Published online Aug 6, 2019. doi: 10.12998/wjcc.v7.i15.2094
Peer-review started: April 18, 2019
First decision: June 12, 2019
Revised: June 18, 2019
Accepted: June 26, 2019
Article in press: June 26, 2019
Published online: August 6, 2019
Processing time: 111 Days and 22.7 Hours
Duplication of the appendix is an infrequent congenital malformation with a complex classification. The horseshoe appendix is a subtype of the duplex appendix and is rarely reported in the literature. Endometriosis is a common gynecological disease that rarely occurs in the appendix. Moreover, horseshoe appendix combined with endometriosis has not been previously reported.
Here, we describe a 44-year-old woman who was admitted with a 1-d history of migratory lower right quadrant pain. Physical examination was consistent with the signs of acute appendicitis. The patient underwent an emergency exploratory laparotomy. The distal tip of the appendix was in contact with the cecum by another base, or “horseshoe appendix”. In addition, a small intestinal mass and an ovarian mass were identified. Subsequently, appendectomy, partial resection of the small intestine, and right oophorectomy were successively performed. The histopathology confirmed the diagnosis of acute inflammation of the duplex appendix with endometriosis, small intestine endometriosis, and ovarian endometriosis.
Surgeons need to be aware of the possibility of the duplex appendix when performing an appendectomy, and this study emphasizes the importance of exploring the entire abdomen.
Core tip: We describe a patient with endometriosis of the duplex appendix, small intestine, and ovary. There are no similar cases reported. Currently, the diagnosis of duplex appendix and endometriosis is difficult before surgery. Our case suggests that serum carbohydrate antigen 125 levels and fecalith of the appendix may be useful signs for the diagnosis of endometriosis and duplex appendix, respectively. However, the most important procedure is the careful exploration of the abdominal cavity during surgery. Serious legal disputes can occur due to neglecting another infected appendix or not carefully exploring other parts of the abdominal cavity.
- Citation: Zhu MY, Fei FM, Chen J, Zhou ZC, Wu B, Shen YY. Endometriosis of the duplex appendix: A case report and review of the literature. World J Clin Cases 2019; 7(15): 2094-2102
- URL: https://www.wjgnet.com/2307-8960/full/v7/i15/2094.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i15.2094
Acute appendicitis is the most common surgical emergency of the abdomen. The overall lifetime risk for acute appendicitis is 6.7% in females and 8.6% in males[1]. Duplication of the appendix is extremely rare and is usually incidentally found during surgery. A duplication of the appendix was first reported in the form of a case report in 1892[2]. To date, only a total of approximately 100 cases have been reported[3]. Endometriosis, as a common disease in women of childbearing age, predominantly occurs in the adnexa and less frequently in the digestive tract, especially in the small intestine and appendix. Here, we report a unique case of duplex appendix with acute appendicitis coexisting with appendiceal endometriosis in an adult female patient. In addition, endometriosis was found in the small intestine and ovary. The most special of the duplex appendix is the horseshoe appendix. To the best of our knowledge, only the abovementioned 14 cases have been reported thus far[4], but there are no reports of horseshoe appendix combined with endometriosis. The classification, symptoms, and radiological appearance of the duplex appendix with endometriosis have been described in the literature and are discussed in this paper.
A 44-year-old Chinese woman was admitted to the Emergency Department of The Second Affiliated Hospital of Jiaxing University (Jiaxing, China) because of migratory lower right quadrant pain for 1 d associated with nausea, vomiting, and anorexia.
She reported a 1-d medical history of migratory lower right quadrant pain that started as epigastric pain and became localized to the lower right abdominal quadrant, especially at McBurney’s point. She also complained about nausea, vomiting, and anorexia.
The patient had an 8-year history of repeated lower abdominal pain that appeared in the first 1-2 d of menstruation and disappeared after the end of menstruation. However, her menstrual cycle was regular, with no menorrhagia or dyspareunia reported. Therefore, she was not regularly seen in the gynecology clinic for several years.
The last menstrual period ended 5 d before admission. She had a history of caesarean section 18 years ago. No additional family history was presented.
Her abdominal examination revealed that the abdomen was diffusely soft, nondistended, but presented tenderness, rebound tenderness, and guarding with a voluntary component in the lower right quadrant, and increased pain with coughing at the McBurney’s point, which were consistent with the signs of acute appendicitis. Moreover, Rovsing’s sign was positive. No abdominal mass was palpable, and bowel sounds were normoactive.
Hematological examinations, including serum electrolyte levels, human chorionic gonadotropin, and complete blood count were within normal limits, apart from white blood cell count, carbohydrate antigen 125 (CA125), and C-reactive protein concen-trations that were mildly elevated at 10.1 × 109/L (77.8% neutrophils), 69.5 U/mL, and 10 mg/L, respectively.
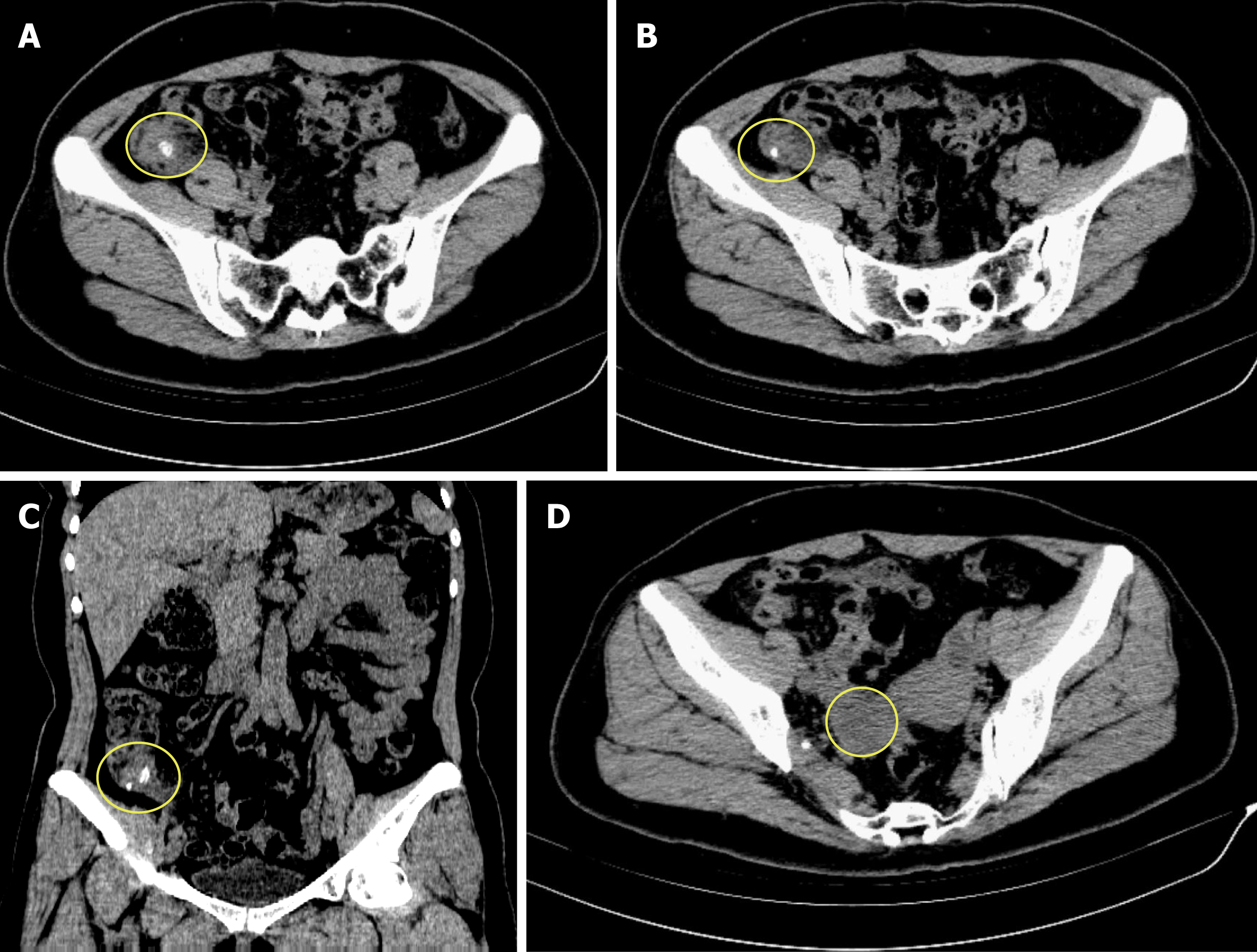
A computed tomography (CT) scan of the abdomen showed that the appendix was markedly swollen and thickened and had obvious periappendicular leaking; additionally, two fecaliths were located at the root of the appendix (Figure 1). Simultaneously, the CT scan also showed a cystic mass in the right ovary (Figure 1). The findings from the patient’s abdominal examination and CT scan were consistent with acute fecal appendicitis.
Based on the above physical examination features and imaging data, a provisional diagnosis of acute appendicitis and right ovarian cyst was made.
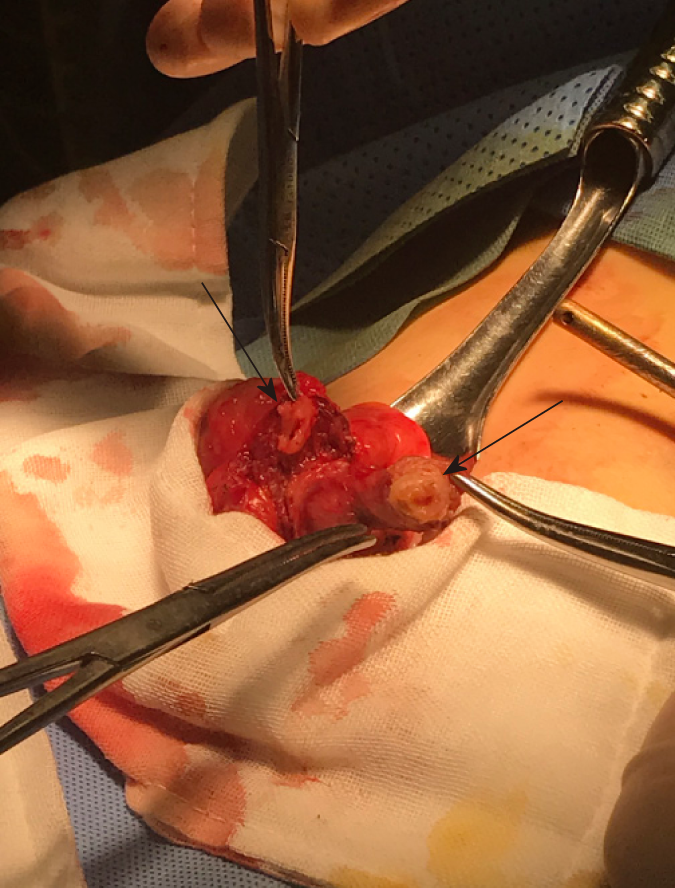
Laparoscopic examination revealed moderate bloody fluid collections, and the omentum was localized to the right lower abdomen and pelvic cavity. Additionally, a cystic mass with a size of 3.5 cm × 2.5 cm was seen in the right ovary, which was not ruptured and was consistent with the CT scan findings. No evidence of endometrium was found by laparoscopic evaluation of the abdominal and pelvic cavities. Moreover, the appendix appeared unusually atrophic upon itself and measured 3 cm × 2.5 cm at the widest diameter, which was obviously inflamed, hyperemic, and swollen, which agreed with the preoperative diagnosis. However, we found a tight adhesion between the appendix, the lateral abdominal wall, and the posterior peritoneum, resulting in unclear anatomical structures that were difficult to separate. Therefore, a laparotomy was performed via an extended McBurney’s incision in the lower right abdominal quadrant. After carefully separating the adhesions, an appendix was seen. Then, we attempted to separate the base of the appendix, and we were surprised to find that there were two bases that had their cavities both in contact with the cecum with each other through the appendiceal lumen, or “horseshoe appendix” (Figure 2). The two bases were positioned frontally on the cecum with a central mesoappendix, and the central mesoappendix vessel was fan-shaped. The proximal appendix stump and mesoappendix vessel were divided and ligated, and then the appendix was removed for pathological examination. Unfortunately, because there was no consideration of the rarity of this case, there were not enough intraoperative photographs remaining. Upon gross pathological inspection, the total length of the duplex appendix was approximately 6 cm. There were two cavities in the root of the cecum, both of which led to a swollen inflamed appendix containing a fecalith. Subsequently, a meticulous inspection of distal ileal segments and right tuboovarian structures was performed through palpation, and we unexpectedly found a hard mass, 10 cm proximal to the ileocecal valve, which gave rise to a mild stenosis of the intestine. Additionally, a right ovarian cyst was found, as previously mentioned. Hence, partial resection of the small intestine with end-to-end anastomosis was executed, as well as right oophorectomy by a gynecologist. Grossly, the soft tissue mass had a size of 1.5 cm × 1.5 cm, but the serosal surface and the mucosa were normal. The cut surface revealed hard nodular regions, which contained some small cystic spaces brimmed with both serous fluid and hemorrhage. The ovarian cyst showed that the cut surface also contained several small cystic spaces and was filled with chocolate-like cyst fluid and old bleeding.
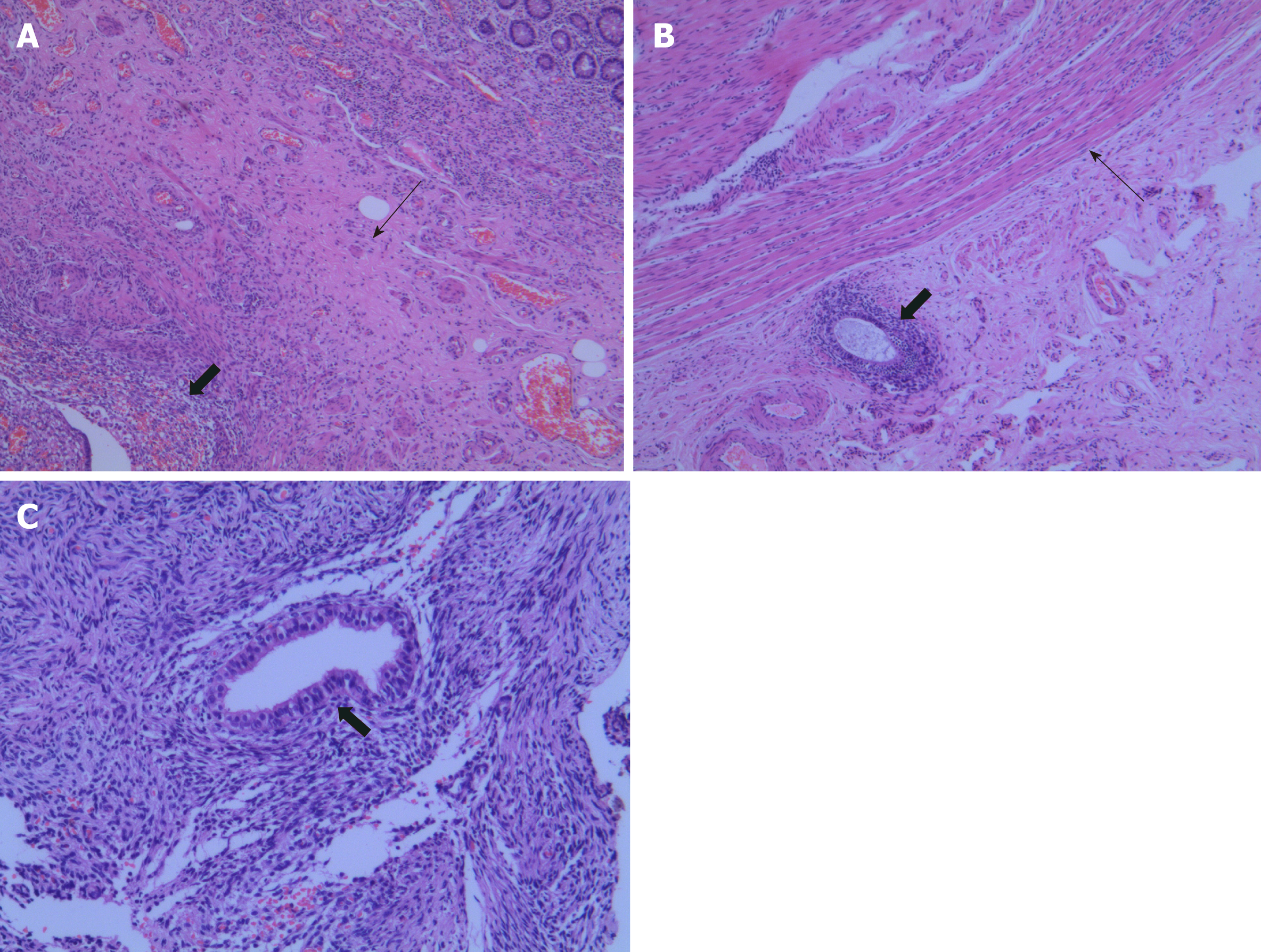
Hematoxylin and eosin staining revealed obvious acute and chronic inflammatory cell infiltration within and around the duplex appendix. The lumens of the two appendixes were obstructed with fecalith. Meanwhile, several ectopic endometrial-type glands and stroma were found in the thickened muscularis propria of the duplex appendix (Figure 3), small intestine (Figure 3), and right ovary (Figure 3). Additionally, the glands were dilated, most of which contained hemorrhage within their cavities. Histological diagnoses of duplex appendix with fecalith and endometriosis were made, which caused acute appendicitis, and diagnoses of endometriosis of the small intestine and the right ovary were also made. These results were surprising discoveries. The patient subsequently recovered well with no complications and was discharged from the hospital on the 10th postoperative day. She was referred to a gynecological clinic for further assessment of her endometriosis. At the 6-month follow-up, there were no recurrences of abdominal pain or other clinical symptoms.
Duplication of the digestive tract is a rare congenital malformation in adults because more than 80% of cases have serious abdominal or intestinal obstruction before the age of 2 years[5]. Appendiceal duplication is extremely rare and may be related to the duplication of other organs or other anomalies. Colons investigated 50000 pathological specimens of the appendix, and there were only just two cases of duplication[6]. The overall incidence of appendiceal duplication is approximately 0.004%[6]. Appendiceal duplication was first formally classified by Cave in 1936 and divided into three types based on their anatomic locations. Then, this classification was updated and amended in 1962 by Wallbridge[7] and is called the “Cave-Wallbridge” classification. Subsequently, this classification was further improved by Biermann et al[8] and Kjossev et al[9], respectively. However, there were several cases that could not be classified according to the above classifications, for instance, horseshoe appendix and triplex appendix. We believe that an updated classification system is needed to distinguish appendiceal anomalies or to modify the present system. Therefore, Calotă et al[10] proposed a new classification system for appendiceal anomalies in 2010, which was divided into number anomalies and shape anomalies and was modified by Takabatake et al[11] again in 2016. The new classification system of appendiceal anomalies is presented in Table 1[4,10-13]. Most cases can be classified on the basis of the new classification. There have been 22 cases of Type A, 8 cases of Type B1, 46 cases of Type B2, 10 cases of Type C, 2 cases of triple appendix, and 14 cases of horseshoe appendix reported as of the beginning of 2018[3,4]. Although the duplex appendix is rare, surgeons should suspect the possibility of it when performing an appendectomy to prevent adverse consequences and medical disputes. In addition, a differential diagnosis is also necessary, including Meckel's diverticulum, colonic tumor, gastroenteritis, congenital cecal diverticulum, intussusceptions, and inflam-matory bowel disease[14]. In the presence of a duplex appendix, the possibility of other congenital malformations should be further explored, especially in cases of Type B1 and Type C. However, Type B2, which is the most common variety and the most likely to be misdiagnosed or mismanaged, is unrelated to any other congenital ano-malies[3].
| Number anomalies |
| Agenesis: Absence of appendix |
| Duplex appendix |
| Type A: Partial duplication with both appendices sharing a common base like ‘’ Y-shaped’’ on a single cecum |
| Type B: Complete duplication of the appendix on a single cecum |
| B1 avian type: Two appendices symmetrically placed on either side of the ileocecal valve |
| B2 tenia coli cecum type: One appendix arising from the usual site of the cecum and the other arising from the cecum along the tenia |
| B3 tenia coli hepatic flexure type: One appendix arising from the usual site of the cecum and the other arising from the hepatic flexure of the colon along the tenia |
| B4 tenia coli splenic flexure type: One appendix arising from the usual site of the cecum and the other arising from the splenic flexure of the colon along the tenia |
| Type C: Duplication of the cecum, each having its own appendix |
| Triplex appendix: Complete triplication of appendix on the cecum |
| Horseshoe appendix |
| With sagittal disposal: The bases of the appendix are along the tenia in sagittal direction |
| With frontal disposal: The bases of the appendix are not on the tenia |
In the classification of duplex appendix, the horseshoe appendix is a rarer congenital malformation. In 1989, Mesko et al[15] first depicted the horseshoe appendix. Through a review of the literature, 14 patients with horseshoe appendix have been reported to date[4], and as per our knowledge, our patient was the 15th patient with a reported horseshoe appendix. The etiology and pathogenesis of horseshoe appendix are still unclear because there are extremely limited cases that have been reported thus far. Currently, some theories have been proposed to explain how the horseshoe appendix forms[16]. First, the horseshoe appendix may form by the mutual fusion between the tip of the normal appendix and that of the abnormal appendix. Second, a horseshoe appendix may develop from the fusion between the tip of the appendix and another part of the cecum, which then becomes the second base. Third, in the embryonic period, the base of the appendix split into two parts, each of which develops continuously, resulting in two bases that are also single structures. However, the first two theories do not seem to explain why both appendixes are supplied by a single blood vessel in the mesoappendix, and its branches fan out instead of forming an arcade. The study of the formation mechanism of the duplex appendix revealed that a “transient appendix” at the terminus of the cecum, which was distinct from the normal appendix, was observed during the 6th week of embryonic development and atrophy at the 7th week[17]. If the transient appendix does not disappear, a duplex appendix may form. Additionally, the horseshoe appendix, a subtype of the duplex appendix, may be caused by some abnormalities in the embryonic period. Therefore, the third theory is most likely to explain the formation of a horseshoe appendix. However, more research is needed to support this theory, because of the limited number of cases.
The horseshoe appendix can be divided into two types according to the following new classification system (Table 1): Frontal type, in which both bases of the appendix are not on the tenia, and sagittal type, in which the bases are along the tenia[11]. The malformation of our patient was a horseshoe type with a frontal location. In addition, we must simultaneously pay attention to whether the patient had other malformations because genitourinary, other intestinal, or vertebral malformations have been observed in cases with a duplex appendix. Fortunately, other associated congenital anomalies had not been observed in our patient, except for the endome-triosis of the small intestine and ovary. Preoperative diagnosis is extremely difficult, whether it is a horseshoe appendix or other types of duplex appendix. It has been reported that[4] ultrasound and three-dimensional reconstruction may be helpful for the preoperative diagnosis of a horseshoe appendix, but most cases are accidentally discovered during surgery, and only two patients had a clear diagnosis before surgery. In our patient, imaging failed to preoperatively diagnose appendiceal anomalies. However, after surgery, we reviewed the CT scan repeatedly, and the images showed that there were two free fecaliths at the root of the appendix, which may indicate the presence of a duplex appendix (Figure 1). This finding was easily ignored.
Endometriosis, which is defined as the growth of endometrial glands and stroma outside the uterine cavity, is a fairly common disease that affects up to 15% of women in childbearing age. Von Rokitansky first described endometriosis in 1860[18]. Several theories have been proposed to explain the pathogenesis of endometriosis, including retrograde menstruation and implantation theory, coelomic metaplasia theory, lymphovascular spread theory, direct transplantation and dissemination theory, and the cellular immunity theory which was a newly developed theory[19-21]. However, the specific etiology of endometriosis is still unclear. A variety of factors potentially contribute to the disease. Endometriosis can occur anywhere in the body, including pelvis organs, gastrointestinal tract, and pleural and pericardial cavities, but the ambilateral adnexa is the most frequent. Once involving the gastrointestinal tract, endometriosis also commonly involves the recto-sigmoid (72%), recto-vaginal septum (13%), small intestine (7%), cecum (3.6%), and appendix (3%)[18]. Endometriosis of the appendix is a rare disease, and its overall incidence ranges between 0.02% and 36.6%, which is widely variable and depends on the population being evaluated[22]. Our patient not only had rare appendix and ileum involvement but also had a duplex appendix. This dual participation has not been observed thus far.
Clinically, the symptoms of endometriosis are diverse and have been determined by the site of occurrence. Endometriosis of the appendix is usually asymptomatic, but it may also cause acute or chronic pelvic pain, appendicitis, lower gastrointestinal hemorrhage, and intussusception[19,22]. Consistent with some reports (Table 2)[19,23-27], our patient also presented the symptoms of acute appendicitis. Moreover, laparoscopic exploration also showed the presence of bloody fluid in the abdominal cavity. The hemoperitoneum is likely to be related to menstruation, because in these reports (Table 2), patients presented the symptoms of acute appendicitis during the menstrual period. As our patient presented the symptoms of appendicitis on the 5th day after the end of menstruation, we assume it to be related to the appendiceal fecalith. The occurrence of acute appendicitis may be the result of the dual effects of endometriosis and appendiceal fecalith. Moreover, our patient had a history of repeated lower abdominal pain which was associated with menstruation, consistent with some reports[23,26,27]. It suggests that hemoperitoneum and chronic abdominal pain may be important signs of endometriosis diagnosis, which further validates the theory of retrograde menstruation. Additionally, gastrointestinal endometriosis can present with episodes of abdominal pain, change in bowel habits, abdominal distention, rectal bleeding, and intestinal obstruction[28-30]. Fortunately, although small intestinal endometriosis in our case was asymptomatic, it did not cause intestinal obstruction due to timely detection.
| Ref. | Year | Age | Symptoms | Previous history | Episode time | Hemoperitoneum |
| Uncu et al[25] | 2008 | 45 | Abdominal pain and nausea | Not described | The second day of menstruation | Yes |
| Akbulut et al[26] | 2009 | 40 | Lower right quadrant pain | Lower right abdominal pain before every menstrual period for 8 or 9 yr | The third day of menstruation | Not described |
| Uwaezuoke et al[23] | 2013 | 29 | Right iliac fossa pain | One-year history of recurrent lower abdominal pain | The second day of menstruation | Yes |
| Curbelo-Peña et al[24] | 2015 | 39 | Right iliac fossa pain | Not described | Be menstruating at the time | Yes |
| Shen et al[27] | 2016 | 34 | Right iliac fossa pain | Repeated abdominal pain associated with menstruation for several months | The second day of menstruation | Yes |
| St John et al[19] | 2018 | 29 | Migratory lower right quadrant pain | Not described | The second day of menstruation | Yes |
| Our case | 2019 | 44 | Migratory lower right quadrant pain | Eight-year history of repeated lower abdominal pain | Five days after the last menstrual period ended | Yes |
The clinical manifestations of endometriosis are usually nonspecific, leading to the diagnostic dilemma. Therefore, complete preoperative examination is needed, including CT scan, magnetic resonance imaging (MRI), abdominal ultrasonography, and laboratory examination. It was reported that[31] multislice CT has a great potential for detecting alterations in the intestinal wall, especially when combined with enteroclysis. MRI has a high sensitivity (77%-93%) in the diagnosis of bowel endometriosis[32]. Unfortunately, there is currently no gold standard for the imaging diagnosis of endometriosis[20]. The serum CA125 level, which has been used to monitor the progress of endometriosis, may be a useful diagnostic indicator[33]. However, it has also been reported that CA125 is not sensitive enough to the diagnosis of endometriosis[30]. In our patient, the abdominal CT scan did not suggest endometriosis, but she had a high preoperative serum CA125 level of 69.5 U/mL. Therefore, we believe that the presence of endometriosis needs to be suspected when patient have elevated serum CA125 levels. Additionally, except for the hemoperi-toneum we have mentioned above, blueberry spot of the peritoneum and nodularity of the appendix may also indicate the presence of endometriosis during surgery[19,23]. Intraoperatively, we only found moderate hemorrhagic peritoneal fluid in our patient. However, the postoperative pathology of our patient confirmed the presence of endometriosis in the appendix, small intestine, and ovary. Therefore, laparoscopy and pathological confirmation remain the gold standard for the diagnosis of endometriosis. Given the nature of endometriosis, patients such as ours should be encouraged to refer to gynecologists for further assessment of the extent of endometriosis and for postoperative follow-up.
Acute appendicitis is a common abdominal disease. Although duplex appendix is rare, especially the horseshoe appendix, surgeons who may not encounter it throughout their careers need to be aware of the possibility of it when performing an appendectomy. In particular, preoperative CT showed two separate fecaliths at the root of the appendix, which may be a useful sign for the diagnosis of a duplex appendix. Therefore, a detailed exploration of the cecal pole and retrocecal space is encouraged to avoid misdiagnosis during surgery; misdiagnosis of appendix duplication may result in a poor clinical outcome and law dispute. In addition, women of childbearing age who have chronic pelvic pain or elevated CA125 levels need to highly suspect the possibility of endometriosis. In summary, whether laparoscopy or laparotomy is used, careful exploration of the entire abdomen is crucial and occasionally surprises us.
We wish to acknowledge Wen-Yan Shen (Department of Pathology, The Second Affiliated Hospital of Jiaxing University, Jiaxing) for her support on this case.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cobucci RNO S-Editor: Cui LJ L-Editor: Wang TQ E-Editor: Wang J
| 1. | Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910-925. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1307] [Cited by in RCA: 1301] [Article Influence: 37.2] [Reference Citation Analysis (0)] |
| 2. | Khanna AK. Appendix vermiformis duplex. Postgrad Med J. 1983;59:69-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Nageswaran H, Khan U, Hill F, Maw A. Appendiceal Duplication: A Comprehensive Review of Published Cases and Clinical Recommendations. World J Surg. 2018;42:574-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Liu J, Dong C, Wang H, Sun D, Liang R, Gao Z, Wang L. One type of duplex appendix: horseshoe appendix. Ther Clin Risk Manag. 2018;14:1987-1992. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Macpherson RI. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13:1063-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 316] [Cited by in RCA: 284] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 6. | COLLINS DC. A study of 50,000 specimens of the human vermiform appendix. Surg Gynecol Obstet. 1955;101:437-445. [PubMed] |
| 7. | Wallbridge PH. Double appendix. Br J Surg. 1962;50:346-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 74] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Biermann R, Borský D, Gogora M. Double appendicitis--a rare pathologic entity. Chirurg. 1993;64:1059-1061. [PubMed] |
| 9. | Kjossev KT, Losanoff JE. Duplicated vermiform appendix. Br J Surg. 1996;83:1259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Calotă F, Vasile I, Mogoantă S, Zavoi R, Paşalega M, Moraru E, Stoicea C. Horseshoe appendix: a extremely rare anomaly. Chirurgia (Bucur). 2010;105:271-274. [PubMed] |
| 11. | Takabatake K, Ikeda J, Furuke H, Kato C, Kishimoto T, Kumano T, Imura K, Shimomura K, Kubota T, Taniguchi F, Shioaki Y. A case of a horseshoe appendix. Surg Case Rep. 2016;2:140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Singh CG, Nyuwi KT, Rangaswamy R, Ezung YS, Singh HM. Horseshoe Appendix: An Extremely Rare Appendiceal Anomaly. J Clin Diagn Res. 2016;10:PD25-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Canbay E, Akman E. Appendix perforation in appendix duplication in a man: a case report. J Med Case Rep. 2011;5:162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Travis JR, Weppner JL, Paugh JC 2nd. Duplex vermiform appendix: case report of a ruptured second appendix. J Pediatr Surg. 2008;43:1726-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Mesko TW, Lugo R, Breitholtz T. Horseshoe anomaly of the appendix: a previously undescribed entity. Surgery. 1989;106:563-566. [PubMed] |
| 16. | DasGupta R, Reber PU, Patel AG. Horseshoe appendicitis. Eur J Surg. 1999;165:1095-1096. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Saleem A, Navarro P, Munson JL, Hall J. Endometriosis of the appendix: Report of three cases. Int J Surg Case Rep. 2011;2:16-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | St John BP, Snider AE, Kellermier H, Minhas S, Nottingham JM. Endometriosis of the appendix presenting as acute appendicitis with unusual appearance. Int J Surg Case Rep. 2018;53:211-213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Charatsi D, Koukoura O, Ntavela IG, Chintziou F, Gkorila G, Tsagkoulis M, Mikos T, Pistofidis G, Hajiioannou J, Daponte A. Gastrointestinal and Urinary Tract Endometriosis: A Review on the Commonest Locations of Extrapelvic Endometriosis. Adv Med. 2018;2018:3461209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 21. | Papavramidis TS, Sapalidis K, Michalopoulos N, Karayanopoulou G, Raptou G, Tzioufa V, Kesisoglou I, Papavramidis ST. Spontaneous abdominal wall endometriosis: a case report. Acta Chir Belg. 2009;109:778-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 22. | Mabrouk M, Raimondo D, Mastronardi M, Raimondo I, Del Forno S, Arena A, Sutherland N, Borgia A, Mattioli G, Terzano P, Seracchioli R. Endometriosis of the Appendix: When to Predict and How to Manage-A Multivariate Analysis of 1935 Endometriosis Cases. J Minim Invasive Gynecol. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Uwaezuoke S, Udoye E, Etebu E. Endometriosis of the appendix presenting as acute appendicitis: a case report and literature review. Ethiop J Health Sci. 2013;23:69-72. [PubMed] |
| 24. | Curbelo-Peña Y, Guedes-De la Puente X, Saladich-Cubero M, Molinas-Bruguera J, Molineros J, De Caralt-Mestres E. Endometriosis causing acute appendicitis complicated with hemoperitoneum. J Surg Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Uncu H, Taner D. Appendiceal endometriosis: two case reports. Arch Gynecol Obstet. 2008;278:273-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Akbulut S, Dursun P, Kocbiyik A, Harman A, Sevmis S. Appendiceal endometriosis presenting as perforated appendicitis: report of a case and review of the literature. Arch Gynecol Obstet. 2009;280:495-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 27. | Shen AY, Stanes A. Isolated Appendiceal Endometriosis. J Obstet Gynaecol Can. 2016;38:979-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Lainas P, Dammaro C, Rodda GA, Morcelet M, Prevot S, Dagher I. Appendiceal endometriosis invading the sigmoid colon: a rare entity. Int J Colorectal Dis. 2019;34:1147-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Sali PA, Yadav KS, Desai GS, Bhole BP, George A, Parikh SS, Mehta HS. Small bowel obstruction due to an endometriotic ileal stricture with associated appendiceal endometriosis: A case report and systematic review of the literature. Int J Surg Case Rep. 2016;23:163-168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 30. | Slesser AA, Sultan S, Kubba F, Sellu DP. Acute small bowel obstruction secondary to intestinal endometriosis, an elusive condition: a case report. World J Emerg Surg. 2010;5:27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 31. | Biscaldi E, Ferrero S, Fulcheri E, Ragni N, Remorgida V, Rollandi GA. Multislice CT enteroclysis in the diagnosis of bowel endometriosis. Eur Radiol. 2007;17:211-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 32. | De Ceglie A, Bilardi C, Blanchi S, Picasso M, Di Muzio M, Trimarchi A, Conio M. Acute small bowel obstruction caused by endometriosis: a case report and review of the literature. World J Gastroenterol. 2008;14:3430-3434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 69] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 33. | Bedaiwy MA, Falcone T. Laboratory testing for endometriosis. Clin Chim Acta. 2004;340:41-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 70] [Article Influence: 3.3] [Reference Citation Analysis (0)] |