Published online Aug 6, 2019. doi: 10.12998/wjcc.v7.i15.2058
Peer-review started: April 16, 2019
First decision: May 9,2019
Revised: June 17, 2019
Accepted: June 27, 2019
Article in press: June 27,2019
Published online: August 6, 2019
Processing time: 113 Days and 10.4 Hours
Solitary rectal ulcer syndrome (SRUS) is a rare rectal disorder characterized by bloody mucus in the stool, difficulty in defecation, pain, and anal swelling. To date, the etiology of this syndrome remains not well understood and the diagnosis is frequently confused with other disorders, making treatment a clinical challenge.
A 50-year-old woman presented to our hospital with a 40-d history of bloody mucus in the stool and anal swelling. SRUS was suspected. Rectoscopy revealed a large, severe ulcerous lesion. Histologically, the lesion was characterized as chronic ulcer without clear tumor cells, and the final diagnosis of SRUS was made. The patient was treated with Chinese medicine therapy, with administration of Tong Xie Yao Fang. After 3 wk of treatment, the symptoms improved significantly. At 2-mo follow-up, rectoscopy in a local hospital showed healed ulcer scars without obvious protrusion 3 cm from the anal verge.
Chinese medicine therapy represents a potential treatment of SRUS with predominant rectal bleeding, mucinous discharge, and anal swelling pain.
Core tip: Solitary rectal ulcer syndrome (SRUS) is a benign but uncommon rectal disorder. We present the case of a 50-year-old woman who suffered from SRUS for 40 d, with the symptoms of bloody mucous in the stools and anal swelling. Following our success of treatment with modified Tong Xie Yao Fang, we discuss how this traditional Chinese medicine prescription might be an effective treatment strategy for SRUS with this symptom profile.
- Citation: Zhang LL, Hao WS, Xu M, Li C, Shi YY. Modified Tong Xie Yao Fang relieves solitary rectal ulcer syndrome: A case report. World J Clin Cases 2019; 7(15): 2058-2064
- URL: https://www.wjgnet.com/2307-8960/full/v7/i15/2058.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i15.2058
Solitary rectal ulcer syndrome (SRUS) is a chronic, benign, uncommon and under-diagnosed disease. It is estimated that the annual incidence of SRUS is one of 100000 people, mainly affecting men in the third decade of life and women in the fourth decade[1]. Its symptomological profile consists of intestinal symptoms, primarily constipation, feeling of incomplete defecation, bloody or purulent stools, discomfort with falling anus, and rectal ulcers.
The diagnosis of SRUS is largely based on findings in rectoscopy and analysis of tissue biopsy. The treatment of SRUS includes local medication, improvement of bowel defecation habits, biofeedback, and surgical operation[2]. We report herein the case of a 50-year-old woman with SRUS and describe its appearance on rectoscopy and in analysis of the gross specimen following Chinese medicine therapy. The purpose of publishing this case is to report and discuss the effects of herbal therapy on SRUS.
A 50-year-old woman presented to our hospital with a 2-year history of intermittent dull pain in her left lower abdomen, a 40-d history of rectal swelling and discomfort, and a 20-d history of mucinous and bloody, loose stools.
The patient was sent to our Chinese medicine hospital on September 5, 2018. She reported having had developed intermittent left lower abdominal dull pain 2 years prior, after suffering from cold and eating irritating food. She reported no obvious cause of the rectal swelling discomfort that had developed 2 mo previously nor of the mucinous bloody, loose stools (occurring three or four times a day) 40 d prior. She also reported insomnia, and we observed her tongue to be red in color with white and thick fur, and a thin pulse.
The patient had undergone hemorrhoid surgery in 2009 and polypectomy of the cervical canal in 2011. Her father had died of a femoral fracture in the neck; otherwise, there was no medical family history.
Physical examination showed no obvious abnormality, except for a tough ulcerative mass, about 2 cm × 2 cm on the wall of the rectum at 3 cm from the anal verge. The remaining rectal mucosa showed smooth surface. Blood stains were detected on the doctor’s disposable glove after examination of the patient.
Laboratory examinations provided the following findings: Gram-positive bacilli of 40.0% (normal range: 50%-71%); Gram-negative bacilli of 45.0% (normal range: 24%-44%); antigen-stimulated interferon A of 15.0 SFCs/2.5 × 106 (normal: < 6 SFCs/2.5 × 106); specific gravity of urine of 1.008 (normal range: 1.015-1.025); total cholesterol of 5.2 mmol/L (normal: < 5.18 mmol/L); and complement C1q of 149.0 mg/L (normal range: 159-233 mg/L). The white blood cell count (5.99 × 109/L) and platelet count (4.03 × 1012/L) were normal. Findings for stool samples’ cultures, fecal occult blood, parasite eggs, and amoeba trophozoites were negative.
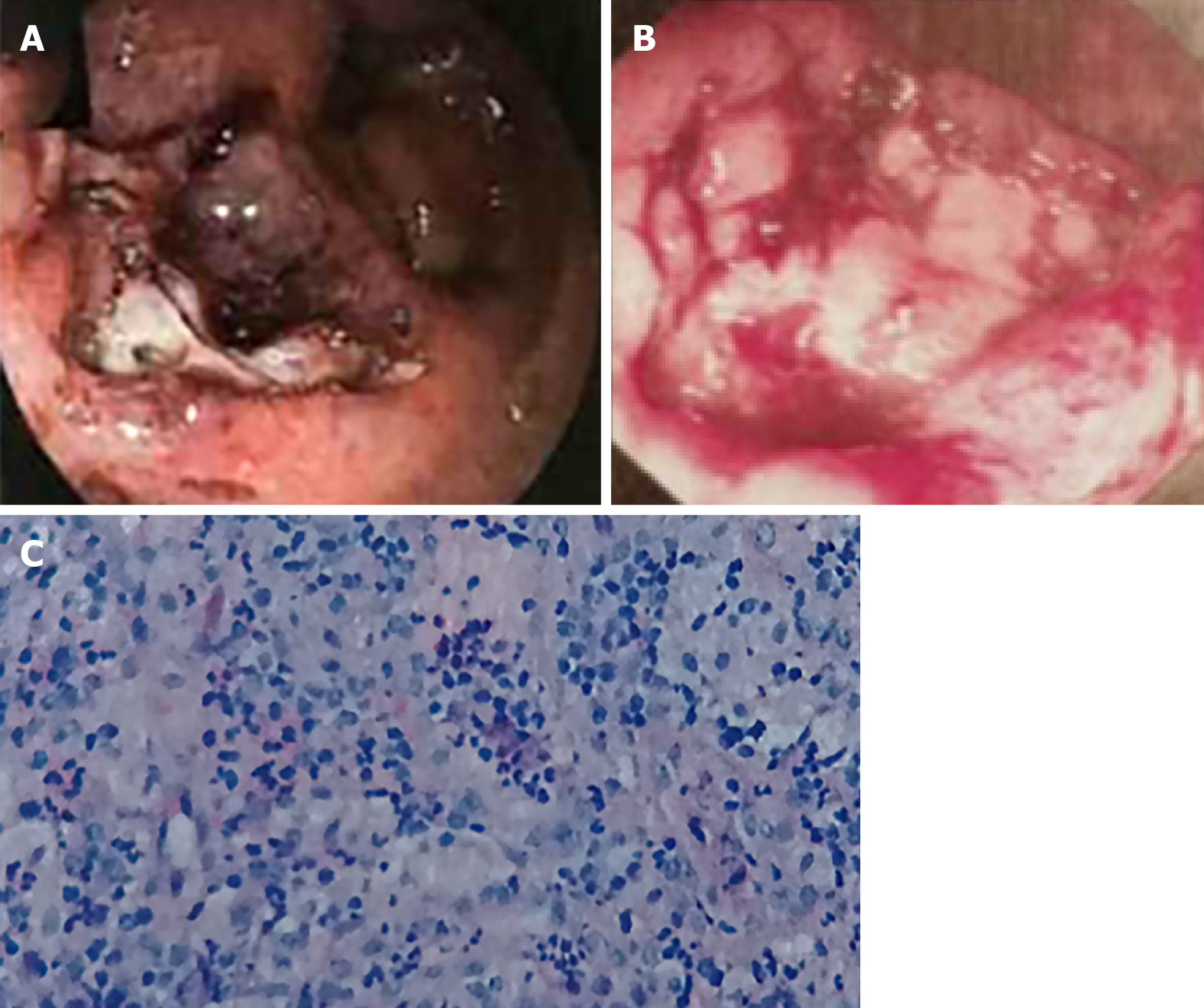
Colonoscopy revealed an irregular nodule, occupying 1/2 of the lumen, at 5 cm from the anal verge. The central ulcer was sunken, with blood stasis spotting and sloughing on the surface, as well as being brittle and bleeding easily (Figure 1A). Rectoscope showed a large ulcerative lesion at 2-4 cm from the anal margin of the rectum, occupying 3/5 of the lumen, covered by a white and bloody sloughing of tissue with central ulcer depression, as well as being brittle and prone to bleeding (Figure 1B). The pathological report noted chronic colonic mucositis, rectal mucosal erosion, and inflammatory granulation (Figure 1C).
The patient was diagnosed with SRUS, based on the findings from endoscopy of the rectum and colon (Figure 1A, B) and histology of the biopsy (Figure 1C). Her condition was deemed to be serious. Diagnosis of Traditional Chinese Medicine (TCM) was diarrhea (liver stagnation and spleen deficiency), according to the patient’s main clinical symptoms.
Treatment of modified Tong Xie Yao Fang (TXYF) was administered to soothe the qi, fortify the spleen, quiet the heart, astringe the intestines, regulate the diarrhea, and relieve the pain. The prescription was composed of Chenpi (tangerine peel; 15 g), Baishao (Radix Paeoniae Alba; 20 g), Fangfeng (Radix Saposhnikoviae; 20 g), Gaoben (Ligusticum; 10 g), Baizhu [Rhizoma Atractylodis Macrocephalae (AM); 15 g], Roudoukou (Myristica fragrans; 10 g), Buguzhi (Psoralea corylifolia; 10 g), Paojiang (prepared ginger; 10 g), Pugongying (Mongolian dandelion; 20 g), Dangshen (Radix Codonopsis; 15 g), Yuanzhi (Polygala Tenuifolia; 12 g), Shichangpu (Acorus Tatarinowii; 10 g), and Gancao (licorice; 10 g). The daily dose was decocted with water and taken at 30 min after food intake in the morning and evening. After 7 d, on September 12, 2018, the patient’s symptoms were alleviated but the patient woke early in the morning, with the continued red tongue with white and thick fur, and thin, wiry pulse. Suanzaoren (spine date seed; 20 g), Hehuanpi (Silktree Albizia bark; 10 g), and Fuling (Poria Cocos; 15 g) were added into the original prescription. The decoction and delivery method was the same as the initial ones. TCM treatment had been insisted on by the patient, who only wanted Chinese herbal medicine and no Western medicine treatment for 21 d.
On September 30, 2018, the patient was examined in the Third Affiliated Hospital of Beijing University. Rectoscopy showed an irregular shaped ulcer, 3 cm from the anal verge, about 1.0 cm × 1.2 cm in size, less white fur on the surface, flat bottom, concentrated folds around the rectum, and fusion, thickening and interruption near the ulcer; the biopsy specimen was tough, with no stenosis (Figure 2A). The pathological report noted chronic rectal ulcer mucosal inflammation, with focal lymphocyte aggregation (Figure 2B). The results suggested that the ulcer surface tended to be scarred, having improved and healed without prescribed Western medicine. The improvement of rectal symptoms in this patient should be attributed to the role of the 21 herbs administered.
During hospitalization, the patient underwent a series of examinations. Although the cause of SRUS was not found, the ulcer improved gradually with treatment. After discharge, the woman adhered to TCM treatment and also used Titanoreine, a kind of anal suppository the covers the surface of the anal and rectal mucosa with a protective membrane. On December 8, 2018, re-examination by rectoscopy in a local hospital showed that the ulcer scars had healed, without obvious protrusion, at 3 cm from the anal verge. A polyp, about 0.3 cm × 0.3 cm, was found at 3 cm from the anal verge. The surface of the mucosa was found to be smooth (Figure 2C).
The pathogenesis of SRUS is not clear, and it is often believed that SRUS might be associated with rectal prolapse and trauma from straining[3,4]. Clinically, SRUS is easy to be suspected as colorectal cancer, based on the similar symptomatic profiles and endoscopic features, which include bleeding or mucus at defecation, anal or rectal pain and discomfort, increased frequency of defecation, and colorectal masses or ulcers[1,5]. Histological features are helpful to distinguish SRUS from malignancy. The key histological features that distinguish SRUS from colorectal cancer are the architectural distortion, fibromuscular obliteration of lamina propria, and absence of tumor cell infiltration[6].
The therapeutic regimens for SRUS include conservative treatment, medical therapy, biofeedback therapy, and surgery[2]. The choice of treatment depends upon the severity of symptoms and the presence of rectal prolapse. In our case, TCM may have played a role in the successful treatment of SRUS and highlights the potential of such as a supplementary and alternative therapy. Some studies have suggested that fruits, vegetables and grains have protective effects against adenoma and colorectal cancer. Probiotics may also have preventive effects on colorectal cancer but the actual beneficial effects remain to be definitively evidenced[7,8]. Conservative treatment (high-fiber diet, laxatives, change in defecatory habits, and biofeedback treatment) were shown to induce a symptomatic improvement in 71/91 patients (63.6%) and healing of mucosal lesion in 17/51 patients (33.3%)[9]. According to those reports, SRUS may be prevented and improved by adjusting dietary structures and probiotic levels.
The basic TCM prescription combination consists of three classic Chinese formulas, (TXYF, consisting of tangerine peel, Radix Paeoniae Alba, Radix Saposhnikoviae, and Rhizoma AM), Er Shen Wan (ESW, consisting of Myristica fragrans and Psoralea corylifolia) and Ding Zhi Xiao Wan (DZXW, consisting of Codonopsis, Polygala tenuifolia Willd, Acorus Tatarinowii, and Poria Cocos). In addition, Gancao (licorice) is used to mediate other herbs. Suanzaoren (spine date seed) and Hehuanpi (Silktree Albizia bark) can be added when the patient suffers from insomnia.
TXYF is recorded in the Dan Xi Xin Fa. Form the viewpoint of TCM, it is used to relieve the pain and diarrhea caused by the incompatibility of the liver and spleen. ESW is recorded in the Pu Ji Ben Shi Fang. Differently, it is used for diarrhea due to deficiency of the spleen. At the patient’s first hospital visit, she mainly complained of pain in her left abdomen, diarrhea, mucinous defecation, and abnormal defecation. Based on TCM theory, her clinical symptoms were categorized as diarrhea. The patient had mild anxiety, depression and insomnia during her illness. DZXW can maintain the ability of learning and memory in depression, and the mechanism involves the promotion of neural stem cell proliferation in hippocampal formation[10].
TXYF is a commonly used Chinese herbal prescription for diarrhea, suggested to be effective in treating diarrhea-predominant irritable bowel syndrome (IBS-D)[11]. 5-hydroxytryptamine (5-HT) is a neurotransmitter that is widely distributed throughout the central nervous system and gastrointestinal tract, which may contribute to the symptoms of IBS. Li et al[12] demonstrated that TXYF treatment diminishes colonic 5-HT levels and alleviates the symptoms of IBS-D by favorably affecting microbiota levels in gut flora communities. Data from a study by Yin et al[13] suggested that the activity of the enteric nervous system and the regulation of 5-HT and substance P activities can be modulated by TXYF. Corticotropin-releasing hormone-receptor 2 (known as CRH-R2) is known to activate the intestinal mucosal anti-inflammatory response by regulating migration, proliferation and apoptosis of intestinal epithelial cells, as has been shown in colitis-induced mice[14], and to play an important anti-inflammatory role. Gong et al[14] demonstrated that TXYF can facilitate mucosal repair in colitis mice by regulating the CRH-R2. TXYF was also shown to improve the symptoms of postinfectious IBS by alleviating behavioral hyperalgesia and exerting antidiarrheal effects, the underlying mechanism of which involves TXYF inhibition of mucosal mast cells’ activation, down-regulation of tryptase and c-Fos expression, and reduction of serum TNF-α and histamine levels[15]. Therefore, it is suspected that TXYF may relieve the symptoms of SRUS by decreasing the defecation frequency and promoting mucosal repair.
AM is the most important herb in TXYF. Studies by Song et al[16] reveal that treatment with AM significantly stimulates the migration of intestinal epithelial cells (commonly known as IECs) through the polyamine-Kv1 channel signaling pathway, which can promote healing of intestinal injury. Findings from another study suggested that AM significantly stimulates the migration of IEC-6 cells through a polyamine-dependent mechanism, which could accelerate the healing of intestinal injury[17]. These results provide evidence for the effect of AM in treating intestinal diseases that are characterized by injury and ineffective repair of the intestinal mucosa in clinical practice.
ESW, composed of Myristica fragrans and Psoralea corylifolia, is a classical Chinese formula for astringing intestines and resolving diarrhea. The Myristica fragrans seed extract has shown protective effects against dextran sulfate sodium-induced colitis in an animal model by inhibiting proinflammatory cytokines in the colon mucosa. This indicates the potential usefulness of Myristica fragrans to address intestinal inflammation in a preventive application[18]. Psoralea corylifolia is a well-known traditional herb used because of its antibacterial activity. Corylifolinin and neobavaisoflavone are two isolated compounds of Psoralea corylifolia. Both of them have significant antibacterial activity against Staphylococcus aureus, methicillin‐resistant Staphylococcus aureus, and β‐lactamase-positive Staphylococcus aureus. Corylifolinin has been shown to produce the largest inhibitory zone (18 mm) with Staphylococcus aureus, being higher than even that of the positive control[19].
Dandelion polysaccharide has a good effect on clearing heat, resolving toxin presence, dissipating binding, and dispersing swelling. It plays an important role in the treatment of ulcerative colitis by decreasing the level of interleukin (IL)-6, which increases chronic intestinal inflammation[20,21]. Dandelion polysaccharide has also been shown to effectively regulate the expression of the IL-6 receptors (particularly the α form) and the glycoprotein 130 (commonly known as gp130) protein in the IL-6/transcriptional activator 3 (commonly known as STAT3) pathway, and then down-regulating the expressions of STAT3 and IL-6 mRNAs in intestinal tissue (of rats), thereby alleviating the colon inflammation state and protecting and repairing the mucosal tissue[21].
Many neurotransmitters, including dopamine, glutamate, norepinephrine, nitric oxide, and 5-HT and its 5-HT3 and 5-HT4 receptors are expressed in the brain and intestine. Disorder of the bidirectional communication between the intestinal tract and intestinal nervous system and brain (brain-intestinal axis) is regulated by various psychosocial and environmental factors (i.e., infection and inflammation)[22]. Therefore, the addition of spirit-regulating herbs may be useful for the recovery of gastrointestinal function.
Clinical application of TCM, DZXW, spine date seed and Silktree Albizia bark has remarkable effect on quieting the spirit and resolving depression. DZXW has been shown to effectively ameliorate learning-memory impairment in aging rats, improving their learning-memory capacity, and its mechanism may be related to a promotion of the function of the cerebral monoamine nervous system in brain tissue and a reduction in the level of lipid peroxidation in brain tissue[23]. Finally, the aqueous extract of Albizia adianthifolia leaves shows anxiolytic and antidepressant effects, and may confer neuroprotection due to alleviation of oxidative stress in the (rat) amygdala induced by 6-hydroxydopamine injection[24].
The case described herein demonstrates that Chinese formulas, specifically modified TXYF, can be effective in relieving the symptoms of SRUS. This finding provides new insight into the treatment of SRUS and a basis for further studies to determine the underlying mechanism.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Biondi A, Zielinski J S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Martin CJ, Parks TG, Biggart JD. Solitary rectal ulcer syndrome in Northern Ireland. 1971-1980. Br J Surg. 1981;68:744-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 94] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 2. | Zhu QC, Shen RR, Qin HL, Wang Y. Solitary rectal ulcer syndrome: clinical features, pathophysiology, diagnosis and treatment strategies. World J Gastroenterol. 2014;20:738-744. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 68] [Cited by in RCA: 70] [Article Influence: 6.4] [Reference Citation Analysis (5)] |
| 3. | Meurette G, Regenet N, Frampas E, Sagan C, Le Borgne J, Lehur PA. The solitary rectal ulcer syndrome. Gastroenterol Clin Biol. 2006;30:382-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Vaizey CJ, van den Bogaerde JB, Emmanuel AV, Talbot IC, Nicholls RJ, Kamm MA. Solitary rectal ulcer syndrome. Br J Surg. 1998;85:1617-1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 96] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Tjandra JJ, Fazio VW, Petras RE, Lavery IC, Oakley JR, Milsom JW, Church JM. Clinical and pathologic factors associated with delayed diagnosis in solitary rectal ulcer syndrome. Dis Colon Rectum. 1993;36:146-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Chiang JM, Changchien CR, Chen JR. Solitary rectal ulcer syndrome: an endoscopic and histological presentation and literature review. Int J Colorectal Dis. 2006;21:348-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Uccello M, Malaguarnera G, Basile F, D'agata V, Malaguarnera M, Bertino G, Vacante M, Drago F, Biondi A. Potential role of probiotics on colorectal cancer prevention. BMC Surg. 2012;12 Suppl 1:S35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 147] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 8. | Waluga M, Zorniak M, Fichna J, Kukla M, Hartleb M. Pharmacological and dietary factors in prevention of colorectal cancer. J Physiol Pharmacol. 2018;69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 9. | Gouriou C, Chambaz M, Ropert A, Bouguen G, Desfourneaux V, Siproudhis L, Brochard C. A systematic literature review on solitary rectal ulcer syndrome: is there a therapeutic consensus in 2018? Int J Colorectal Dis. 2018;33:1647-1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Shan DH, Chai JY, Wang DS, Wang CT. [Effect of Dingzhixiaowan on Neural Stem Cells of Dentate Gyrus and Learning Memory in Depression Model Rats]. Zhonghua Zhongyiyao Xuekan. 2005;23:1426-1427. |
| 11. | Chen M, Tang TC, Wang Y, Shui J, Xiao XH, Lan X, Yu P, Zhang C, Wang SH, Yao J, Zheng H, Huang DQ. Randomised clinical trial: Tong-Xie-Yao-Fang granules versus placebo for patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2018;48:160-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 12. | Li J, Cui H, Cai Y, Lin J, Song X, Zhou Z, Xiong W, Zhou H, Bian Y, Wang L. Tong-Xie-Yao-Fang Regulates 5-HT Level in Diarrhea Predominant Irritable Bowel Syndrome Through Gut Microbiota Modulation. Front Pharmacol. 2018;9:1110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 13. | Yin Y, Zhong L, Wang JW, Zhao XY, Zhao WJ, Kuang HX. Tong Xie Yao Fang relieves irritable bowel syndrome in rats via mechanisms involving regulation of 5-hydroxytryptamine and substance P. World J Gastroenterol. 2015;21:4536-4546. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Gong SS, Fan YH, Wang SY, Han QQ, Lv B, Xu Y, Chen X, He YE. Mucosa repair mechanisms of Tong-Xie-Yao-Fang mediated by CRH-R2 in murine, dextran sulfate sodium-induced colitis. World J Gastroenterol. 2018;24:1766-1778. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Ma X, Wang X, Kang N, Chen T, Ji H, Lv L, Yin X, Tian Y, Zheng R, Duan Y, Wang F, Tang X. The Effect of Tong-Xie-Yao-Fang on Intestinal Mucosal Mast Cells in Postinfectious Irritable Bowel Syndrome Rats. Evid Based Complement Alternat Med. 2017;2017:9086034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Song HP, Li RL, Chen X, Wang YY, Cai JZ, Liu J, Chen WW. Atractylodes macrocephala Koidz promotes intestinal epithelial restitution via the polyamine--voltage-gated K+ channel pathway. J Ethnopharmacol. 2014;152:163-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 34] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 17. | Song HP, Li RL, Zhou C, Cai X, Huang HY. Atractylodes macrocephala Koidz stimulates intestinal epithelial cell migration through a polyamine dependent mechanism. J Ethnopharmacol. 2015;159:23-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Kim H, Bu Y, Lee BJ, Bae J, Park S, Kim J, Lee K, Cha JM, Ryu B, Ko SJ, Han G, Min B, Park JW. Myristica fragrans seed extract protects against dextran sulfate sodium-induced colitis in mice. J Med Food. 2013;16:953-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Wang TX, Yin ZH, Zhang W, Peng T, Kang WY. [Chemical constituents from Psoralea corylifolia and their antioxidant alpha-glucosidase inhibitory and antimicrobial activities]. Zhongguo Zhongyao Zazhi. 2013;38:2328-2333. [PubMed] |
| 20. | Powell N, Lo JW, Biancheri P, Vossenkämper A, Pantazi E, Walker AW, Stolarczyk E, Ammoscato F, Goldberg R, Scott P, Canavan JB, Perucha E, Garrido-Mesa N, Irving PM, Sanderson JD, Hayee B, Howard JK, Parkhill J, MacDonald TT, Lord GM. Interleukin 6 Increases Production of Cytokines by Colonic Innate Lymphoid Cells in Mice and Patients With Chronic Intestinal Inflammation. Gastroenterology. 2015;149:456-67.e15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 21. | Wang Q, Bie YL, Wang D, Fan WT. [Effects of Dandelion polysaccharide on IL-6/STAT3 signaling pathway in ulcerative colitis rats]. Zhongguo Yingyong Shenglixue Zazhi. 2017;33:422-425. [PubMed] |
| 22. | Mach T. The brain-gut axis in irritable bowel syndrome--clinical aspects. Med Sci Monit. 2004;10:RA125-RA131. [PubMed] |
| 23. | Qu R, Ma S, Zhan Y, Xia W. [Effect of dingzhi xiaowan on learning and memory function in aging rats]. Zhongguo Linchuang Kangfu. 2004;8:684-685. |
| 24. | Beppe GJ, Dongmo AB, Foyet HS, Dimo T, Mihasan M, Hritcu L. The aqueous extract of Albizia adianthifolia leaves attenuates 6-hydroxydopamine-induced anxiety, depression and oxidative stress in rat amygdala. BMC Complement Altern Med. 2015;15:374. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |