Published online Jul 6, 2019. doi: 10.12998/wjcc.v7.i13.1643
Peer-review started: February 27, 2019
First decision: April 18, 2019
Revised: April 28, 2019
Accepted: May 1, 2019
Article in press: May 1, 2019
Published online: July 6, 2019
Processing time: 130 Days and 23.3 Hours
Colonic diverticulosis is a common disease, and the coexistence of colonic diverticulosis and colorectal cancer is often seen clinically. It is very rare that colon cancer arises from the mucosa of a colonic diverticulum. When colon cancer arises in a diverticulum and then tends to develop outside the wall, without developing within the lumen, the differential diagnosis from complicating lesions due to colonic diverticulitis is difficult.
A 76-year-old man was admitted to a nearby clinic with a chief complaint of discomfort and urinary frequency. Since a vesicosigmoidal fistula was seen on abdominal computed tomography, he was referred to our hospital. Laparoscopic sigmoidectomy was performed because the various diagnostic findings were diagnosed as a vesicosigmoidal fistula with diverticulitis of the sigmoid colon. However, on histopathological examination, it was diagnosed as a vesicosigmoidal fistula due to colon cancer arising in the diverticulum. Laparoscopic partial resection of the bladder was performed because local recurrence was observed in the bladder wall one and a half years after surgery. It is currently one year after reoperation, but there has been no recurrence or metastasis.
Colon cancer arising in a diverticulum of the colon should be considered when diverticulitis with complications is observed.
Core tip: Cancers arising from a diverticulum of the colon are extremely rare, and few cases have been reported. Cancer of a colonic diverticulum has difficulty progressing into the lumen, and it is often difficult to identify by imaging examinations. In addition, due to the anatomical characteristics of the diverticulum, it is easy for the cancer to progress outside the colon wall. Thus, it is often in an advanced stage at the time of discovery, and careful attention is needed.
- Citation: Kayano H, Ueda Y, Machida T, Hiraiwa S, Zakoji H, Tajiri T, Mukai M, Nomura E. Colon cancer arising from colonic diverticulum: A case report. World J Clin Cases 2019; 7(13): 1643-1651
- URL: https://www.wjgnet.com/2307-8960/full/v7/i13/1643.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i13.1643
The co-existence of colorectal diverticulosis and colorectal cancer is seen clinically, and so far there have been many research reports and case reports[1-4]. However, it is extremely rare for colon cancer to develop from within a diverticulum of the colon. In this case, laparoscopic surgery was performed for a vesicosigmoidal fistula with diverticulitis of the sigmoid colon, and the postoperative histopathological examina-tion showed colon cancer arising in the diverticulum. The clinical features of colon cancer arising in the diverticulum are reviewed, along with past reports[5-20] and including this case.
Discomfort during urination and frequent urination.
A 76-year-old man became conscious of urgency when urinating three months earlier and developed frequent urination. He also recognized food residue in the urine three days earlier and consulted a nearby clinic. Since a vesicosigmoidal fistula was found on abdominal computed tomography (CT), he was referred to our hospital and admit-ted for the purpose of intensive examination and treatment.
The patient had a history of spinal posterior fusion surgery for disc herniation. There was no history of trauma, abdominal disease, abdominal surgery, or urological disease. Moreover, there was no history of colonoscopy or upper esophagogastro-duodenoscopy.
The patient was taking Olmetec OD tablets (olmesartan medoxomil) for hypertension, Allopurinol tablets (Allopurinol) for hyperuricaemia, and Urief tablets (Silodosin) and Cernilton tablets (cernitin pollen extract) for prostate enlargement. His family medical history was unremarkable.
The patient’s abdomen was smooth and soft, with no tenderness and no palpable tumor.
The results of hematological examinations were: White blood cell count 8200/μL; C-reactive protein 4.635 mg/dL; Hb 11.8 g/dL; Plt 15.3 × 104/μL; BUN 19 mg/dL; Cre 1.00 mg/dL; and HbA1c 6.1%. Thus, there was a mild inflammatory response and anemia. The tumor markers were not elevated (CEA 1 ng/mL, CA19-9 15.3 U/mL). On urinalysis, the leukocyte reaction was 3+, and occult blood was 1+.
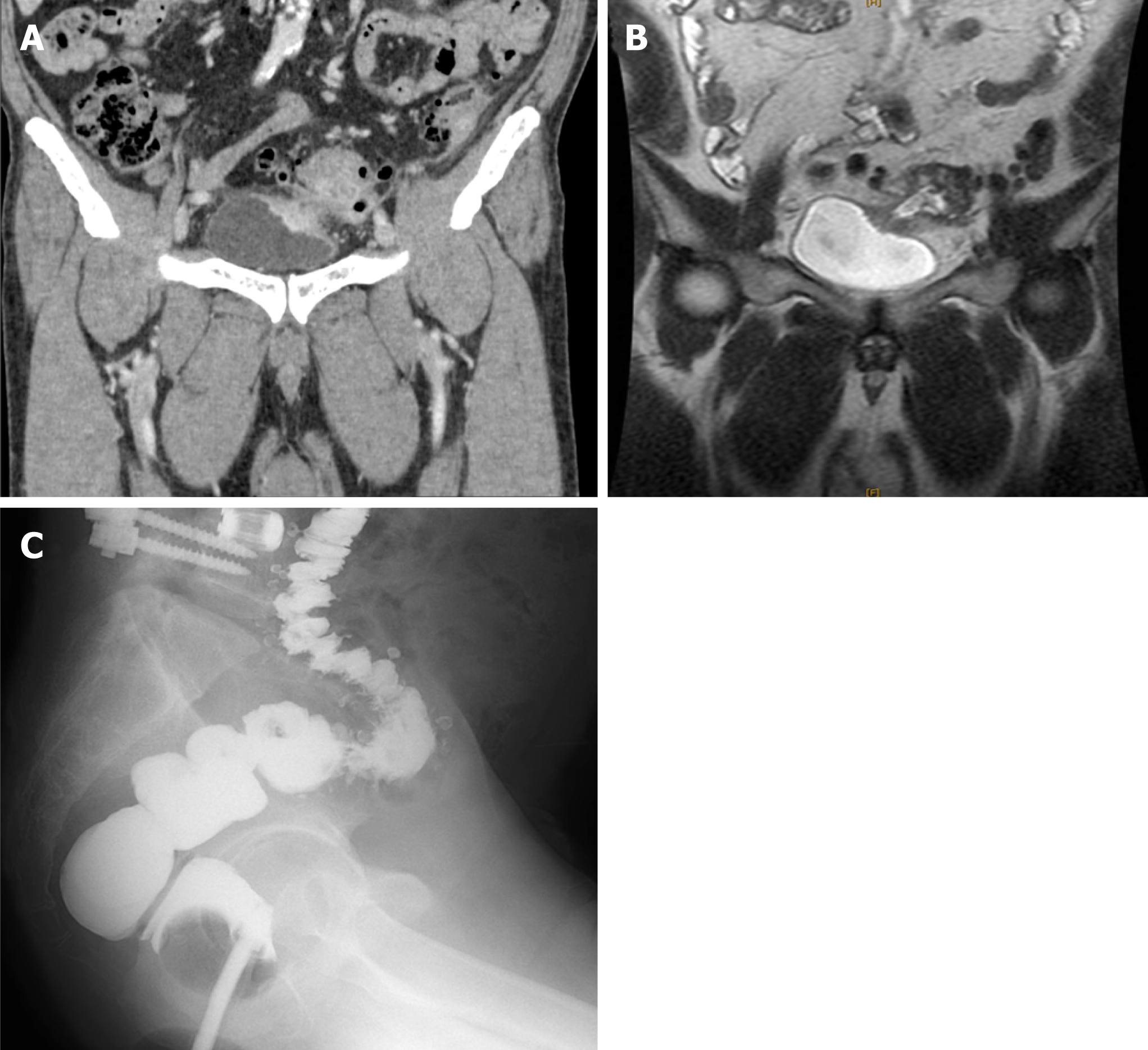
Enhanced abdominal CT showed multiple diverticula in the sigmoid colon, and an increased CT value of panniculitis was observed around the large intestinal tract. Inflammatory changes around the large intestinal tract continued to the left bladder wall, and the bladder wall was slightly thickened. Neither a tumorous lesion nor swelling of the para colic lymph nodes was seen (Figure 1A). Similarly, enhanced abdominal magnetic resonance imaging (MRI) showed a penetrating portion continuous with the sigmoid colon on the upper left side wall of the bladder. However, tumorous lesions were not seen (Figure 1B). With an enema of a water-soluble contrast agent (Figure 1C) and colonoscopy, only multiple diverticula were found in the sigmoid colon. Cystoscopy showed inflammatory changes on the mucosal surface of the bladder, but there was no fistula; no intestinal fluid flowed into the bladder, and no tumorous lesion was seen.
Vesicosigmoidal fistula with diverticulitis of the sigmoid colon.
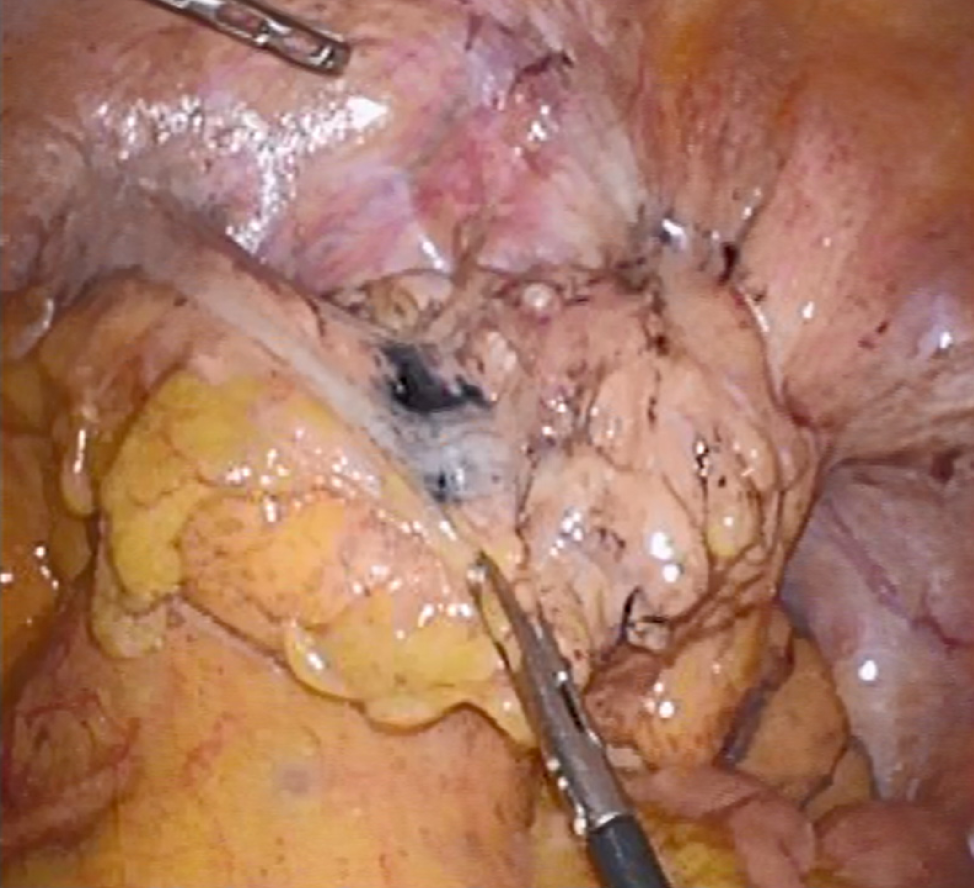
Laparoscopic sigmoidectomy and fistulectomy were performed. At surgery, fistula formation was observed in the sigmoid colon and the upper left side of the bladder wall (Figure 2). To resect the fistula, blunt dissection was first performed using a suction tube followed by sharp dissection using bipolar scissors. Although the fistula was somewhat firm, it was relatively easily separated from the surrounding tissue during the dissection. The bladder wall was preserved because no tumorous lesions that suggested cancer were observed. Finally, sigmoidectomy was performed. Anastomosis was completed with a double stapling technique, and the operation was completed. A colostomy was not created.
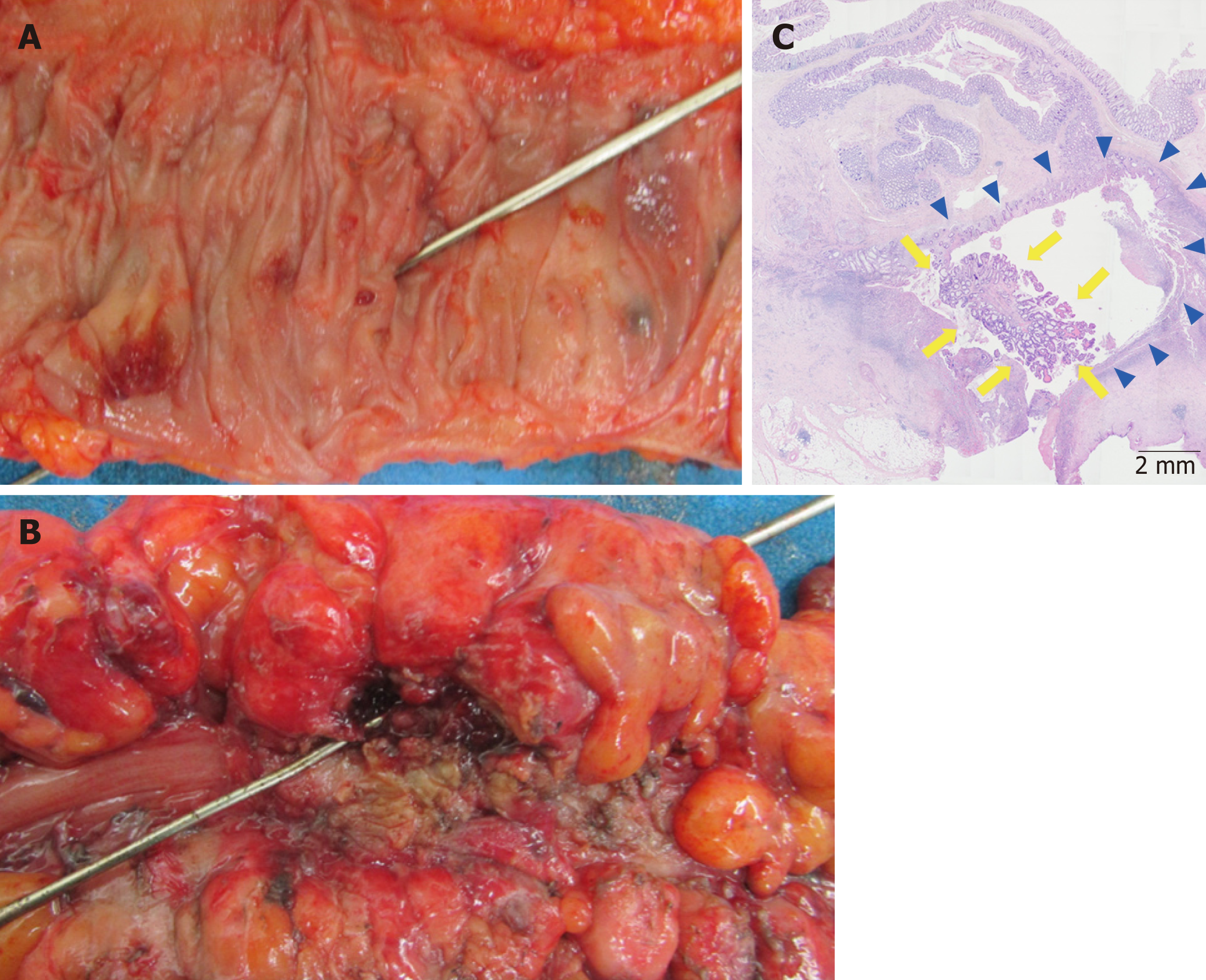
In the resected specimen, macroscopic findings only showed diffuse diverticula in the sigmoid colon lumen. A diverticulum was found in the area of fistula formation, but no tumorous lesions were observed (Figure 3A, 3B). On microscopic examination, a protruding lesion appeared toward the diverticular lumen, and well-differentiated cylindrical cancer cells proliferated in a papillary or tubular pattern, indicating a diagnosis of well-differentiated adenocarcinoma (Figure 3C). The depth of invasion was diagnosed as exceeding the serosal surface, and the resection margin was positive. Metastasis was not observed in the para colic lymph nodes near the lesions. The patient was offered additional resection, but refused. Thus, strict observation was performed. For follow-up, the patient’s serum carcinoembryonic antigen level was tested at a 3-mo interval, chest and abdomino-pelvic CT were performed at a 6-mo interval, and colonoscopy was performed at a 1-year interval.
A tumorous lesion about 1-cm in size was noted in the bladder wall on enhanced abdominal CT (Figure 4) one and a half years after the operation, and tumor biopsy was performed transurethrally by urological surgery. On histopathological examination, well-differentiated adenocarcinoma was recognized, which was similar in appearance to the cancer in the diverticulum operated previously, and it was diagnosed as recurrence in the bladder wall. The condition of the disease was again explained to the patient and family, and informed consent was obtained for laparoscopic partial resection of the bladder. On follow-up after the surgery, there has been no recurrence or metastasis one year after re-operation.
The co-existence of colonic diverticulosis, colon cancer, and adenoma is often seen clinically. However, there have been various reports as to whether there is a difference in the incidence of colorectal cancer due to the presence or absence of colonic diverticula, and the relationship is unclear[1-4]. As for the effect of the presence of diverticula on carcinogenesis, it has been reported that carcinogenesis may be caused by repeated chronic inflammation due to diverticulitis and changes in the intestinal bacterial flora caused by multiple diverticula[5]. On the other hand, colorectal cancer that arises in the diverticulum of the colon is extremely rare. The relevant English literature was retrieved from the PubMed database from 1990 to 2018 using the keywords “colon cancer”, “diverticulum”, “diverticulosis”, and “diverti-culitis”. The clinical features of cancers in diverticula were considered based on the 17 cases identified and the present case[5-20] (Table 1). The cancer was detected due to the appearance of various symptoms, such as abdominal pain, urination pain due to abscess formation, and bleeding from a tumor. Abdominal examination was performed, but only 47% (8/17) of cases were diagnosed with colorectal cancer by colonoscopy or enema before surgery, and in abdominal CT, only 37% (4/7) of cases were suspected colorectal cancer. Suspected colorectal cancer/colorectal cancer was diagnosed in about 50% (9/18) of cases preoperatively. About half of the cases were operated for complications due to colonic diverticulitis, and in many cases the diagnosis of colorectal cancer arising in the diverticulum was made for the first time after surgery. Even in the present case, it was not possible to identify the colorectal cancer in all examinations performed, including enhanced abdominal CT, enhanced abdominal MRI, and enema and colonoscopy. Therefore, it was decided to perform surgery based on the diagnosis of a vesicosigmoidal fistula caused by sigmoid colon diverticulitis. On pathological examination, no tumorous lesion was observed on macroscopic observation. Microscopic findings showed that the tumor developed slightly in the mucous membrane of the luminal side, but progressed mainly from the inside of the diverticulum in which the muscularis propria was missing. Colorectal cancer generally grows and progresses along the mucous membrane direction (horizontal development) and the membrane direction (vertical development). Compared with common colorectal cancer, the colon cancer that develops from within a diverticulum has less mucosal direction toward the luminal side (horizontal development), despite the fact that the cancer propagates easily from the diverticulum in the direction of the serosa (vertical development) out the wall. This is due to the anatomical characteristics of the diverticular lumen, which spreads widely in the colon diverticulum, but the diverticular orifice area is narrower than the diverticular lumen. Thus, it seems that it is difficult for the cancer to develop in the direction of the luminal side. Unlike usual colorectal cancer, due to such anatomical features that restrict development, it is difficult to identify lesions on colonoscopy with an enema of the lower gastrointestinal tract. Furthermore, another anatomical characteristic of the colonic diverticulum is that it is a pseudo diverticulum in which the muscularis propria is deficient, and compared with usual colorectal cancer, colon cancer that arises from within the diverticulum progresses more in the direction of the membrane towards the mucosal surface than in the direction of the mucosal surface. Therefore, at the time of detection, the depth of invasion is already above T3 in over 80% (15/18) of cases. Furthermore, infiltration into other organs is not uncommon in T4a cases (4/18 22.2%). As to the histopathological type, there were 5 cases of mucinous carcinoma (5/18, 27%). Since it is generally reported that mucinous carcinoma is seen in 3.5% to 5.1% of colon cancer cases[21-23], this is a higher rate than in normal colon cancer. Since the histopathological feature of mucinous carcinoma is development to the center of the submucosa, and it is difficult for it to be exposed on the mucosal surface, early detection is difficult. In the case of multiple diverticula, there are cases where the intestinal wall hardens or shortens and the lumen narrows due to chronic inflamma-tion; therefore, detailed observation of mucous membranes is often difficult in colonoscopy. From the above, it was thought that cancers arising from the inside of the diverticulum of the colon are difficult to identify by various examinations and are difficult to detect at an early stage. As a result, it is necessary to always keep in mind the coexistence of colon cancer in patients with colon diverticulosis/diverticulitis.
| Case | Ref. | Yr | Age (yr)/ Sex | Symptom | Seen on CT | Seen on CS/CE | Preoperativediagnosis | Tumor site | Operation | TNM (UICC) | Differentiation |
| 1 | Tolley et al[6] | 1967 | 59/M | Constipation | ND2 | Yes | Diverticulitis | Cecum | Right hemicolectomy | T4N0M0 | Mucinous |
| 2 | Drut et al[7] | 1974 | 84/M | Abdominal pain | ND | No | Diverticulitis | Sigmoid | Left hemicolectomy | T4N3M0 | Adenosqua-mous |
| 3 | Hines et al[8] | 1975 | 55/F | Abdominal pain | ND | No | Diverticulitis | Descending | Left hemicolectomy | T4N0M0 | Mucinous |
| 4 | McCrow et al[5] | 1976 | 80/M | Hematochezia | ND | No | Diverticulitis | Sigmoid | Sigmoidectomy | T3N0M0 | Mucinous |
| 5 | Prescott et al[9] | 1992 | 89/F | Abdominal pain | ND | No | Giant diverticulum | Sigmoid | Sigmoidectomy | T3N0M0 | Well |
| 6 | Cohn et al[10] | 1993 | 80/M | Abdominal pain | ND | ND | Ileus | Sigmoid | Hartmann operation | T3N0M0 | Mucinous |
| 7 | Cohn et al[10] | 1993 | 61/M | Hematochezia | ND | Yes | Bulky tumor | Sigmoid | Sigmoidectomy | T2N0M0 | Well |
| 8 | Kajiwara et al[11] | 1996 | 67/M | Hematochezia | No | Yes | Cancer | Ascending | Right hemicolectomy | T3N0M0 | Mucinous |
| 9 | Kikuchi et al[12] | 1999 | 58/F | No symptom | ND | Yes | Tumor | Cecum | Ileocecal resection | TisNxM0 | Moderate |
| 10 | Bellows et al[13] | 2002 | 63/M | Hematochezia | No | No | Vesicosigmoidal fistula | Sigmoid | Sigmoidectomy Partial resection of the urinary bladder | T4aN0M0 | Moderate |
| 11 | Van Beyrden et al[14] | 2008 | 54/M | ND | No | No | Diverticulitis | Sigmoid | Sigmoidectomy | T4aN2M0 | Moderate |
| 12 | Fu et al[15] | 2010 | 71/M | Hematochezia | ND | Yes | Tumor | Descending | EMR with the assistance of laparoscopy | TisNxM0 | Well |
| 13 | Merkow et al[16] | 2011 | 60/M | Abdominal pain | Yes | No | Bulky tumor | Sigmoid | Sigmoidectomy | T4bN2M0 | Poorly |
| 14 | Parsyan et al[18] | 2013 | 60/M | ND | Yes | Yes | Cancer | Sigmoid | Left hemicolectomy | T3N1M0 | Moderate |
| 15 | Yagi et al[19] | 2014 | 73/M | Hematuria | Yes | Yes | Cancer | Sigmoid | Sigmoidectomy, total resection of the urinary bladder | T4bN0M0 | Well |
| 16 | Nomi et al[20] | 2014 | 64/F | Anemia | Yes | No | Bulky tumor | Transverse | Right hemicolectomy | T4bN0M0 | Well |
| 17 | Our case | - | 76/M | Dysuria | No | No | Vesicosigmoidal fistula | Sigmoid | Laparoscopic sigmoidectomy | T4bN0M0 | Well |
Colon diverticulosis/diverticulitis is usually diagnosed by first performing abdominal CT examination in most cases. If there is no inflammation and only diverticula exist, careful examination such as colonoscopy cannot be performed. On the other hand, as to whether colonoscopy is necessary for colon diverticulitis found on abdominal CT, some studies[24-26] have reported that colonoscopy is not necessary for colon diverticulitis without complications, but in cases with complications such as abscess formation and penetration, the possibility of finding colon cancer or polyps increases. Moreover, it has been reported that CT findings of a wall thickness > 6 mm, abscess, lymphadenopathy, localized mass, and obstruction are predictive of malignancy[27]. One report also noted that patients with CT findings of local perfora-tion, abscess, and fistula have higher odds of malignancy than patients with diverticulitis without complications[25].
Based on the present case, it was considered important to conduct a detailed examination at the time of colonoscopy. Even when a preoperative diagnosis is made, many cases present with T4 invasion, so treatment requires combined resection. In cases where early detection was possible, even for Tis cases, which are oncologically indicated for endoscopic resection, because it is difficult to safely and completely excise tumorous lesions in diverticula without endoscopically causing perforation, some cases[15] are treated with combined laparoscopic surgery. In this case, it seems that recurrence could be prevented by performing partial resection of the bladder in addition to fistula resection as initial surgery. However, in the present case, no lesions were seen before surgery, and the presence of cancer was not considered. Moreover, surgery for a colonic urinary bladder fistula due to colon diverticulitis has been performed previously with colon resection and partial resection of the bladder, but recently, partial resection of the bladder has not been considered necessary[28,29]. From the above two perspectives, partial resection of the bladder was not performed. However, in cases of complications of abscess formation and fistula formation of colonic diverticulitis, given the possibility of cancer developing in a colonic diverti-culum as in the present case, even in the absence of mass lesions on the luminal side, it is considered necessary to add intraoperative rapid pathologic diagnosis for the fistula.
It is difficult to detect cancer arising in a diverticulum of the colon, and it is not easy to differentiate it from complications caused by diverticulitis. Therefore, with this in mind, imaging examinations and surgery are needed.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Contini S, Fabozzi M S-Editor: Dou Y L-Editor: A E-Editor: Wang J
| 1. | Jaruvongvanich V, Sanguankeo A, Wijarnpreecha K, Upala S. Risk of colorectal adenomas, advanced adenomas and cancer in patients with colonic diverticular disease: Systematic review and meta-analysis. Dig Endosc. 2017;29:73-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Kieff BJ, Eckert GJ, Imperiale TF. Is diverticulosis associated with colorectal neoplasia? A cross-sectional colonoscopic study. Am J Gastroenterol. 2004;99:2007-2011. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Soran A, Harlak A, Wilson JW, Nesbitt L, Lembersky BC, Wienad HS, O'Connell MJ. Diverticular disease in patients with colon cancer: subgroup analysis of national surgical adjuvant breast and bowel project protocol C-06. Clin Colorectal Cancer. 2006;6:140-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Choi YH, Koh SJ, Kim JW, Kim BG, Lee KL, Im JP, Kim JS, Jung HC. Do we need colonoscopy following acute diverticulitis detected on computed tomography to exclude colorectal malignancy? Dig Dis Sci. 2014;59:2236-2242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | McCraw RC, Wilson SM, Brown FM, Gardner WA. Adenocarcinoma arising in a sigmoid diverticulum: report of a case. Dis Colon Rectum. 1976;19:553-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Tolley JA. Chronic diverticulitis with perforation and associated carcinoma of the cecum. Dis Colon Rectum. 1967;10:389-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Drut R. Adenoacanthoma arising in a diverticulum of the colon: report of a case. Dis Colon Rectum. 1974;17:258-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Hines JR, Gordon RT. Adenocarcinoma arising in a diverticular abscess of the colon: report of a case. Dis Colon Rectum. 1975;18:49-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Prescott RJ, Haboubi NY, Dunaway DJ, Kiff ES. Carcinoma arising in a diverticulum of sigmoid colon. Histopathology. 1992;21:387-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Cohn KH, Weimar JA, Fani K, DeSoto-LaPaix F. Adenocarcinoma arising within a colonic diverticulum: report of two cases and review of the literature. Surgery. 1993;113:223-226. [PubMed] |
| 11. | Kajiwara H, Umemura S, Mukai M, Sadahiro S, Tsutsumi Y. Adenocarcinoma arising within a colonic diverticulum. Pathol Int. 1996;46:538-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Kikuchi T, Kotanagi H, Kon H, Koyama K, Ito S, Otaka M. Mucosal carcinoma within a colonic diverticulum. J Gastroenterol. 1999;34:622-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Bellows CF, Haque S. Adenocarcinoma within a diverticulum: a common tumor arising in an uncommon location. Dig Dis Sci. 2002;47:2758-2759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 14. | van Beurden A, Baeten CI, Lange CP, Doornewaard H, Tseng LN. Adenocarcinoma Arising within a Colonic Diverticulum in a Patient with Recurrent Diverticulitis. Clin Med Oncol. 2008;2:529-531. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Fu KI, Hamahata Y, Tsujinaka Y. Early colon cancer within a diverticulum treated by magnifying chromoendoscopy and laparoscopy. World J Gastroenterol. 2010;16:1545-1547. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (4)] |
| 16. | Merkow RP, Sun JH. Metastatic adenocarcinoma arising within a diverticulum: endoscopist's nightmare. Am Surg. 2011;77:109-110. [PubMed] |
| 17. | Anusionwu CC, Novick DM, Anusionwu NU, Akram S. Malignant Polyp in a Colonic Diverticulum: a Rare Cause of Diverticular Hemorrhage. J Gastrointest Cancer. 2012;43 Suppl 1:S104-S107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Parsyan A, Cardin MJ, Hassoun H, Andalib A, Tataryn D, Meterissian S, Roy I. Challenging diagnosis of intra-diverticular colonic adenocarcinoma with submucosal localization. Int J Colorectal Dis. 2013;28:1735-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Yagi Y, Shoji Y, Sasaki S, Yoshikawa A, Tsukioka Y, Fukushima W, Hirosawa H, Izumi R, Saito K. Sigmoid colon cancer arising in a diverticulum of the colon with involvement of the urinary bladder: a case report and review of the literature. BMC Gastroenterol. 2014;14:90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Nomi M, Umemoto S, Kikutake T, Hosaka S, Mase T, Kawamoto S, Yoshida T. [A case of carcinoma arising in a diverticulum of the transverse colon]. Gan To Kagaku Ryoho. 2014;41:1680-1682. [PubMed] |
| 21. | Greene FL, Balch CM, Page DL, Haller DG, Fleming ID, Morrow M, Fritz AG. American Joint Committee on Cancer: Staging Manual. New York: Springer 2002; . |
| 22. | Kang H, O'Connell JB, Maggard MA, Sack J, Ko CY. A 10-year outcomes evaluation of mucinous and signet-ring cell carcinoma of the colon and rectum. Dis Colon Rectum. 2005;48:1161-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 243] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 23. | Pande R, Sunga A, Levea C, Wilding GE, Bshara W, Reid M, Fakih MG. Significance of signet-ring cells in patients with colorectal cancer. Dis Colon Rectum. 2008;51:50-55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 85] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 24. | Suhardja TS, Norhadi S, Seah EZ, Rodgers-Wilson S. Is early colonoscopy after CT-diagnosed diverticulitis still necessary? Int J Colorectal Dis. 2017;32:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Lau KC, Spilsbury K, Farooque Y, Kariyawasam SB, Owen RG, Wallace MH, Makin GB. Is colonoscopy still mandatory after a CT diagnosis of left-sided diverticulitis: can colorectal cancer be confidently excluded? Dis Colon Rectum. 2011;54:1265-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 26. | Andrade P, Ribeiro A, Ramalho R, Lopes S, Macedo G. Routine Colonoscopy after Acute Uncomplicated Diverticulitis - Challenging a Putative Indication. Dig Surg. 2017;34:197-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 27. | Elmi A, Hedgire SS, Pargaonkar V, Cao K, McDermott S, Harisinghani M. Is early colonoscopy beneficial in patients with CT-diagnosed diverticulitis? AJR Am J Roentgenol. 2013;200:1269-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Royds J, O'Riordan JM, Eguare E, O'Riordan D, Neary PC. Laparoscopic surgery for complicated diverticular disease: a single-centre experience. Colorectal Dis. 2012;14:1248-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Cirocchi R, Arezzo A, Renzi C, Cochetti G, D'Andrea V, Fingerhut A, Mearini E, Binda GA. Is laparoscopic surgery the best treatment in fistulas complicating diverticular disease of the sigmoid colon? A systematic review. Int J Surg. 2015;24:95-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |