH. Hypercalcemia in patients with PHPT can result in various comorbidities such as gastrointestinal symptoms, electrolyte disturbance, renal dysfunction, acute pancreatitis, or can be asymptomatic[2-5]. Hypercalcemia with acute pancreatitis as an initial symptom is an uncommon presentation of PHPT and its prevalence is estimated to be between 1.5% and 7%[6,7]. Upon routine laboratory testing, PHPT may be diagnosed incidentally as hypercalcemia can be asymptomatic in a large number of patients.
The regulation of serum calcium in humans mainly depends on the secretion of PTH. The normal serum levels of calcium range from 2.25 to 2.75 mmol/L. Multi-organ clinical manifestations can occur due to excessive serum calcium. However, acute pancreatitis as the first clinical presentation in PHPT is rare. Hypercalcemia caused by undiagnosed PHPT may be the only causative factor in acute pancreatitis[8]. Therefore, this disease is often misdiagnosed or overlooked completely during clinical consultation. We report a case of hypercalcemia-induced acute edematous pancreatitis as the first manifestation of a benign parathyroid adenoma in a male patient. This man was diagnosed with PHPT and subsequently underwent parathyroidectomy with complete resolution of all symptoms.
A 57-year-old man presented to the emergency room with sudden onset of severe epigastric pain with nausea and vomiting for less than one day.
The patient’s initial symptoms consisted of sudden onset of severe epigastric pain, nausea, and vomiting. His consciousness was unaffected. The pain did not radiate along his back and was without paroxysmal exacerbation. He denied chill, fever, cough, and expectoration.
He had no history of essential hypertension, diabetes mellitus, or relevant cerebrovascular disease. There was no previous history of gastrointestinal disease or biliary system symptoms. He had no history of smoking or alcohol consumption.
His temperature, blood pressure, heart rate, and respiratory rate were all normal on admission. There was mild upper abdominal tenderness, rebound tenderness, and no apparent muscle tension in physical examination.
After admission, the patient completed a series of laboratory examinations. Blood tests revealed the following inflammation markers: White blood cell count, 26.71 × 109/L (4-10 × 109/L)(94.9% neutrophils); C-reactive protein, 35.5 mg/L (0-10 mg/L); hemoglobin, 152.0 g/L; platelet count, 433 × 109/L; glutamic-pyruvic transaminase, 15 µ/L; glutamic-oxalacetic transaminase, 13 µ/L; alkaline phosphatase, 121 µ/L; urea, 8.48 mmol/L; and creatinine, 127.0 µmol/L. The representative diagnostic markers of pancreatitis were as follows: serum amylase 1091 µ/L; serum sodium, 152.2 mmol/L; serum potassium, 4.01 mmol/L; serum calcium, 4.67 mmol/L; and serum PTH level, 95.8 pmol/L.
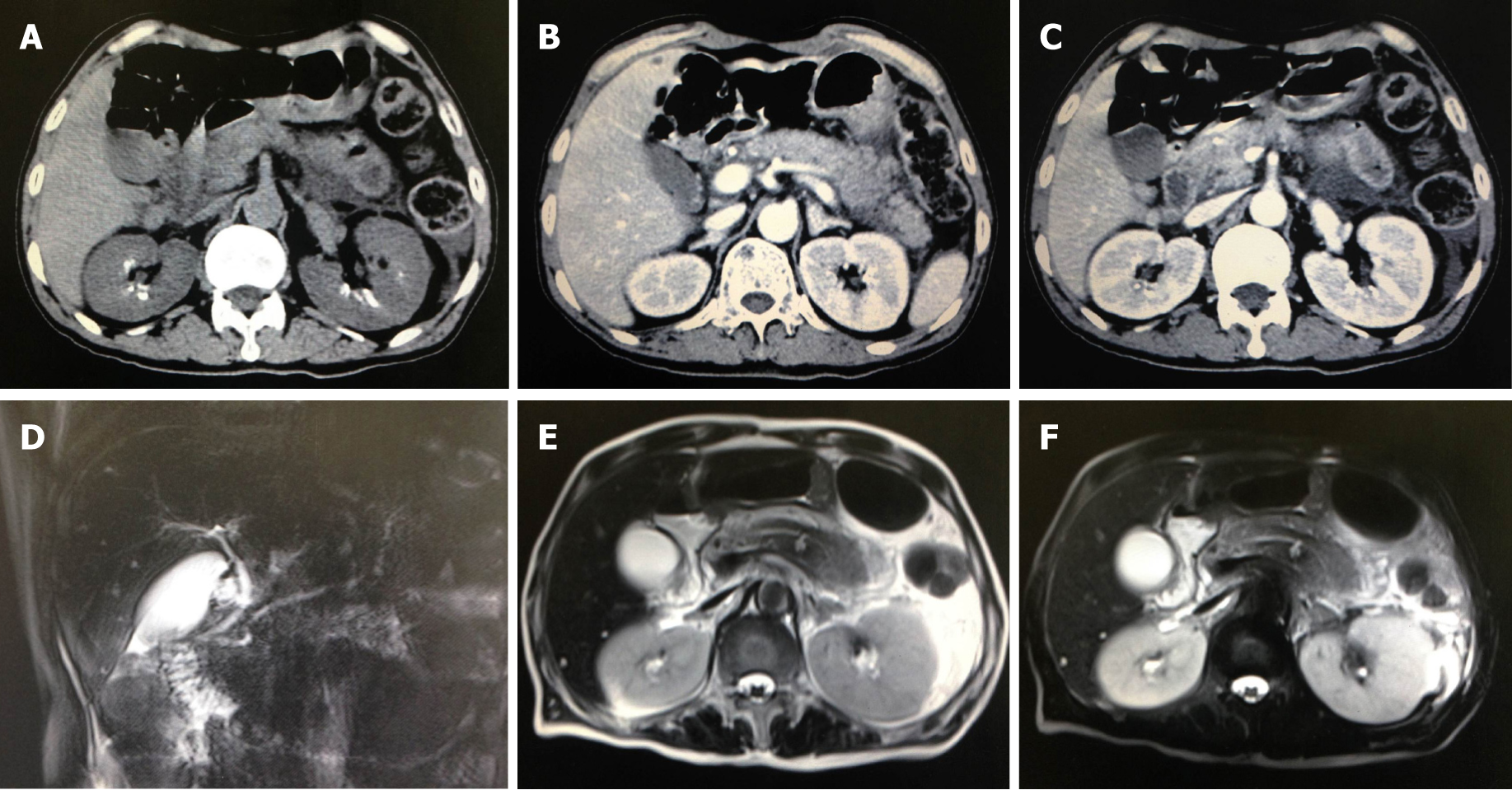
B-mode ultrasound showed mild fatty liver and no obvious gallbladder or pancreas abnormalities. Electronic gastroscopy revealed esophagitis, chronic superficial gastritis with bile reflux and duodenal bulb inflammation. Electrocardiography and contrast echocardiography showed no special heart symptoms. Computed tomography and magnetic resonance imaging of the abdomen revealed pancreatic tail contusion, exudative changes around the pancreas, and double kidney stones. Gallstones or correlative biliary system diseases were not observed (Figure 1).
In order to confirm the diagnosis, thyroid ultrasound was undertaken in this patient. It showed bilateral thyroid nodules on the right neck mass originating from the inferior thyroid gland or parathyroid (Figure 2).
On the basis of biochemical parameters combined with his clinical manifestations, the patient was diagnosed with acute pancreatitis, hypercalcemia, and PHPT.
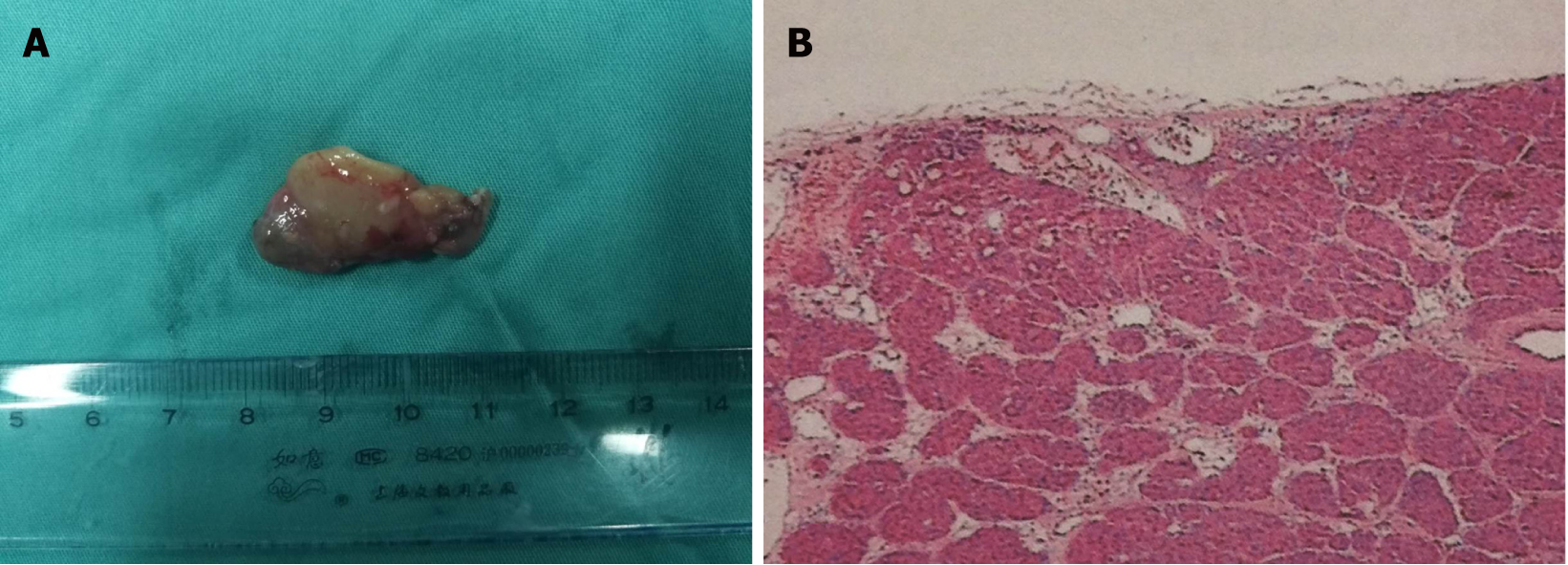
During the first two days, the patient was treated with hydration consisting of 2 L isotonic saline every day, diuresis with the intravenous loop diuretic furosemide at 20 mg every 8 h, and small doses of glucocorticoids each day for depression of serum calcium concentration. However, the concentration of serum calcium was still maintained at a high level. Due to the high risk of cardiovascular and cerebrovascular disorders and deterioration of acute pancreatitis, following discussion with the patient and his relatives, he subsequently accepted parathyroid exploration and right parathyroidectomy. During surgery, the volume of the bilateral thyroid was normal. A 3.0 cm × 2.0 cm hyperplastic parathyroid mass on the inferior aspect of the right thyroid lobe was excised. After operation, the patient was admitted to the intensive care unit and treated with fasting, water deprivation, continuous gastrointestinal decompression, gastric acid suppression, inhibition of pancreatic secretion, fluid replacement, nutritional support, and anti-infectious agents.
In the postoperative period, the levels of serum PTH and calcium decreased slowly (Figure 3), and the patient gradually recovered over the next two weeks. Histopathological examination confirmed the diagnosis of right parathyroid adenoma (Figure 4). The patient was discharged with regular follow-up for six months.
PHPT is now a common endocrine disorder caused by the inappropriate over-production of PTH secreted by an overactive parathyroid gland[9]. Compared with young individuals, postmenopausal women over the age of 50 years have a greater probability of developing PHPT[10]. The most common pathogenesis of PHPT is parathyroid gland adenomas (80%-85%), and rare causes include parathyroid hyperplasia, carcinoma, multiple endocrine neoplasia type 1 and 2A, and parathyroid cysts[11]. Most patients with PHPT have mild symptoms or are asymptomatic. Despite the variety of PHPT clinical manifestations, hypercalcemia is the most common condition in most clinical cases[12].
Hypercalcemia is a common and potentially fatal metabolic disorder that is most often attributable to PHPT or malignancy-associated disease[13]. An elevation in PTH is one of the principal factors in the initiation of hypercalcemia. Excessive accumulation of serum calcium and decompensation of the renal system promote the development of hypercalcemia. Initially, the symptoms of hypercalcemia are mild or are not notable at the time of discovery. However, the developing symptoms that characterize a crisis are mental disturbance, metabolic encephalopathy, renal insufficiency, gastrointestinal symptoms, and cardiac dysrhythmia[14]. Early diagnosis and preoperative medical management are crucial, and surgical intervention is the optimal treatment for a hypercalcemic crisis.
Acute pancreatitis is an inflammatory process, which has sudden onset due to the premature activation of proteolytic zymogens within the exocrine pancreas[15]. It can be severe with extensive morbidity and mortality[16]. The majority of cases of acute pancreatitis are caused by chronic alcohol consumption and biliary stones. The most frequent cause of acute pancreatitis is gallstone pancreatitis. Biliary stones induced pancreatitis is caused by duct obstruction by gallstone migration leading to temporary impaction of migrating stones at the duodenal ampulla, increased duct pressure, and unregulated stimulation of the digestive enzymes secreted by the pancreas. The second most common cause of acute pancreatitis is alcoholic pancreatitis. Alcohol may sensitize the pancreas to damage by external and environmental factors. The development and recurrence of acute pancreatitis are positively associated with chronic alcohol consumption.
Acute pancreatitis is an uncommon clinical manifestation of PHPT and the prevalence of PHPT-associated pancreatitis in patients were just 1%-8%[17]. The association between PHPT and acute pancreatitis has been debated for decades. Hypercalcemia may play a crucial role in this association and directly affect the severity and prognosis of the disease. Three mechanisms are involved in the development of PHPT-induced acute pancreatitis. One is PHPT-induced high serum calcium level, which can lead to acceleration of the conversion of trypsinogen to trypsin in the pancreas resulting in pancreatic autodigestion and subsequent acute pancreatitis[18]. Secondly, the accumulation of calcium can promote the formation of ductal obstruction, pancreatic calculi, and subsequent attacks of acute pancreatitis[19]. Thirdly, genetic variants in serine protease inhibitor Kazal type 1 and cystic fibrosis transmembrane conductance regulator genes in combination with hypercalcemia markedly increase the risk of developing acute pancreatitis in patients with PHPT[20].
The level of serum calcium is the key to early diagnosis, estimating disease severity, and treatment. When patients with acute pancreatitis are found to have no obvious causes and elevated serum calcium is observed, PHPT-induced pancreatitis should be suspected. The treatment of hypercalcemia includes hydration with saline, forced diuresis, bisphosphonates, calcitonin, oral phosphates, glucocorticoids, and dialysis. But surgical resection is still the most effective treatment. Parathyroidectomy may not only relieve the abdominal symptoms of acute pancreatitis but also prevent the recurrence of hypercalcemia. However, a severe parathyroid crisis caused by a parathyroid adenoma can lead to a series of secondary clinical manifestations, including gastrointestinal symptoms, electrolyte disturbance, renal dysfunction, and acute pancreatitis.
In our case, renal function reflected by creatinine and urea nitrogen increased, to some extent, before and after surgery. Therefore, we used continuous renal replacement therapy to maintain stable renal function. Continuous renal replacement therapy is a method of renal support that has the potential to avoid the development of electrolyte disturbance and deterioration of renal function. Renal replacement therapy was essential for controlling symptomatic hypercalcemia until medical therapy restored renal function and enhanced renal excretion of calcium. Therefore, PHPT-associated acute pancreatitis should be detected early and appropriate early treatment initiated. Establishing good cooperation between various hospital departments is also critical in treating this rare phenomenon of acute pancreatitis caused by PHPT-induced hypercalcemia.
The clinical features of PHPT-induced acute pancreatitis are nonspecific; thus, the diagnosis can be challenging. However, we should exclude patients with acute pancreatitis caused by chronic alcohol consumption and biliary stones before the diagnosis of PHPT-induced acute pancreatitis. Although the disease has a relatively good prognosis, complete surgical resection remains the optimal, safe and curative treatment option available. Early recognition and early-targeted treatment may be the best way to tackle the corresponding diseases.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Casella C, Manenti A S-Editor: Cui LJ L-Editor: Filipodia E-Editor: Liu JH
| 1. | Bilezikian JP, Brandi ML, Rubin M, Silverberg SJ. Primary hyperparathyroidism: new concepts in clinical, densitometric and biochemical features. J Intern Med. 2005;257:6-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Mohebati A, Shaha AR. Imaging techniques in parathyroid surgery for primary hyperparathyroidism. Am J Otolaryngol. 2012;33:457-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 3. | Silverberg SJ, Walker MD, Bilezikian JP. Asymptomatic primary hyperparathyroidism. J Clin Densitom. 2013;16:14-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Rejnmark L, Vestergaard P, Mosekilde L. Nephrolithiasis and renal calcifications in primary hyperparathyroidism. J Clin Endocrinol Metab. 2011;96:2377-2385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 5. | Starup-Linde J, Waldhauer E, Rolighed L, Mosekilde L, Vestergaard P. Renal stones and calcifications in patients with primary hyperparathyroidism: associations with biochemical variables. Eur J Endocrinol. 2012;166:1093-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Egea Valenzuela J, Belchí Segura E, Sánchez Torres A, Carballo Alvarez F. Acute pancreatitis associated with hypercalcemia. A report of two cases. Rev Esp Enferm Dig. 2009;101:65-69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Kanno K, Hikichi T, Saito K, Watanabe K, Takagi T, Shibukawa G, Wakatsuki T, Imamura H, Takahashi Y, Sato A, Sato M, Irisawa A, Obara K, Ohira H. A case of esophageal small cell carcinoma associated with hypercalcemia causing severe acute pancreatitis. Fukushima J Med Sci. 2007;53:51-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Lanitis S, Sivakumar S, Zaman N, Westerland O, Al Mufti R, Hadjiminas DJ. Recurrent acute pancreatitis as the first and sole presentation of undiagnosed primary hyperparathyroidism. Ann R Coll Surg Engl. 2010;92:W29-W31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Sociedade Brasileira de Endocrinologia e Metabologia. Bandeira F, Griz L, Chaves N, Carvalho NC, Borges LM, Lazaretti-Castro M, Borba V, Castro LC, Borges JL, Bilezikian J. Diagnosis and management of primary hyperparathyroidism--a scientific statement from the Department of Bone Metabolism, the Brazilian Society for Endocrinology and Metabolism. Arq Bras Endocrinol Metabol. 2013;57:406-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | DeLellis RA. Parathyroid tumors and related disorders. Mod Pathol. 2011;24 Suppl 2:S78-S93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Bai HX, Giefer M, Patel M, Orabi AI, Husain SZ. The association of primary hyperparathyroidism with pancreatitis. J Clin Gastroenterol. 2012;46:656-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Machenahalli P, Shotliff K. Problem based review: The patient with hypercalcaemia. Acute Med. 2015;14:138-141. [PubMed] |
| 13. | Ziegler R. Hypercalcemic crisis. J Am Soc Nephrol. 2001;12 Suppl 17:S3-S9. [PubMed] |
| 14. | Edelson GW, Kleerekoper M. Hypercalcemic crisis. Med Clin North Am. 1995;79:79-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 67] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Tsang SW, Guan YF, Wang J, Bian ZX, Zhang HJ. Inhibition of pancreatic oxidative damage by stilbene derivative dihydro-resveratrol: implication for treatment of acute pancreatitis. Sci Rep. 2016;6:22859. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Neoptolemos JP, Raraty M, Finch M, Sutton R. Acute pancreatitis: the substantial human and financial costs. Gut. 1998;42:886-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 193] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Foroulis CN, Rousogiannis S, Lioupis C, Koutarelos D, Kassi G, Lioupis A. Ectopic paraesophageal mediastinal parathyroid adenoma, a rare cause of acute pancreatitis. World J Surg Oncol. 2004;2:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Haverback BJ, Dyce B, Bundy H, Edmondson HA. Trypsin, trypsinogen and trypsin inhibitor in human pancreatic juice. Am J Med. 1960;29:421-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 134] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 19. | Cope O, Culver PJ, MIxter CG, Nardi GL. Pancreatitis, a diagnostic clue to hyperparathyroidism. Ann Surg. 1957;145:857-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 140] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Felderbauer P, Karakas E, Fendrich V, Bulut K, Horn T, Lebert R, Holland-Letz T, Schmitz F, Bartsch D, Schmidt WE. Pancreatitis risk in primary hyperparathyroidism: relation to mutations in the SPINK1 trypsin inhibitor (N34S) and the cystic fibrosis gene. Am J Gastroenterol. 2008;103:368-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |