Published online May 16, 2018. doi: 10.12998/wjcc.v6.i5.84
Peer-review started: December 22, 2017
First decision: February 9, 2018
Revised: February 15, 2018
Accepted: March 7, 2018
Article in press: March 7, 2018
Published online: May 16, 2018
Processing time: 144 Days and 19.4 Hours
We report a case of remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome in a 71-year-old woman. She referred to our hospital with finger stiffness, edema of both hands and feet, pain of bilateral shoulder, wrist, metacarpophalangeal, proximal interphalangeal, and ankle joints. Rheumatoid factor was negative, human leukocyte antigen -B7 antigen was positive. Moreover, matrix metalloproteinase 3 (MMP-3) was high. She was diagnosed with RS3PE syndrome, and treatment with prednisolone (15 mg/d) was started. One week after prednisolone treatment initiation, CRP decreased to negative, and joint pain was almost completely resolved. However, hand stiffness persisted, and MMP-3 level was still high. Thus, prednisolone dose was increased to 20 mg/d, and the stiffness resolved. Twenty days after treatment initiation, MMP-3 was normalized. MMP-3 was more indicative of RS3PE syndrome symptoms than CRP. Thus, MMP-3 seems to be more sensitive to RS3PE syndrome symptoms.
Core tip: We report a patient with remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome and elevation of matrix metalloproteinase 3 (MMP-3). MMP-3 was more indicative of RS3PE syndrome symptoms than CRP. Although the study of additional cases is necessary, MMP-3 seems to be more sensitive to RS3PE syndrome symptoms.
- Citation: Kenzaka T, Goda K. Serum matrix metalloproteinase 3 in detecting remitting seronegative symmetrical synovitis with pitting edema syndrome: A case report. World J Clin Cases 2018; 6(5): 84-87
- URL: https://www.wjgnet.com/2307-8960/full/v6/i5/84.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i5.84
Remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome was first reported by McCarty et al[1] in 1985. It commonly occurs in the elderly and is “remitting,” “seronegative” (namely rheumatoid factor-negative), “symmetrical,” and characterized by synovitis with pitting edema on the dorsum of the hands and feet. Additionally, patients with RS3PE are rheumatoid factor (RF)-negative. According to a report from Japan[2], it is rare disease , and the incidence rate is 0.09% in those aged 50 and over. The male: female ratio is 1:1 to 2:1 with slightly more men than women affected. About half of patients are human leukocyte antigen (HLA)-B7 antigen-positive[1].
Unlike rheumatoid arthritis or polymyalgia rheumatica, there is no clear classification criteria for RS3PE syndrome. Thus, patients are often diagnosed with RS3PE syndrome when they have the aforementioned characteristics and other diseases are ruled out. According to Olive et al[3], RS3PE syndrome is diagnosed by the following diagnostic criteria: (1) Pitting edema in the extremities; (2) acute onset; (3) age ≥ 50 years; and (4) negative findings for rheumatoid factor.
Recently, it has been reported that vascular endothelial growth factor (VEGF) and matrix metalloproteinase 3 (MMP-3) can aid in the diagnosis of RS3PE syndrome, because these patients have higher levels of both[4,5].
We experienced a case of elevated MMP-3 that proved to be more sensitive to RS3PE syndrome symptoms than CRP.
A 71-year-old woman presented to our hospital with polyarticular pain and dorsal pedal edema. She had a history of open left femur supracondylar fractures, open right lateral malleolus fractures, and fractures of the second cervical vertebral body due to traffic accident involvement 8 years prior.
Three weeks before the visit, edema suddenly appeared in the dorsum of both hands and feet. Following that, pain was experienced in bilateral shoulder, wrist, metacarpophalangeal, proximal interphalangeal, and ankle joints. Finger stiffness was also observed. She visited another hospital and was prescribed diuretics. However, the edema and pain did not improve. Thus, she was referred to our hospital.
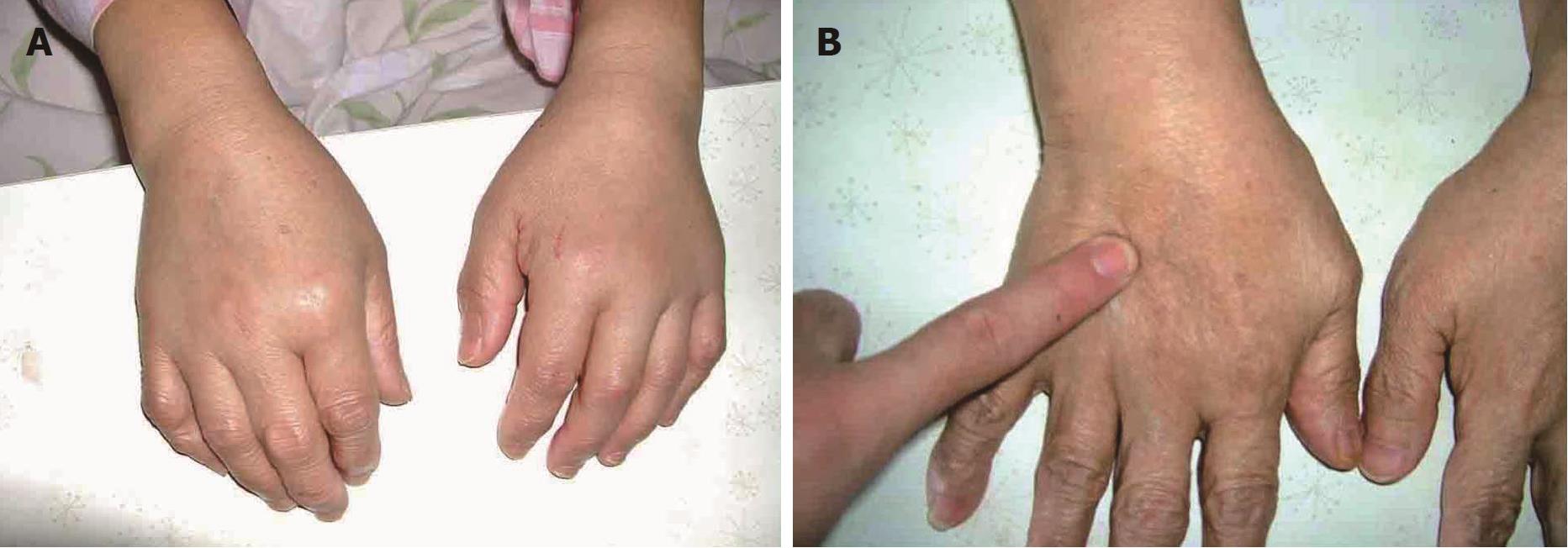
Physical characteristics and vital signs of the patient were as follows: height, 145 cm; weight, 54 kg; temperature, 36.4 °C; blood pressure, 122/64 mmHg; pulse, regular at 72 beats per minute; respiratory rate, 18 breaths/min. Her weight remained unchanged. Physical examination showed remarkable pitting edema in the dorsum of the hands and feet (Figure 1). Tenderness and swelling were observed in bilateral shoulder joints, wrist joints, all finger joints, and bilateral ankle joints. Blood test results were as follows: WBC, 5100/μL (neutrophils, 75%); CRP, 20.8 mg/dL; erythrocyte sedimentation rate, 99 mm/h; RF, negative; MMP-3488 ng/mL; VEGF, 135 pg/mL; HLA-B 7 (+) (Table 1).
| Parameter | Recorded value | Standard value |
| White blood cell count, /μL | 5100 | 4500-7500 |
| Neutrophil | 75% | |
| Lymphocyte | 18% | |
| Monocyte | 6% | |
| Hemoglobin, g/dL | 12.2 | 11.3-15.2 |
| Hematocrit | 37.1% | 36%-45% |
| Platelet, ×103/μL | 463 | 130-350 |
| Erythrocyte sedimentation rate, mm/h | 99 | 20 |
| C-reactive protein, mg/dL | 20.8 | ≤ 0.60 |
| Total protein, g/dL | 6.8 | 6.9-8.4 |
| Albumin, g/dL | 3.2 | 3.9-5.1 |
| Aspartate aminotransferase, U/L | 12 | 11-30 |
| Alanine aminotransferase, U/L | 12 | 4-30 |
| Lactate dehydrogenase, U/L | 146 | 109-216 |
| Creatine phosphokinase, U/L | 20 | 40-150 |
| Blood nitrogen urea, mg/dL | 17.4 | 8-20 |
| Creatinine, mg/dL | 0.48 | 0.63-1.03 |
| Sodium, mEq/L | 139 | 136-148 |
| Potassium, mEq/L | 4.3 | 3.6-5.0 |
| Glucose, mg/dL | 98 | 70-109 |
| Immunoglobulin G, mg/dL | 1190 | 900-2000 |
| C3, mg/dL | 128 | 86-160 |
| C4, mg/dL | 25 | 17-45 |
| Rheumatoid factor, U/mL | 2 | 2 |
| Anti-nuclear Ab | ≤ 40 | ≤ 40 |
| Anti-CCP Ab, U/mL | < 0.6 | < 4.5 |
| PR-3-ANCA, U/mL | < 1.0 | < 3.5 |
| MPO-ANCA, U/mL | < 1.0 | <3.5 |
| MMP-3, ng/mL | 488 | 36.9-121 |
| VEGF, pg/mL | 135 | < 38.3 |
| HLA-B7 | (+) |
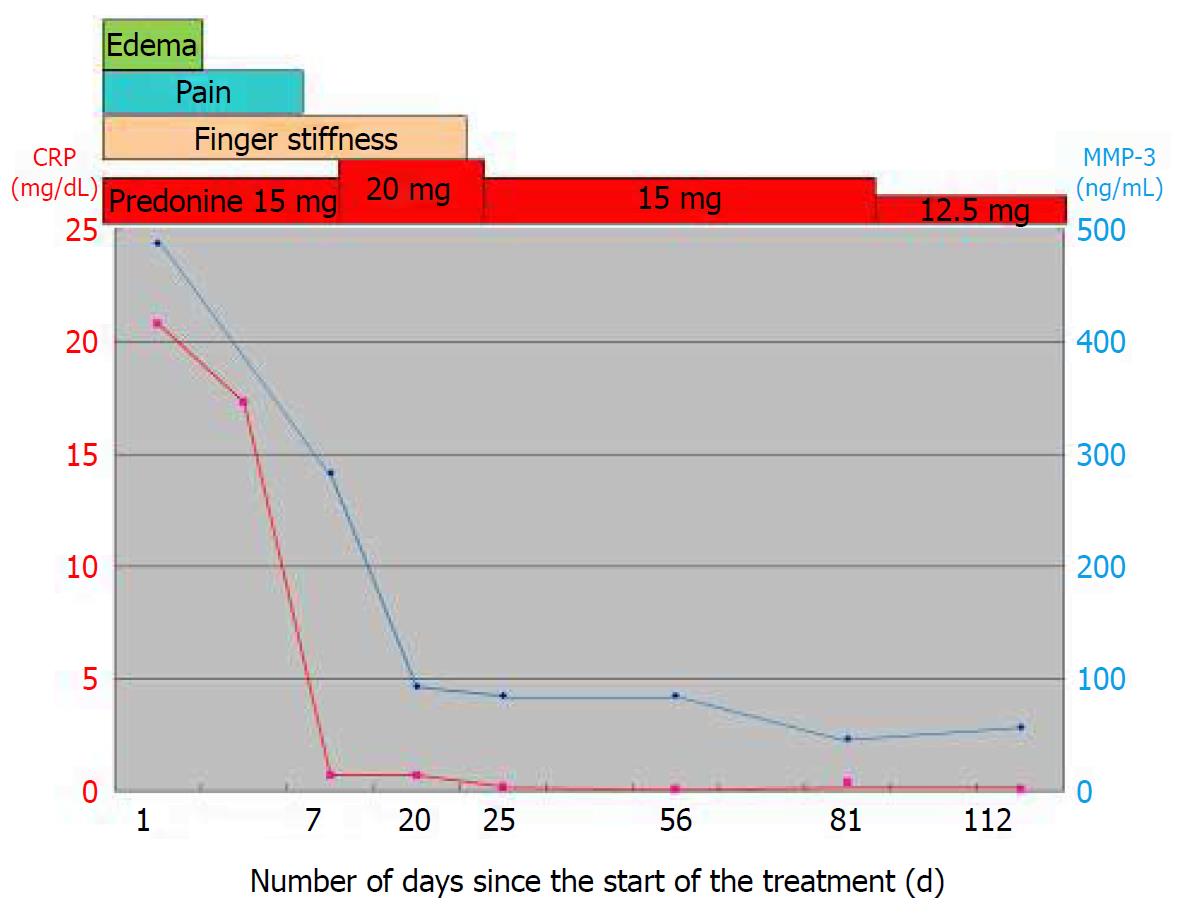
Based on the above results, she was diagnosed with RS3PE syndrome, and treatment with prednisolone (15 mg/d) was started. Within a few days, the extremity edema resolved. One week after prednisolone treatment initiation, CRP decreased to 0.7 mg/dL, and joint pain was almost completely resolved. However, hand stiffness persisted, and MMP-3 level was still high (283 ng/mL). Thus, prednisolone dose was increased to 20 mg/d, and the stiffness resolved. Twenty days after treatment initiation, MMP-3 was normalized (93 ng/mL). The clinical course is shown in Figure 2. After that, prednisolone dose prescribed in the outpatient clinic was reduced, and discontinued 1.5 years later. No relapse has been observed in 4 years of follow up. During follow-up, she underwent multiple imaging studies including chest-abdominal CT, upper and lower gastrointestinal endoscopy, thyroid ultrasonography, and echocardiography. However, no malignant tumors were found.
We report a patient with RS3PE syndrome in which elevated serum MMP-3 was more sensitive to RS3PE syndrome symptoms than CRP. To our knowledge, this is the first long-term follow-up study to establish this relationship.
MMP-3 is a proteolytic enzyme produced by joint synovial cells, chondrocytes, and fibroblasts, due to inflammatory cytokines and oxidative stress. RS3PE syndrome is known to cause inflammation in the synovium and increase MMP-3 expression[6]. In rheumatoid arthritis, which causes similar inflammation in the synovium, the disease activity score in 28 joints (DAS28) is used for the overall assessment of disease activity[7]. However, there is a report in which the combined use of serum MMP-3 and DAS28 predicted a higher clinical remission rate[8]. Additionally, one report showed that the activity score in joint ultrasonography was significantly correlated with MMP-3. Thus, MMP-3 is useful in the daily assessment of disease activity[9]. Additionally, a few reports have demonstrated that serum MMP levels are elevated in patients with RS3PE syndrome[5,10,11], while one report documented that MMP levels decrease following treatment[11].
In this study, the patient’s CRP level improved relatively quickly after the start of prednisolone treatment. Regarding clinical symptoms, edema was immediately improved. Joint pain also improved in about a week, but stiffness persisted. While objective evaluations (e.g., MRI, joint ultrasonography) were not performed, patient-reported stiffness seemed to be from mild residual synovial inflammation. This may be the reason that MMP-3 remained at a high level. After increasing prednisone dose, stiffness improved and serum MMP-3 levels were normalized. Because CRP concentration was within the normal range during this time, we believe that MMP-3 is a better predictor of symptoms.
MMP-3 is also known to be produced in breast cancer, stomach cancer, colon cancer, lung cancer, head and neck cancer, and basal cell carcinoma[5]. In RS3PE syndrome, attention should be paid to the complications of malignant tumors in patients with high MMP-3 levels[12]. It has been reported that patients with RS3PE syndrome are often observed with malignant tumors within 2 to 3 years of disease onset. However, in this patient, malignant tumors were not observed four years after the onset, and there was no recurrence of RS3PE syndrome symptoms.
In conclusion, we report a patient with RS3PE syndrome and elevation of MMP-3. MMP-3 was more indicative of RS3PE syndrome symptoms than CRP. Although the study of additional cases is necessary, MMP-3 seems to be more sensitive to RS3PE syndrome symptoms.
A 71-year-old woman was referred to our hospital with finger stiffness; edema of both hands and feet; and bilateral pain in the shoulder, wrist, metacarpophalangeal, proximal interphalangeal, and ankle joints.
Physical examination showed remarkable pitting edema in the dorsum of the hands and feet, as well as bilateral tenderness and swelling in the shoulder, wrist, finger, and ankle joints.
Remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome and rheumatoid arthritis were considered.
Blood test results were as follows: WBC, 5100/μL (neutrophils, 75%); CRP, 20.8 mg/dL; erythrocyte sedimentation rate, 99 mm/h; RF, negative; matrix metalloproteinase 3 (MMP-3) 488 ng/mL; VEGF, 135 pg/mL; HLA-B 7, (+).
Treatment with prednisolone (15 mg/d) was started.
We report a patient with RS3PE syndrome and elevation of MMP-3. MMP-3 was more indicative of RS3PE syndrome symptoms than was CRP.
CARE Checklist (2013) statement: The authors have read the CARE Checklist statement, and the manuscript was prepared and revised according to the CARE Checklist statement.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Hori T, Meteoglu I S- Editor: Cui LJ L- Editor: A E- Editor: Wang CH
| 1. | McCarty DJ, O’Duffy JD, Pearson L, Hunter JB. Remitting seronegative symmetrical synovitis with pitting edema. RS3PE syndrome. JAMA. 1985;254:2763-2767. [PubMed] |
| 2. | Okumura T, Tanno S, Ohhira M, Nozu T. The rate of polymyalgia rheumatica (PMR) and remitting seronegative symmetrical synovitis with pitting edema (RS3PE) syndrome in a clinic where primary care physicians are working in Japan. Rheumatol Int. 2012;32:1695-1699. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Olivé A, del Blanco J, Pons M, Vaquero M, Tena X. The clinical spectrum of remitting seronegative symmetrical synovitis with pitting edema. The Catalán Group for the Study of RS3PE. J Rheumatol. 1997;24:333-336. [PubMed] |
| 4. | Arima K, Origuchi T, Tamai M, Iwanaga N, Izumi Y, Huang M, Tanaka F, Kamachi M, Aratake K, Nakamura H. RS3PE syndrome presenting as vascular endothelial growth factor associated disorder. Ann Rheum Dis. 2005;64:1653-1655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Kawashiri SY, Nakano M, Kawakami A, Eguchi K. Monitoring of therapeutic efficacy in a patient with RS3PE syndrome by serologic variables and radiographic methods. Rheumatol Int. 2010;30:1677-1680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Origuchi T, Arima K, Kawashiri SY, Tamai M, Yamasaki S, Nakamura H, Tsukada T, Aramaki T, Furuyama M, Miyashita T. High serum matrix metalloproteinase 3 is characteristic of patients with paraneoplastic remitting seronegative symmetrical synovitis with pitting edema syndrome. Mod Rheumatol. 2012;22:584-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Fransen J, van Riel PL. The Disease Activity Score and the EULAR response criteria. Rheum Dis Clin North Am. 2009;35:745-757, vii-viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 217] [Cited by in RCA: 275] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 8. | Urata Y, Uesato R, Tanaka D, Nakamura Y, Motomura S. Treating to target matrix metalloproteinase 3 normalisation together with disease activity score below 2.6 yields better effects than each alone in rheumatoid arthritis patients: T-4 Study. Ann Rheum Dis. 2012;71:534-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Gorai M, Ogasawara M, Matsuki Y, Yamada Y, Murayama G, Sugisaki N, Nemoto T, Ando S, Minowa K, Kon T. Weighting with the Lansbury articular index improves the correlation of ultrasound score with serum matrix metalloproteinase-3 level in rheumatoid arthritis patients. Mod Rheumatol. 2014;24:915-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Kato T, Ubara Y, Sawa N, Tagami T, Katori H, Takemoto F, Hara S, Takaichi K. An abrupt onset of seropositive polyarthritis with prominent distal tenosynovitis concomitant with bronochiolitis obliterans organizing pneumonia (BOOP): consideration of the relationship with RS3PE syndrome. Intern Med. 2004;43:143-147. [PubMed] |
| 11. | Yanai H, Yoshida H, Tada N. Clinical, radiological, and biochemical characteristics in patients with diseases mimicking polymyalgia rheumatica. Clin Interv Aging. 2009;4:391-395. [PubMed] |
| 12. | Origuchi T, Arima K, Kawashiri SY, Tamai M, Yamasaki S, Nakamura H, Tsukada T, Aramaki T, Furuyama M, Miyashita T. High serum matrix metalloproteinase 3 is characteristic of patients with paraneoplastic remitting seronegative symmetrical synovitis with pitting edema syndrome. Mod Rheumatol. 2012;22:584-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |