Published online Dec 26, 2018. doi: 10.12998/wjcc.v6.i16.1194
Peer-review started: September 18, 2018
First decision: October 11, 2018
Revised: November 12, 2018
Accepted: November 23, 2018
Article in press: November 24, 2018
Published online: December 26, 2018
Processing time: 97 Days and 18.7 Hours
Primary sebaceous carcinoma of lacrimal gland (SCLG) is extremely rare. Due to its clinical characteristics, it is often misdiagnosed. It is known to be aggressive so delay in diagnosis can increase the chance of local recurrence and metastasis. We report a case of primary SCLG.
A 75-year-old man was referred with a painful swelling in the right eyelid. Computed tomography scan demonstrates a 2.6 cm mass in upper outer quadrant of right orbit. After the incisional biopsy of the mass, he was diagnosed with squamous cell carcinoma of lacrimal gland. A right orbital exenteration, cervical lymph node dissection was performed. There was no involvement of the overlying periorbital skin, eyelid, or conjunctiva. Histological examination of the exenteration specimen showed tumor arising from the lacrimal gland, which had been entirely replaced by sebaceous carcinoma with sarcomatous and squamous differentiation. Neoplastic cells which were large and contained prominent nucleoli. Focal tumor remained in the posterior resection margin. Patient underwent adjuvant radiotherapy, total dose of 56 Gy with dose-per-fraction 2 Gy to primary lesion. There has been no sign of recurrence until 2-years follow-up.
We report a rare case of sebaceous carcinoma arising from the lacrimal gland. Accurate diagnosis of SCLG is important for appropriate treatment and prognosis prediction.
Core tip: A 75-year-old man was referred with a painful swelling in the right eyelid. After the incisional biopsy of the mass, he was diagnosed with squamous cell carcinoma of lacrimal gland. A right orbital exenteration, cervical lymph node dissection was performed. Histological examination of the exenteration specimen showed tumor arising from the lacrimal gland, which had been entirely replaced by sebaceous carcinoma with sarcomatous and squamous differentiation. Patient underwent adjuvant radiotherapy, total dose of 56 Gy with dose-per-fraction 2 Gy to primary lesion. Sebaceous carcinoma of lacrimal gland has high morbidity and mortality rates; therefore, accurate and early diagnosis is important.
- Citation: Park H, Choi SG. Primary sebaceous carcinoma of lacrimal gland: A case report and review of literature. World J Clin Cases 2018; 6(16): 1194-1198
- URL: https://www.wjgnet.com/2307-8960/full/v6/i16/1194.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i16.1194
Tumors of the lacrimal gland are rare and present in less than one per 1000000 individuals per year[1]. Among tumors of the lacrimal gland, sebaceous carcinoma of the lacrimal gland (SCLG) is extremely rare. Only several case studies have been reported to date[2-6]. In the present study, we reviewed our case of SCLG to investigate clinical features, diagnosis and treatment of SCLG, especially with radiotherapy.
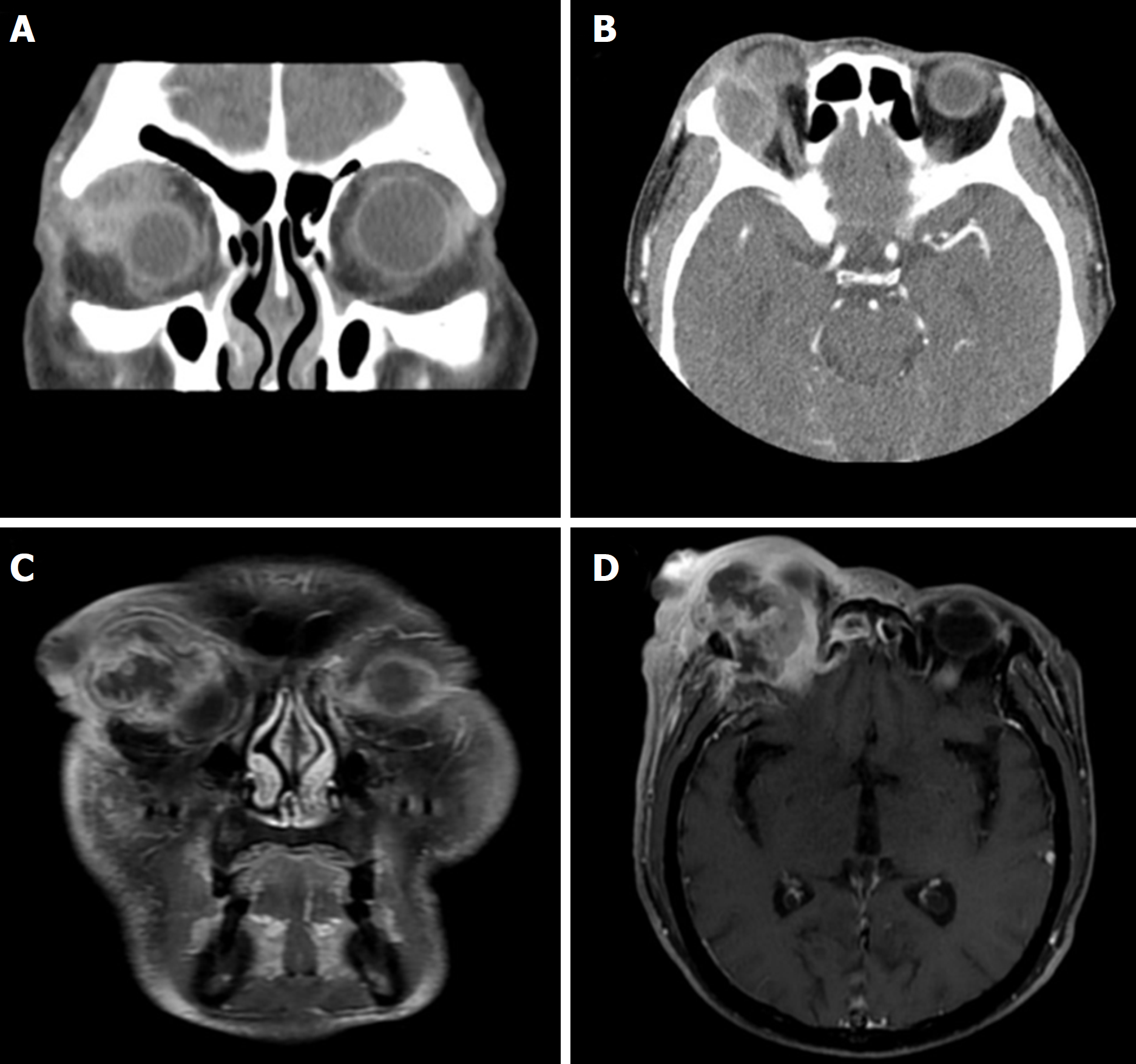
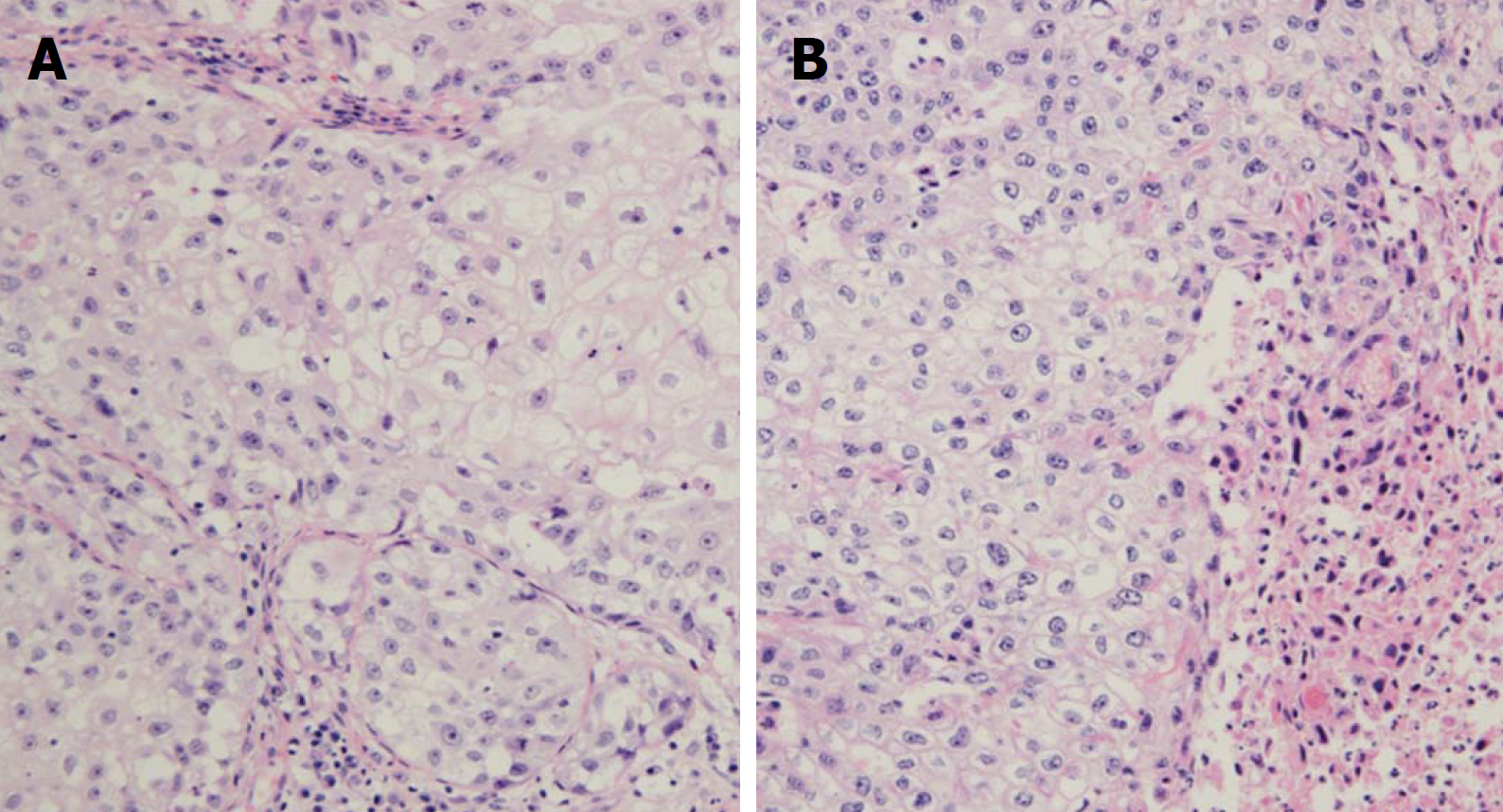
A 75-year-old man was referred with a 10-d history of painful swelling in the right eyelid. He had no medication or disease history. Upon examination, he had a palpable mass in the right superior orbit with tenderness. There were no abnormal findings other than hyperemia in the right eyelid and conjunctiva. At presentation, visual acuities were 6/12 for the right eye and 6/6 for the left eye. Intraocular pressure was in the normal range. Under the suspicion of dacryocystitis or preseptal cellulitis empiric antibiotics were prescribed, and computed tomography (CT) was performed. The CT scan demonstrated a 2.6 cm mass in the upper outer quadrant of the right orbit (Figure 1A and B). After incisional biopsy of the mass, the patient was diagnosed with squamous cell carcinoma of lacrimal gland (Figure 2A). The 18F-fludeoxyglucose positron emission tomography scan showed no distant metastases. We recommended surgery, but he refused treatment. After 3 mo, he presented with a greatly increased orbital mass. Magnetic resonance imaging (MRI) showed a 3.4 cm heterogeneously enhanced mass in the region of the lacrimal gland causing proptosis of the right eye (Figure 1C and D). This mass protruded into the skull base and was suspected to have invaded the dura, adjacent orbital roof and greater wing of the sphenoid bone.
The patient was diagnosed with primary tumor of lacrimal gland.
A right orbital exenteration, cervical lymph node dissection of ipsilateral level I-V and contralateral level I, and duroplasty were performed. There was no involvement of the overlying periorbital skin, eyelid, or conjunctiva. Histological examination of the exenteration specimen showed a 5.8 cm × 5.7 cm × 4.9 cm tumor arising from the lacrimal gland, which was entirely replaced by sebaceous carcinoma with sarcomatous and squamous differentiation (Figure 2B). Neoplastic cells were large and contained prominent nucleoli. Immunohistochemistry of the tissue was performed for human epithelial membrane antibody (EMA), cytokeratin, the androgen receptor, and anti-cytokeratin (CAM 5.2). Only EMA and CMA 5.2 showed positive staining. There was no perineural, lymphovascular space or lymph node involvement. The focal tumor remained in the posterior resection margin. The patient underwent adjuvant radiotherapy with a total dose of 56 Gy with dose-per-fraction 2 Gy to primary lesion. Elective neck irradiation was not performed.
There was no sign of recurrence during the 2-year follow-up period.
Tumors of lacrimal gland are relatively rare. It accounts for approximately 22%-28% of all orbital spaceoccupying lesions and 20%-50% of these tumors are malignant[7-9]. Epithelial tumors are the most common lesions of the lacrimal gland[8]. Epithelial lesions of the lacrimal gland include both benign and malignant tumors[10]. The most common benign tumor of the lacrimal gland is the pleomorphic adenoma, while the adenoid cystic carcinoma (ACC) is the most common malignant tumor[7,9,11]. Therefore, most studies on epithelial tumors of the lacrimal gland have been predominantly on ACC[12,13]. The subtypes of lacrimal gland carcinoma, other than ACC, are very rare and sebaceous carcinoma is one of the rarest tumor among them[12]. It has been studied only through several case series. Sebaceous carcinoma usually arises from the periorbital area, especially the eyelids, but primary SCLG is extremely rare[14]. Sebaceous carcinoma of the orbit is usually caused by orbital invasion of the periorbital carcinoma or by metastasis of tumors from other parts of the body. To establish a differential diagnosis, a systemic examination of the eyelids and conjunctiva is therefore essential.
Several hypotheses of pathogenesis of SCLG have been suggested. The first hypothesis is the possibility of malignant transformation and sebaceous differentiation of other epithelial tumors of the lacrimal gland[15]. Similarly, the tumor could likely arise from pluripotent cells that have differentiated into sebaceous cell[16]. Harvey et al[4] reported a patient with an eyelid tumor which grew slowly over the course of 8 years and grew rapidly afterwards. Histopathological examination showed malignant cells mixed with sarcomatous, adenocarcinomatous and pleomorphic sarcomatoid components. Cases support this hypothesis demonstrate relatively long duration of disease. Also, malignant cells have various differentiations and components similarly to our study. Second, some studies have suggested that SCLG may arise from heterotopic sebaceous cells in the lacrimal gland[15]. It has been reported that sebaceous glands have been observed in the orbital dermoid[4]. Evidence from tumors supporting this hypothesis consists of histopathological examination of homogenous cell lines and shows a relatively short duration of the disease.
SCLG shows similar clinical features and disease history to benign diseases such as chalazion, unilateral conjunctivitis and blepharitis, which often result in a long delay before the correct diagnosis is made[6,17]. The pathological growth pattern, which mimics that of squamous cell carcinoma or basal cell carcinoma, is another factor delaying the diagnosis[6]. Approximately 40%-75% of cases of SCLG have been misdiagnosed as squamous cell carcinoma, as in this study; therefore, histopathologically diagnosed squamous cell carcinoma cases should be considered for re-examination with lipid staining in order to reduce the error in initial diagnosis[6,17]. For the differential diagnosis, immunohistochemical studies using oil red-O stain, fat stain, EMA, cytokeratin, CAM 5.2, or BRST-1 are used[17]. SCLG is classified as a high grade tumor and potentially aggressive[8,9,14,18]. SCLG can metastasize into the preauricular and deep cervical lymph nodes early in the course of the disease[6]. The mortality rate has been estimated to be over 20%[6]. The delay in diagnosis, therefore, can increase the chance of local recurrence, metastasis, and death.
The optimal treatment of SCLG is difficult to study due to its rare incidence[12]. SCLG has so far been treated by surgical excision[3]. Because the local recurrence after surgical excision is approximately 9%-36%, postoperative radiotherapy is usually recommended[6]. For patients with difficulties in achieving a tumor-free margin or a cosmetically acceptable reconstruction, or when the patient refuses further surgical excision in the absence of orbital extension or distant metastasis, surgical excision with postoperative radiotherapy or radiotherapy alone could be an alternative treatment[6]. Currently, photon is widely used radiation, while particle radiation, using proton, carbon ion or neutron, is often used because of its physiological and biological advantages over photon. Compared with photon, particle radiation is characterized by high linear energy transfer and high relative biological effectiveness[3]. Moreover, particle radiation shows a maximum energy release in the focal site due to the formation of a Bragg peak[3]. As a result, radiation can be administered with superior tumor control and relative safety when the cancer is adjacent to an important organ[3]. Several institute use particle radiotherapy for improved tumor control and toxicities in the treatment of tumors of the lacrimal gland[3]. Yamamoto et al[3] reported promising treatment results of SCLG using carbon ion, one of the particle radiations. Some studies have reported similar results using carbon ion in tumors of the lacrimal gland with non-sebaceous histology[19]. It is not yet widely used due to treatment cost and accessibility, but particle radiation, including carbon ion, is expected to become widely used in the future. Another issue in radiotherapy of SCLG is target volume. As tumors could metastasize to preauricular and deep cervical lymph nodes early in the course of disease, parotidectomy and cervical lymphadenectomy could be considered[6,14]. Similarly, studies of optimal levels of elective neck irradiation are necessary. In the current study, we treated only primary lesions, considering lymph node dissection and pathology results. Until a consensus is reached, physicians should modify levels of neck irradiation according to physical examination and images.
We report a rare case of sebaceous carcinoma arising from the lacrimal gland initially diagnosed as squamous cell carcinoma. Although recent studies have reported a favorable prognosis, SCLG has high morbidity and mortality rates; therefore, accurate and early diagnosis is important[6]. Surgery is the main treatment, but radiotherapy could be applied postoperatively or as the only treatment. Further studies of radiotherapy target volume, including levels of neck irradiation and type of radiation used to treat SCLG, are needed. Primary sebaceous carcinoma can be diagnosed as benign or other malignancies. For appropriate treatment, accurate and early diagnosis is important. Due to its rarity, optimal treatment is not established. Further studies of treatment including radiotherapy are needed.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Cuevas-Covarrubias SAA, Kimyai-Asadi A, Vasconcellos C S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | von Holstein SL, Coupland SE, Briscoe D, Le Tourneau C, Heegaard S. Epithelial tumours of the lacrimal gland: a clinical, histopathological, surgical and oncological survey. Acta Ophthalmol. 2013;91:195-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 2. | Kiratli H, Tarlan B, Fırat P. Primary sebaceous carcinoma of the lacrimal gland. Orbit. 2012;31:352-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Yamamoto N, Mizoe JE, Hasegawa A, Ohshima K, Tsujii H. Primary sebaceous carcinoma of the lacrimal gland treated by carbon ion radiotherapy. Int J Clin Oncol. 2003;8:386-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Harvey PA, Parsons MA, Rennie IG. Primary sebaceous carcinoma of lacrimal gland: a previously unreported primary neoplasm. Eye (Lond). 1994;8:592-595. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Briscoe D, Mahmood S, Bonshek R, Jackson A, Leatherbarrow B. Primary sebaceous carcinoma of the lacrimal gland. Br J Ophthalmol. 2001;85:625-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Yoon JS, Kim SH, Lee CS, Lew H, Lee SY. Clinicopathological analysis of periocular sebaceous gland carcinoma. Ophthalmologica. 2007;221:331-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Snaathorst J, Sewnaik A, Paridaens D, de Krijger RR, van der Meij EH. Primary epithelial tumors of the lacrimal gland; a retrospective analysis of 22 patients. Int J Oral Maxillofac Surg. 2009;38:751-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | von Holstein SL, Rasmussen PK, Heegaard S. Tumors of the lacrimal gland. Semin Diagn Pathol. 2016;33:156-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Weis E, Rootman J, Joly TJ, Berean KW, Al-Katan HM, Pasternak S, Bonavolontà G, Strianese D, Saeed P, Feldman KA. Epithelial lacrimal gland tumors: pathologic classification and current understanding. Arch Ophthalmol. 2009;127:1016-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 97] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 10. | Chawla B, Kashyap S, Sen S, Bajaj MS, Pushker N, Gupta K, Chandra M, Ghose S. Clinicopathologic review of epithelial tumors of the lacrimal gland. Ophthalmic Plast Reconstr Surg. 2013;29:440-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 11. | Andreasen S, Esmaeli B, Holstein SL, Mikkelsen LH, Rasmussen PK, Heegaard S. An Update on Tumors of the Lacrimal Gland. Asia Pac J Ophthalmol (Phila). 2017;6:159-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Woo KI, Yeom A, Esmaeli B. Management of Lacrimal Gland Carcinoma: Lessons From the Literature in the Past 40 Years. Ophthalmic Plast Reconstr Surg. 2016;32:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 38] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Perez DE, Pires FR, Almeida OP, Kowalski LP. Epithelial lacrimal gland tumors: a clinicopathological study of 18 cases. Otolaryngol Head Neck Surg. 2006;134:321-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Dasgupta T, Wilson LD, Yu JB. A retrospective review of 1349 cases of sebaceous carcinoma. Cancer. 2009;115:158-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 223] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 15. | Shields JA, Shields CL, Epstein JA, Scartozzi R, Eagle RC Jr. Review: primary epithelial malignancies of the lacrimal gland: the 2003 Ramon L. Font lecture. Ophthalmic Plast Reconstr Surg. 2004;20:10-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 76] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Lima CG, Chahud F, Paiva CJ, Nebl D, Cruz AA. Primary adenocarcinoma of the lacrimal gland with sebaceous differentiation in a 4-year-old child. Ophthalmic Plast Reconstr Surg. 2014;30:e55-e57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Shields JA, Demirci H, Marr BP, Eagle RC Jr, Shields CL. Sebaceous carcinoma of the ocular region: a review. Surv Ophthalmol. 2005;50:103-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 225] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 18. | von Holstein SL, Therkildsen MH, Prause JU, Stenman G, Siersma VD, Heegaard S. Lacrimal gland lesions in Denmark between 1974 and 2007. Acta Ophthalmol. 2013;91:349-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 19. | Tsujii H, Kamada T. A review of update clinical results of carbon ion radiotherapy. Jpn J Clin Oncol. 2012;42:670-685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 214] [Article Influence: 16.5] [Reference Citation Analysis (0)] |