Published online Jul 26, 2019. doi: 10.12998/wjcc.v7.i14.1850
Peer-review started: February 11, 2019
First decision: April 18, 2019
Revised: May 2, 2019
Accepted: May 23, 2019
Article in press: May 23, 2019
Published online: July 26, 2019
Processing time: 175 Days and 8.6 Hours
Total talar dislocation (TTD) is very uncommon for many orthopedic surgeons and emergency/trauma specialists. Scarce cases of TTD have been reported, mainly in the form of open fracture-dislocation injury.
We report a very rare injury of closed TTD with a follow-up period of 36 mo. Initial closed reduction was not successful because of a fractured highly unstable medial malleolus displaced into the ankle mortise, blocking the relocation of the talus. The patient was able to walk pain-free after the 3rd month of surgery. At the 36-mo follow-up, there were 10 degrees of flexion loss and 10 degrees of extension loss in the tibiotalar joint. Furthermore, 5 degrees of subtalar joint inversion-eversion loss was present.
Open reduction should be performed for closed TTDs unless closed reduction is successful.
Core tip: Total talar dislocation occurs as a result of high energy trauma and may lead to permanent disability or amputation. A non-displaced medial malleolus may prevent closed reduction of the talus if it displaces in the ankle mortise. Therefore, open reduction may be needed. Successful results are possible, ensuring that the remaining vascular supply is not harmed. Additionally, a negative Hawkins sign might not indicate talar avascular necrosis with certainty.
- Citation: Yapici F, Coskun M, Arslan MC, Ulu E, Akman YE. Open reduction of a total talar dislocation: A case report and review of the literature. World J Clin Cases 2019; 7(14): 1850-1856
- URL: https://www.wjgnet.com/2307-8960/full/v7/i14/1850.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i14.1850
The body weight is transferred to the foot by the talus, which is vulnerable to injuries because of the absence of muscular attachments. The shape of the talus and its strong ligamentous support holds it in the ankle mortise.
Total talar dislocation (TTD; dislocation of the tibiotalar, subtalar, and talonavicular joints) with or without an accompanying fracture is an extremely rare type of injury[1]. TTD accounts for 0.06% of all dislocations and 2% of all talar injuries[2]. TTD treatment is subject to complications such as avascular necrosis (AVN), osteoarthritis, and infection due to the limited talar blood supply and frequency of open injury[3-8]. The incidence of open injury among reported TTDs was reportedly to be 84.9% (73 of 86 cases) in the latest systematic review by Weston et al[9]; only three patients (3.5%) were able to be treated by closed reduction, and 50% of TTDs were associated with fractures, especially talus fracture (37.3%).
The tenuous blood supply of the talus is provided by the dorsalis pedis artery, peroneal arteries, tarsal canal and sinus arteries, deltoid artery, and their branches or anastomoses[6,10,11]. However, given the rarity of TTD, many aspects of this injury are not fully understood, and there is no established treatment protocol. Many surgeons may have never treated this type of injury in their surgical careers[12]. We aim to share our clinical experience and outcomes of this rare dislocation in order to improve the clinical understanding of TTD.
A 32-year-old man presented to the Emergency Department of our hospital after falling from a 3-meter ladder onto his feet.
The patient’s past medical history was unremarkable.
Physical examination revealed no open wounds but gross swelling and pain of either ankle. The skin was intact bilaterally. The dislocated talar head was prominent under the lateral border of the foot but did not lead to pressure necrosis or blisters. There was no neurovascular compromise bilaterally. Dorsalis pedis and tibialis posterior artery pulses were palpable. Our clinical considerations were, first, a talar dislocation and, second, a pilon fracture of the tibia.
The blood biochemistries, chest X-ray films, and arterial blood gases were normal.
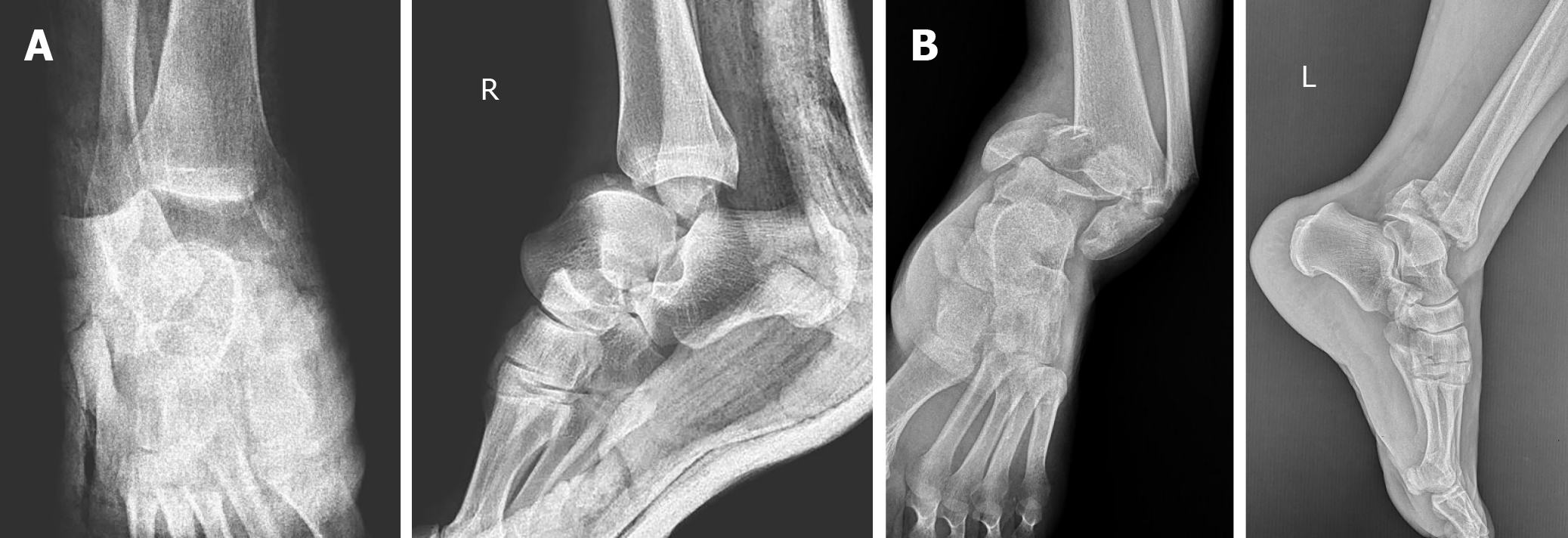
Plain films and computed tomography scans revealed anterolateral TTD and fracture of the medial malleolus on the right side and a pilon fracture on the left side (Figure 1). Plain films of the dorsolumbar vertebrae, pelvis, bilateral knee, and femur were also obtained because of the possibility of axial load fracture during the fall.
The final diagnosis was anterolateral dislocation of the talus and non-displaced medial malleolus fracture of the right ankle, and pilon fracture of the left tibia.
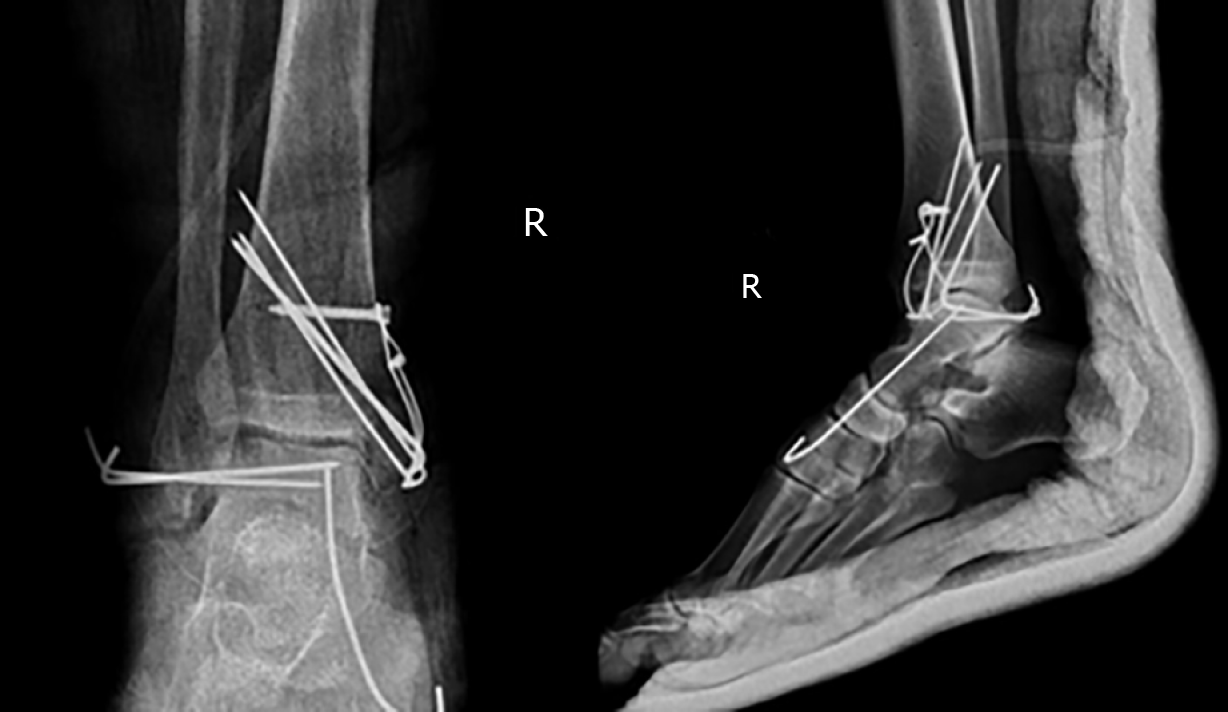
Closed reduction of the right TTD in the emergency room was not successful. During the reduction by simple traction with the knee flexed 90 degrees, the fractured highly unstable medial malleolus displaced into the ankle mortise, blocking the relocation of the talus (Figure 2). Therefore, open reduction by the medial and lateral approach was performed.
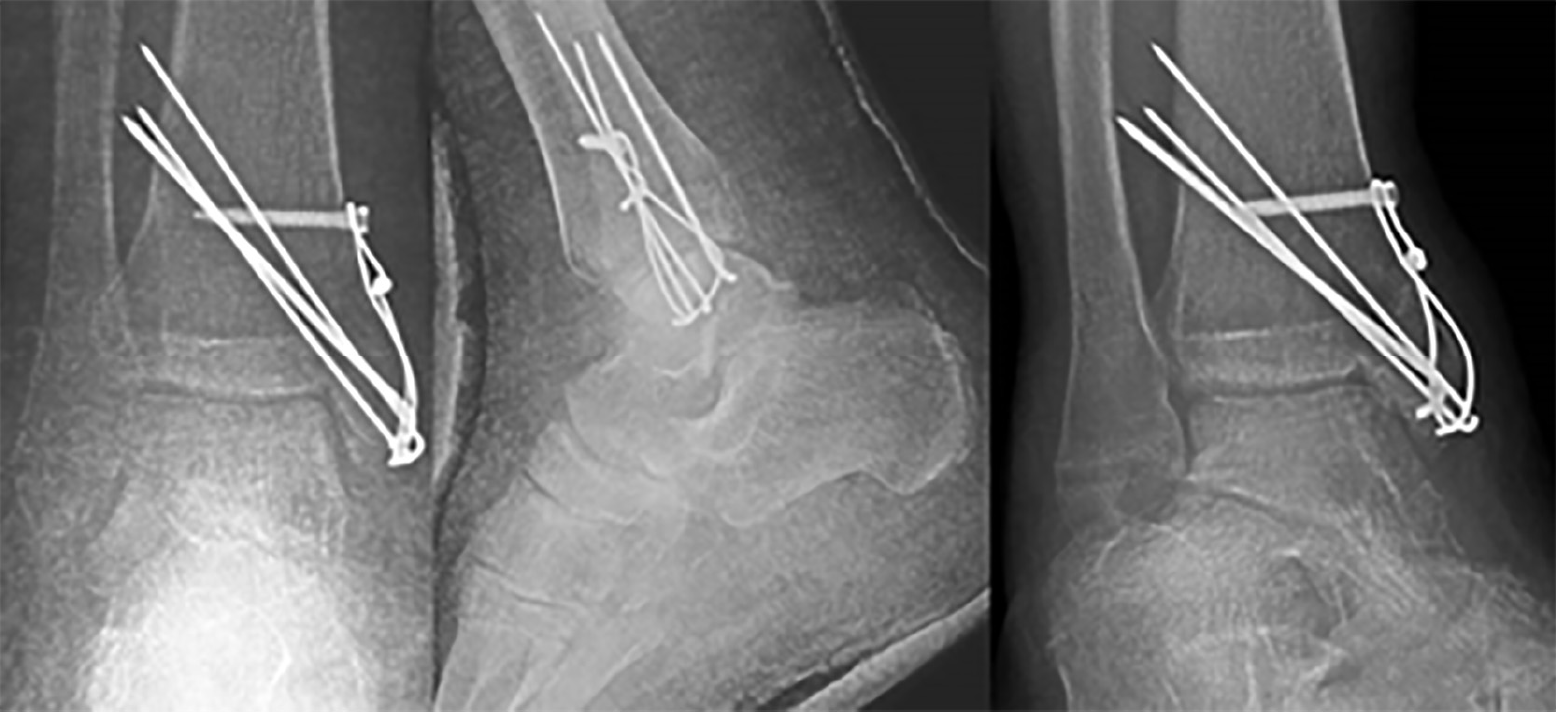
After reduction of the medial malleolus and the talus, the medial malleolus was fixed using the tension band technique (Figure 3). Next, subtalar, tibiotalar, talonavicular, and calcaneocuboid joints were checked for the tendency to dislocate. Tibiotalar and talonavicular joints were unstable. Therefore, two Kirschner (K) wires were inserted horizontally from the lateral malleolus to the talus in order to increase the stability of the tibiotalar joint. A K-wire for the talonavicular joint was used for maintenance of the reduction. A short-leg cast was placed after surgery. Due to the swelling in the left ankle, external fixation was performed in order to restore the alignment, and open reduction and internal fixation with locking anatomical plates and screws using anterolateral and posterolateral approaches were performed two weeks after the initial surgery (Figure 4).
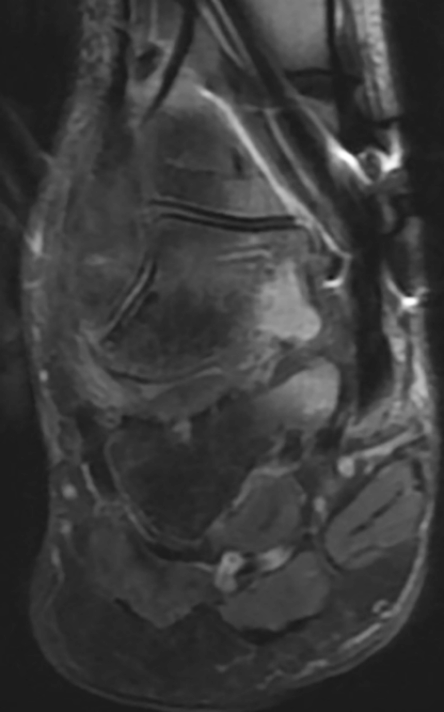
The K-wires were removed at the 6th postoperative week. After surgery, any weight-bearing was avoided for six weeks. Postoperative radiographs obtained in the 6th postoperative week revealed no Hawkins sign (Figure 5).
Hawkins sign is a subchondral radiolucent band in the talar dome that can be observed on anteroposterior ankle radiographs. This radiolucent band is formed by an increase in bone reabsorption and accompanied by active hyperemia of the talus. Therefore, the blood supply of the talus must be preserved. Hawkins sign is a good prognostic factor suggesting that the blood supply to the talus has been preserved and AVN will likely not occur[13]. The sensitivity and specificity of Hawkins sign are reported to be 100% and 57.7%, respectively, and it is present between the 6th and 9th weeks after trauma. In contrast, the absence of the Hawkins sign is not a reliable factor for predicting AVN or the development of talar collapse. In the absence of the Hawkins sign, magnetic resonance imaging (MRI) should be performed if there is any clinical or radiographic suspicion of AVN[14].
The patient was able to walk with crutches with mild pain during the 6th postoperative week and was pain-free at the third month. At 36-month follow-up, there were 10 degrees of flexion loss and 10 degrees of extension loss in the tibiotalar joint. Furthermore, 5 degrees of subtalar joint inversion-eversion loss was present.
One of the significant findings of this study is that an initially non-displaced medial malleolus may prevent closed reduction of the talus if it displaces in the ankle mortise. Therefore, open reduction may become a necessity. We speculate that closed reduction should always be the first choice of reduction to prevent disruption of the remaining tenuous vascular supply. It is possible to achieve good results even by open reduction and fixation with the necessary sensitivity to the soft tissue around talus. Another main finding is that despite the absence of Hawkins sign, a good prognosis and result are possible.
The talus has no muscular or tendinous attachments, and 60% of its surface is articular. Maintaining the position of the talus is only possible with its unique ligamentous support: The heavy talocalcaneal interosseous ligament, the anterior/posterior tibiotalar deltoid components medially, and the anterior/posterior talofibular ligaments laterally[1].
TTD is generally due to a car/motorcycle accident or a fall from a height. A rarer clinical entity called “missing talus” may occur if the talus is completely extruded out of the skin[1]. In the present case, the talus was dislocated out of the mortise but did not extrude out of the skin after the fall from a height.
Talar dislocations may be subtalar or total. Subtalar dislocation involves the talocalcaneal and talonavicular joints, whereas TTD involves tibiotalar dislocation in addition to subtalar dislocation. There are three types of TTD: anterolateral (common), medial, and posterior. This case had an anterolateral TTD involving the tibiotalar, talonavicular, and talocalcaneal joints.
TTD is generally an open-type injury. Closed TTD is an extremely infrequent injury[2]. Surgical debridement and open reduction are necessary for open TTDs. Furthermore, external fixation may be needed because of wounds, injury, and concomitant fracture. Closed reduction with sedation in the emergency room and a short-leg cast may be sufficient for closed TTDs without fracture.
Neurovascular, capsular, and ligamentous injuries and pressure necrosis are early concomitant injuries related to TTD. Late complications are more worrisome, including AVN, infection, and post-traumatic degenerative arthritis. Post-traumatic arthritis may occur even after several years. No neurovascular injuries were encountered in this case. There was an anterolateral capsular tear treated by primary suturing, and an anterior talofibular ligament sprain treated conservatively.
Good prognosis and clinical outcome without AVN or arthritis have been reported[7]. However, according to some authors, the reported prognosis was very poor[3], and the risk of post-traumatic talar AVN is as high as 90%, especially in the first year after the injury[15]. AVN is the most common complication (26%) of TTD, followed by radiographic osteoarthritis (22%), clinical osteoarthritis (16%), and infection (12%), as reported in the latest systematic review[9].
In our patient, six-week radiographs revealed no Hawkins sign. The six-week MRI revealed only talar bone bruising and edema, but no signs of AVN (Figure 6). Patients should be monitored by MRI for early AVN. Hawkins sign can be seen in serial radiographs as well. All reported closed anterolateral TTDs, as in this case, were treated by closed reduction and showed no signs of AVN at follow-up[10].
One of the major TTD series is reported by Detenbeck and Kelly[3], with the majority of cases being the open type. In Detenbeck’s mini-series of nine patients, there were seven open, and two closed TTDs. Eight developed sepsis. Seven of nine were treated by talectomy. Five patients required tibiocalcaneal arthrodesis and one required amputation.
Various treatment procedures exist, including debridement, fracture fixations if necessary, closed/open reductions, and talectomy with or without tibiocalcaneal arthrodesis for open TTDs[16]. In the Palomo-Traver’s review, closed reduction was recommended except in cases of gross contamination or complete extrusion[16]. Furthermore, there is no consensus for closed TTD treatment, such as open[7] or closed reduction[17]; however, in recent years, closed reduction has become the treatment of choice[17]. Some authors reported favorable outcomes after closed reduction[18].
Although Detenbeck and Kelly reported that total or partial talectomy might be necessary even in closed TTD[3], only two of nine patients had closed TTD, both of whom had talar fractures and the treatment was delayed because of head injury in one of them. The first closed TTD patient in Detenbeck and Kelly’s mini-series had a talus neck and body fracture treated by open reduction, internal fixation, and subtalar fusion. Two days later, the ankle joint became infected and was revised by talectomy, open drainage, and tibiocalcaneal arthrodesis. Their second patient with closed TTD also had a talar body fracture, and because of the head injury, only a compression dressing was applied for initial treatment. Septicemia developed because of hematogenous seeding of the ankle infection and draining sinuses. The second patient was also treated by talectomy and tibiocalcaneal arthrodesis.
Fixation with the K-wire may be performed in cases of with a tendency for dislocation, and cast or external fixator immobilization is recommended for six to eight weeks[7]. In the present case, we inserted two K-wires through the lateral malleolus and one K-wire through the navicular to the talus in order to maintain reduction temporarily for six weeks. Few high-level studies have reported the superiority of either closed or open reduction. Therefore, closed or open reduction appears to be a treatment of choice[7].
We believe that our study makes a significant contribution to the literature because this combination of injuries is extremely rare, and the illustration of our case will help orthopedic surgeons who encounter similar cases in the future. Nevertheless, more studies with a higher level of evidence and higher number of cases are needed to gain a better clinical understanding and treatment protocol for TTD.
In our opinion, for closed TTDs, the closed reduction should be performed first not to jeopardize the remaining vascular supply of the talus if possible. If closed reduction is unsuccessful, open reduction should be performed, as in this case. In terms of life-threatening conditions such as sepsis, talectomy with or without tibiocalcaneal fusion and amputation are the procedures to be undertaken as a last resort. Positive Hawkins sign is a good prognostic factor in terms of AVN, but absence of the sign does not indicate that AVN will likely occur.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El Ghoch M, Vidal EIO S-Editor: Ji FF L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Hiraizumi Y, Hara T, Takahashi M, Mayehiyo S. Open total dislocation of the talus with extrusion (missing talus): report of two cases. Foot Ankle. 1992;13:473-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 64] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | El Ibrahimi A, Shimi M, Elidrissi M, Daoudi A, Elmrini A. A case of closed total dislocation of talus and literature review. Am J Emerg Med. 2011;29:475.e1-475.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Detenbeck LC, Kelly PJ. Total dislocation of the talus. J Bone Joint Surg Am. 1969;51:283-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Jaffe KA, Conlan TK, Sardis L, Meyer RD. Traumatic talectomy without fracture: four case reports and review of the literature. Foot Ankle Int. 1995;16:583-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Kleiger B. Injuries of the talus and its joints. Clin Orthop Relat Res. 1976;243-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Rammelt S, Zwipp H. Talar neck and body fractures. Injury. 2009;40:120-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Wagner R, Blattert TR, Weckbach A. Talar dislocations. Injury. 2004;35 Suppl 2:SB36-SB45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 42] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Pereles TR, Koval KJ, Feldman DS. Fracture-dislocation of the neck of the talus in a ten-year-old child: a case report and review of the literature. Bull Hosp Jt Dis. 1996;55:88-91. [PubMed] |
| 9. | Weston JT, Liu X, Wandtke ME, Liu J, Ebraheim NE. A systematic review of total dislocation of the talus. Orthop Surg. 2015;7:97-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 10. | Schiffer G, Jubel A, Elsner A, Andermahr J. Complete talar dislocation without late osteonecrosis: clinical case and anatomic study. J Foot Ankle Surg. 2007;46:120-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Katz BE, Yang E. Complete closed posterior talus dislocation without fracture. Orthopedics. 2000;23:846-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Maffulli N, Francobandiera C, Lepore L, Cifarelli V. Total dislocation of the talus. J Foot Surg. 1989;28:208-212. [PubMed] |
| 13. | Donnelly EF. The Hawkins sign. Radiology. 1999;210:195-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | Tezval M, Dumont C, Stürmer KM. Prognostic reliability of the Hawkins sign in fractures of the talus. J Orthop Trauma. 2007;21:538-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Sarabia Condes JM, De Casas Fernández E, Salmerón Martínez EJ. Subtotal talus dislocation. Foot Ankle Surg. 2003;9:45-49. [DOI] [Full Text] |
| 16. | Palomo-Traver JM, Cruz-Renovell E, Granell-Beltran V, Monzonís-García J. Open total talus dislocation: case report and review of the literature. J Orthop Trauma. 1997;11:45-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Vick J. [Total dislocation of the talus]. Zentralbl Chir. 1967;92:184-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Xarchas KC, Psillakis IG, Kazakos KJ, Pelekas S, Ververidis AN, Verettas DA. Total Dislocation of the Talus without a Fracture. Open or Closed Treatment? Report of Two Cases and Review of the Literature. Open Orthop J. 2009;3:52-55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |