Published online Jan 6, 2019. doi: 10.12998/wjcc.v7.i1.10
Peer-review started: October 29, 2018
First decision: November 22, 2018
Revised: December 16, 2018
Accepted: December 21, 2018
Article in press: December 21, 2018
Published online: January 6, 2019
Processing time: 69 Days and 9.3 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy has been a major challenge to gastrointestinal endoscopists with low success rates for reaching the target site as well as high complication rates. The knowledge of ERCP-related risk factors is important for reducing unexpected complications.
To identify ERCP-related risk factors for perforation in patients with surgically altered anatomy.
The medical records of 187 patients with surgically altered anatomy who underwent ERCP at our institution between April 2009 and December 2017 were retrospectively reviewed. An analysis of patient data, including age, sex, type of reconstruction, cause of surgery, aim of ERCP, success rate of reaching target site, success rate of procedure, adverse events, type of scope, time to reach the target site, and duration of procedure, was performed. In patients with Billroth-II reconstruction, additional potential risk factors were the shape of the inserted scope and whether the anastomosis was antecolic or retrocolic.
All patients (n = 187) had surgical anatomy, such as Billroth-I (n = 22), Billroth-II (n = 33), Roux-en-Y (n = 54), Child, or Whipple reconstruction (n = 75). ERCP was performed for biliary drainage in 43 cases (23%), stone removal in 29 cases (16%), and stricture dilation of anastomosis in 59 cases (32%). The scope was unable to reach the target site in 17 cases (9%), and an aimed procedure could not be accomplished in 54 cases (29%). Adverse events were pancreatitis (3%), hyperamylasemia (10%), cholangitis (6%), cholestasis (4%), excessive sedation (1%), perforation (2%), and others (3%). Perforation occurred in three cases, all of which were in patients with Billroth-II reconstruction; in these patients, further analysis revealed loop-shaped insertion of the scope to be a significant risk for perforation (P = 0.01).
Risk factors for perforation during ERCP in patients with surgically altered anatomy were Billroth-II reconstruction and looping of the scope during Billroth-II procedure.
Core tip: Endoscopic retrograde cholangiopancreatography (ERCP) for patients with surgically altered anatomy accompanies a high risk of perforation. This study identified that Billroth-II reconstruction was associated with high risk of perforation during ERCP procedure. Moreover, a looping shape of a scope during insertion in patients with Billroth-II reconstruction proved to be a more specific risk factor of perforation in ERCP.
- Citation: Takano S, Fukasawa M, Shindo H, Takahashi E, Hirose S, Fukasawa Y, Kawakami S, Hayakawa H, Yokomichi H, Kadokura M, Sato T, Enomoto N. Risk factors for perforation during endoscopic retrograde cholangiopancreatography in post-reconstruction intestinal tract. World J Clin Cases 2019; 7(1): 10-18
- URL: https://www.wjgnet.com/2307-8960/full/v7/i1/10.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i1.10
Performing endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy has been a major challenge to gastrointestinal endoscopists; success rates for reaching the target site are 71%-92% and 33% in Billroth-II and Roux-en-Y reconstructions, respectively[1,2]. The development of deep enteroscopies, such as double-balloon enteroscopy (DBE) and single-balloon enteroscopy, increased those success rates to 95%-100% and 75%-100% in patients with Billroth-II[3-5] and Roux-en-Y[3,4,6-12] reconstructions, respectively. However, complication rates associated with ERCP in patients with surgically altered anatomy reportedly 10%-13%, are still high. Complications can include pancreatitis, cholangitis, aspiration pneumonia, biliary damage, and perforation[3,13]. Perforation[2] and embolic stroke-[13] related deaths have been reported rarely, and although perforations associated with sphinctectomy can be treated conservatively, those not associated with sphintectomy often require emergency surgical treatment[3,14]. Some reports show a high incidence of perforation, at rates of 2.0%-11.1%[3,8,12] and 5.6%-7.7%[2-5] in Roux-en-Y and Billroth-II reconstructions, respectively, though the overall rate of perforation in ERCP has been reported to be as low as 0.35%[15].
Surgically altered anatomy is a risk factor for perforations, not only in ERCP-related procedures, but also in DBE-related procedures[16]. The perforation rates of DBE-related procedures are reported to be 0.2% and 3% in patients without and with surgically altered anatomy, respectively, with statistical significance. Moreover, the reported incidence of perforation seems to be higher in patients with Billroth-II reconstruction[3,8,12] than in those with Roux-en-Y reconstruction[2-5], and another report showed that Billroth-II is a significant risk factor for adverse events, including perforations, in ERCP procedure with DBE[3]. However, no report has elucidated the risk factors for perforation by type of surgical anatomy and detailed operative information.
In this study, we identified risk factors for perforation in ERCP-related procedures in patients with surgically altered anatomy. We identified the type of reconstruction carrying a high risk of perforation, and we further analyzed detailed information of operative methods to identify the risks for perforation before or during DBE.
We retrospectively reviewed the medical records of 187 patients who had surgically altered anatomy and underwent ERCP-related procedures between April 2009 and December 2017 at our institution. Patient data collected were age, sex, type of reconstruction, indication for surgery, aim of ERCP, success at reaching target site, success of procedure, adverse events, type of scope, time to reach the target site, and duration of procedure.
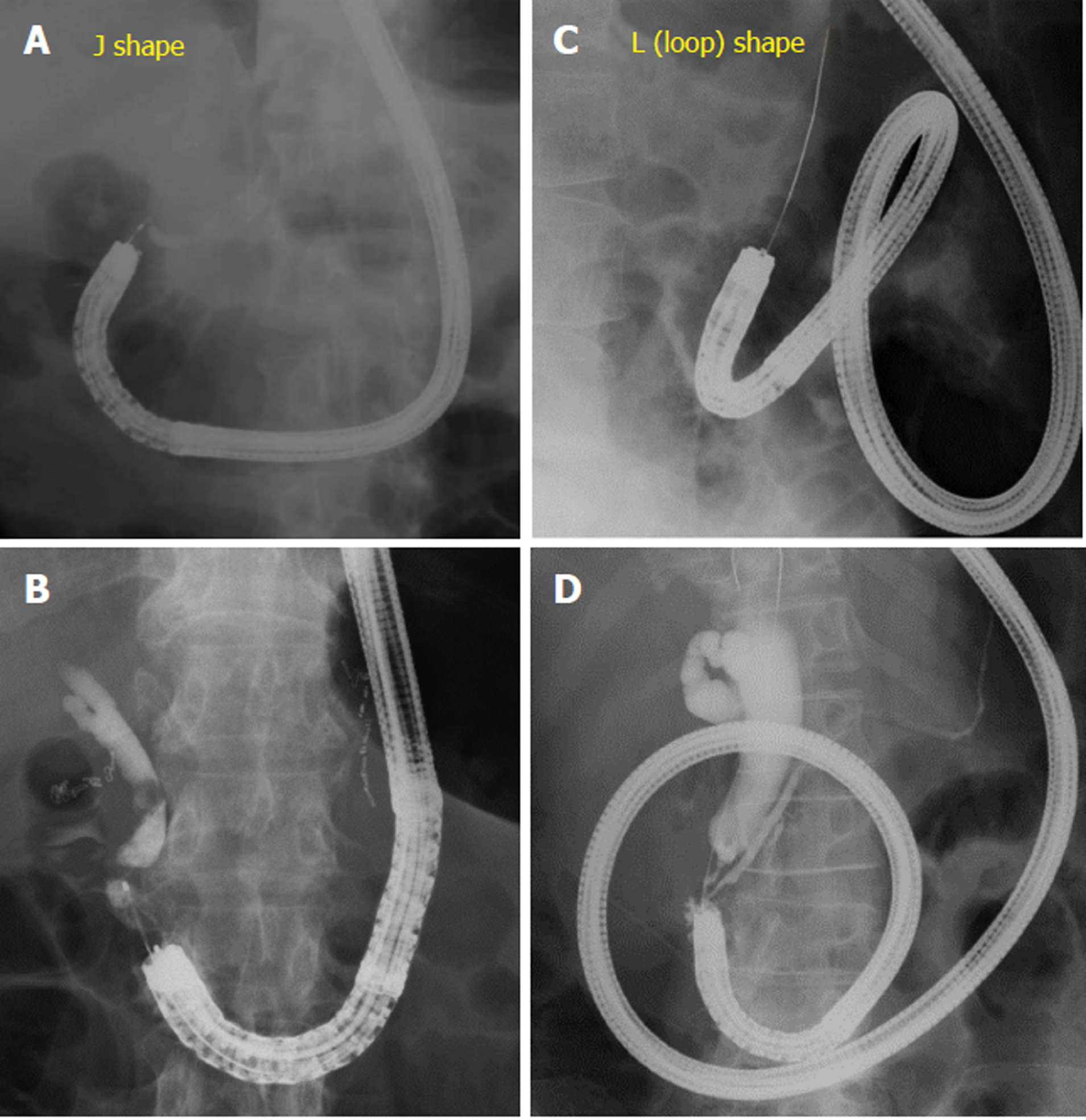
In addition to data from medical records, we extracted two other factors in cases of Billroth-II reconstruction. The first was whether reconstruction was antecolic or retrocolic. Afferent loops pass through the anterior space of transverse colon in the antecolic reconstruction, but through posterior colonic mesentery in retrocolic reconstruction. The second risk factor was the shape of inserted scope when the target site was reached. There were two scope shapes upon reaching the target site: the simple J shape (Figure 1A, 1B) and the looped, L-shaped scope (Figure 1C, 1D).
Continuous data were expressed as medians and ranges and categorical data were expressed as numbers and percentages. Two-group comparisons were conducted by χ2 test, and differences with P values of < 0.05 were considered statistically significant.
Characteristics of patients included in this retrospective study are shown in Table 1. All patients (n = 187) had surgical anatomy such as Billroth-I, Billroth-II, Roux-en-Y, Child, or Whipple reconstruction. More than half of patients underwent operation for malignant tumor, the others for benign diseases such as gastric or duodenal ulcer. ERCP was performed for biliary drainage in 43 cases (23%), stone removal in 29 cases (16%), stricture dilation of anastomosis in 59 cases (32%)(Table 2). The scope was unable to reach the target site in 17 cases (9%), and an aimed procedure could not be accomplished in 54 cases (29%).
| Parameters | Value (n = 187) | |
| Age, median (range) | 72 (31-90) | |
| Female sex, | 49 (26) | |
| Surgical anatomy | ||
| Billroth-I | 22 (12) | |
| Billroth-II | 33 (18) | |
| Roux-en-Y | 54 (29) | |
| Child or Whipple | 75 (40) | |
| Others | 3 (2) | |
| Cause of surgery | ||
| GU or DU | 30 (16) | |
| Benign disease | 14 (7) | |
| Benign tumor | 29 (16) | |
| Malignant tumor | 107 (57) | |
| N/A | 7 (4) | |
| Parameters | Value (n = 187) | |
| Failure in reaching target site | 17 (9) | |
| Failed procedure | 54 (29) | |
| Procedure | ||
| ERCP | 23 (12) | |
| Drainage | 43 (23) | |
| Stone treatment | 29 (16) | |
| Stricture dilation | 59 (32) | |
| N/A | 33 (18) | |
The incidences of adverse events are shown in Table 3. Adverse events include pancreatitis (n = 5), hyperamylasemia (n = 19), cholangitis (n = 12), cholestasis (n = 7), excessive sedation (n = 1), perforation (n = 3), and other (n = 5). The overall rate of adverse events, without overlapping, was 25% (n = 47). We next evaluated risk factors for perforation in all cases (Table 4). Among factors of age, sex, type of scope, indication for surgery, and type of surgical anatomy, only Billroth-II reconstruction was significantly associated with perforation (P = 0.003).
| Parameters | Incidence (n = 187) |
| Pancreatitis | 5 (3) |
| Hyperamylasemia | 19 (10) |
| Cholangitis | 12 (6) |
| Cholestasis | 7 (4) |
| Excessive sedation | 1 (1) |
| Perforation | 3 (2) |
| Others | 5 (3) |
| Total (no overlap) | 47 (25) |
| Parameters | n | Perforation | P value | |
| Age (yr) ≥ 75 | 68 | 2 (2.9) | 0.621 | |
| Female sex | 49 | 2 (4.1) | 0.345 | |
| Scope | ||||
| DBE | 108 | 1 (0.9) | 0.784 | |
| Other scope | 49 | 2 (4.1) | 0.345 | |
| Cause of surgery | ||||
| malignancy | 107 | 1 (0.9) | 1 | |
| Type of surgical anatomy | ||||
| B-II | 33 | 3 (9.1) | 0.003 | |
| R-Y | 54 | 0 (0.0) | 0.638 | |
That Billroth-II reconstruction is the risk factor for perforation in patients with surgically altered anatomy could easily have been predicted by previous reports, as described in the introduction section of this report. In addition, we noticed that some cases of ERCP procedure with Billroth-II reconstruction were easy, and some difficult, to perform. Therefore, we further pursued risk factors for perforation in patients with Billroth-II reconstruction, for which we extracted two more factors associated with operative methods. The two factors were whether the reconstruction was antecolic or retrocolic, and whether the shape of inserted scope was J type or L type upon reaching the target site (Figure 1). Among 33 patients with Billroth-II reconstruction, 14 cases had retrocolic reconstruction, with eight of those with the scope in an L shape when it reached the target site (Table 5). Statistical analysis revealed that only L shape; that is, loop-shaped insertion, of the scope was associated with perforation in patients with Billroth-II reconstruction.
| n | Perforation | P value | |
| Age (yr) ≥ 75 | 25 | 2 (8) | 1 |
| Female sex | 8 | 2 (25) | 0.14 |
| L shape | 8 | 3 (37.5) | 0.01 |
| Retrocolic reconstruction | 14 | 2 (14.3) | 0.56 |
| Surgery by malignancy | 10 | 1 (10) | 0.34 |
| Time to papilla (> 15 min.) | 14 | 3 (21.4) | 0.07 |
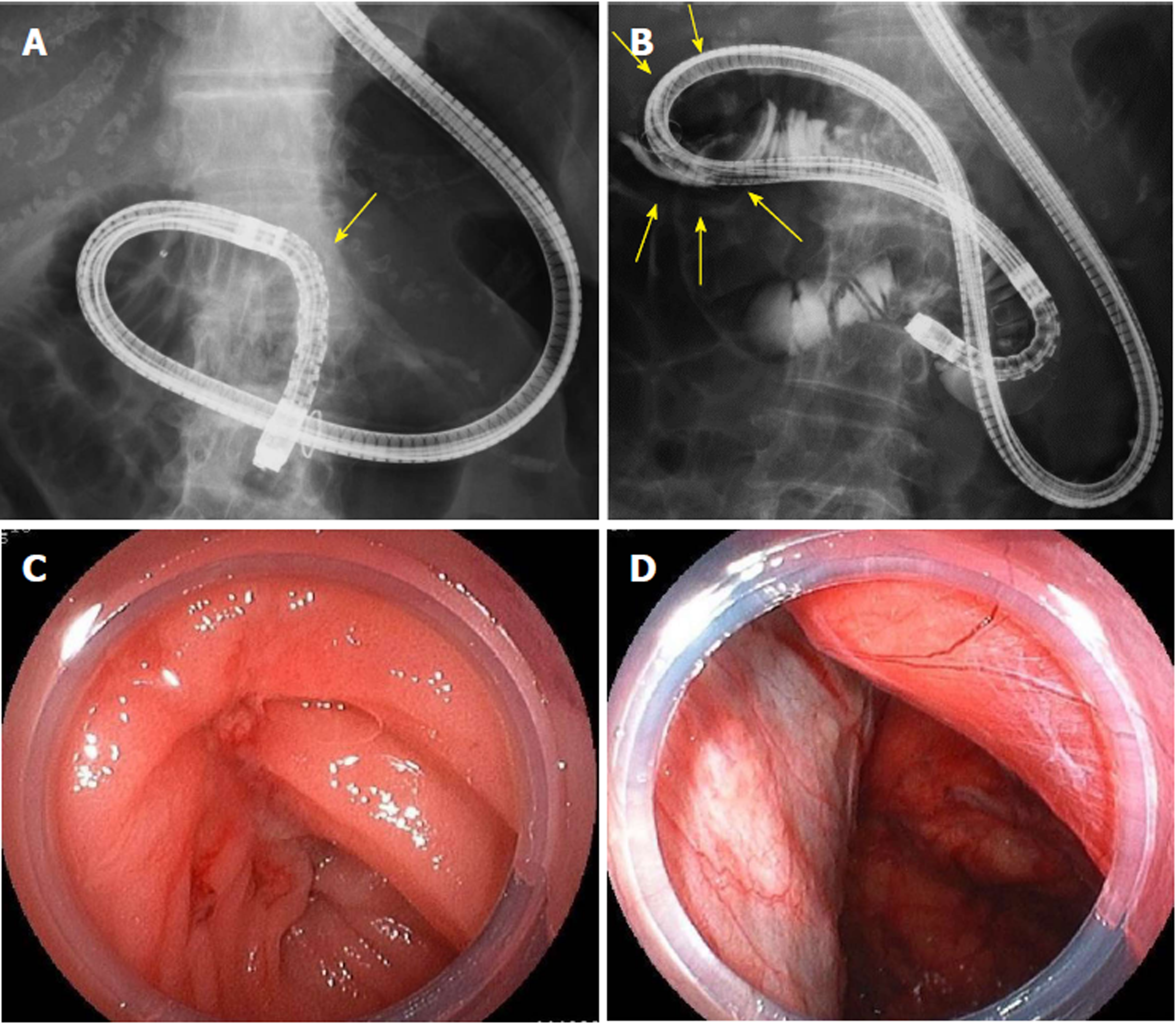
Intraoperative imaging of an 82-year-old female with perforation is shown in Figure 2. The patient had antecolic Billroth-II reconstruction and underwent ERCP with DBE to remove common bile duct stones. The scope was inserted in a loop shape and could not be advanced further than the third portion of the duodenum retrograde; perforation (arrows) occurred while pushing the scope (Figure 2B). Review of the video indicates that the reduced mobility of the scope around the perforated space, suggesting that the perforation occurred in an area of thick adhesion. Clinical characteristics of all cases with perforation are shown in Table 6 and all these cases were adequately managed by conservative therapy or operation.
| Case | Age | Sex | Diagnosis | Indication for an endoscopy | Reaching the target site | Cause of surgery | Therapy of perforation |
| 1 | 67 | F | Pancreatic cancer | Drainage | Success | Gastric cancer | Conservative |
| 2 | 83 | M | Biliary tract cancer | Drainage | Failure | Duodenal ulcer | Operation |
| 3 | 82 | F | Choledocholithiasis | Stone treatment | Failure | N/A | Operation |
This study demonstrated that Billroth-II reconstruction was a risk factor for perforation in ERCP procedures in patients with surgically altered anatomy. We further identified that looping of the scope in Billroth-II reconstruction was a risk factor for perforation in ERCP.
Surgically altered anatomy is a risk factor for perforation in both ERCP procedures and DBE examinations. No report has compared the rate of perforation in ERCP between with and without surgical altered anatomy. The overall rate of perforation in ERCP has been reported to be 0.35%[15], whereas that of patients with surgical anatomy has been reported to be 2.0%-11.1%[3,8,12] and 5.6%-7.7%[2-5] in Roux-en-Y and Billroth-II reconstruction, respectively, although there are some reports describing no incidence of perforation. Therefore, surgically altered anatomy appears to be a risk factor for perforation in ERCP. However, one report that analyzed the risk factors for complications during DBE, including perforation, suggested that the perforation rate was significantly elevated in patients with surgically altered anatomy[16]. Therefore, risk factors for perforation in patients with surgically altered anatomy should be investigated further.
Billroth-II reconstruction is a significant risk factor for perforation in ERCP procedures. The perforation rates of ERCP in patients with Roux-en-Y reconstruction are reported to be 2.1 ± 3.9%, with a median and range of 0% and 0%-11.1%, whereas those with Billroth-II reconstruction are reported to be 6.3 ± 1.1%, with a median and range of 6.7% and 5.6%-7.7% (P = 0.035). A report of a multicenter prospective study of ERCP with altered gastrointestinal anatomy demonstrated that there was an obvious perforation only in patients with Billroth-II anatomy[3]. These reports are consistent with our result that the perforation occurred only in patients with Billroth-II reconstruction.
Looping the scope during insertion proved to be a risk factor for perforation in patients with Billroth-II reconstruction. There were shown to be two types of scope insertion in patients with Billroth-II reconstruction: J type and L type. J type is a simple scope configuration that often makes it easy to reach a target site, whereas in L type, the scope forms a loop during scope insertion and sometimes makes it difficult to reach the target site. In all three patients with perforation, the scope was in an L type configuration upon reaching the target site. Review of the videos of the procedures led us to consider another possible cause of perforation in Billroth-II anatomy: the appearance of stiff adhesions at the perforation sites. We therefore added a potential risk factor, reconstruction technique in Billroth-II, for stiff adhesions after surgery. The reconstruction techniques are employed in Billroth-II and appear to be divided into two categories: whether the afferent loop passes antecolic or retrocolic. Although we did not identify a direct relationship between these reconstruction techniques and perforation, we speculate that an old surgical method may be associated with stiff adhesions, which could lead to perforation.
An intestinal tract with stiff adhesions is presumed to be easy to perforate during scope insertion of a scope, although this was not demonstrated directly in our study. Upon reviewing the videos of procedures, we noted that the intestinal tracts wherein perforation occurred did not seem flexible, suggesting those areas had stiff adhesions and were easy to perforate. One way to avoid perforation might be to insert the overtube used in deep enteroscopy beyond the adhesion site to distribute the scope’s load on the intestinal tract. Another possibility may be to have the courage to withdraw when there is little chance to achieve success.
In conclusion, the present study shows surgically altered anatomy, especially in Billroth-II reconstruction to be ERCP-related risk factors for perforation. Our findings suggest that, in patients with Billroth-II reconstruction, reaching the target site with the scope in a loop configuration carried a risk of perforation and should be performed carefully.
The development of deep enteroscopies, such as double-balloon enteroscopy (DBE) and single-balloon enteroscopy has enabled performing endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy, such as Billroth-II and Roux-en-Y reconstructions.
Surgically altered anatomy is a risk factor for perforations, not only in ERCP-related procedures, but also in DBE-related procedures. However, no report has elucidated the risk factors for perforation by type of surgical anatomy and detailed operative information.
The main objective of this study is to identify ERCP-related risk factors for perforation in patients with surgically altered anatomy.
Medical records of 187 patients with surgically altered anatomy who underwent ERCP at our institution between April 2009 and December 2017 were retrospectively reviewed and analyzed to identify risk factors for perforation.
All patients who had undergone perforation were with Billroth-II reconstruction; further analysis in these patients revealed loop-shaped insertion of the scope to be a significant risk for perforation.
The new findings of this study are that risk factors for perforation during ERCP in patients with surgically altered anatomy were Billroth-II reconstruction and looping of the scope during Billroth-II procedure.
Our findings suggest that, in patients with Billroth-II reconstruction, reaching the target site with the scope in a loop configuration carried a risk of perforation; therefore, it should be performed carefully.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Fiori E, Sinagra E S- Editor: Ma YJ L- Editor: A E- Editor: Bian YN
| 1. | Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 146] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 2. | Faylona JM, Qadir A, Chan AC, Lau JY, Chung SC. Small-bowel perforations related to endoscopic retrograde cholangiopancreatography (ERCP) in patients with Billroth II gastrectomy. Endoscopy. 1999;31:546-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 94] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 3. | Shimatani M, Hatanaka H, Kogure H, Tsutsumi K, Kawashima H, Hanada K, Matsuda T, Fujita T, Takaoka M, Yano T, Yamada A, Kato H, Okazaki K, Yamamoto H, Ishikawa H, Sugano K; Japanese DB-ERC Study Group. Diagnostic and Therapeutic Endoscopic Retrograde Cholangiography Using a Short-Type Double-Balloon Endoscope in Patients With Altered Gastrointestinal Anatomy: A Multicenter Prospective Study in Japan. Am J Gastroenterol. 2016;111:1750-1758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 120] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 4. | Osoegawa T, Motomura Y, Akahoshi K, Higuchi N, Tanaka Y, Hisano T, Itaba S, Gibo J, Yamada M, Kubokawa M, Sumida Y, Akiho H, Ihara E, Nakamura K. Improved techniques for double-balloon-enteroscopy-assisted endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:6843-6849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 47] [Cited by in RCA: 46] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 5. | Bagci S, Tuzun A, Ates Y, Gulsen M, Uygun A, Yesilova Z, Karaeren N, Dagalp K. Efficacy and safety of endoscopic retrograde cholangiopancreatography in patients with Billroth II anastomosis. Hepatogastroenterology. 2005;52:356-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 151] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 7. | Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 8. | Shimatani M, Matsushita M, Takaoka M, Koyabu M, Ikeura T, Kato K, Fukui T, Uchida K, Okazaki K. Effective “short” double-balloon enteroscope for diagnostic and therapeutic ERCP in patients with altered gastrointestinal anatomy: a large case series. Endoscopy. 2009;41:849-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 9. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 10. | Saleem A, Baron TH, Gostout CJ, Topazian MD, Levy MJ, Petersen BT, Wong Kee Song LM. Endoscopic retrograde cholangiopancreatography using a single-balloon enteroscope in patients with altered Roux-en-Y anatomy. Endoscopy. 2010;42:656-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 11. | Wang AY, Sauer BG, Behm BW, Ramanath M, Cox DG, Ellen KL, Shami VM, Kahaleh M. Single-balloon enteroscopy effectively enables diagnostic and therapeutic retrograde cholangiography in patients with surgically altered anatomy. Gastrointest Endosc. 2010;71:641-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 12. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Fukuzawa K, Moriyasu F, Tsuchida A. Long- and short-type double-balloon enteroscopy-assisted therapeutic ERCP for intact papilla in patients with a Roux-en-Y anastomosis. Surg Endosc. 2011;25:713-721. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 75] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 13. | Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A, Morgan DR, Sethi A, Stevens PD, Akerman PA, Thakkar SJ, Brauer BC. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77:593-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 228] [Cited by in RCA: 200] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 14. | Morgan KA, Fontenot BB, Ruddy JM, Mickey S, Adams DB. Endoscopic retrograde cholangiopancreatography gut perforations: when to wait! When to operate! Am Surg. 2009;75:477-83; discussion 483-4. [PubMed] |
| 15. | Enns R, Eloubeidi MA, Mergener K, Jowell PS, Branch MS, Pappas TM, Baillie J. ERCP-related perforations: risk factors and management. Endoscopy. 2002;34:293-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 179] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Gerson LB, Tokar J, Chiorean M, Lo S, Decker GA, Cave D, Bouhaidar D, Mishkin D, Dye C, Haluszka O, Leighton JA, Zfass A, Semrad C. Complications associated with double balloon enteroscopy at nine US centers. Clin Gastroenterol Hepatol. 2009;7:1177-1182, 1182.e1-1182.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 112] [Article Influence: 7.0] [Reference Citation Analysis (0)] |