Published online Dec 26, 2018. doi: 10.12998/wjcc.v6.i16.1160
Peer-review started: September 30, 2018
First decision: October 12, 2018
Revised: October 15, 2018
Accepted: October 22, 2018
Article in press: October 22, 2018
Published online: December 26, 2018
Processing time: 85 Days and 13.4 Hours
We reported displacement of a ureteral double J stent into the vena cava and laparoscopic management in a 69-year-old patient with a history of ureteral stent placement. Preoperative computed tomography and plain X-rays showed malpositioning of the double J stent and displacement into the inferior vena cava. The characteristics of stent misplacement precluded endovascular procedures and explorative laparoscopic surgery was performed. The intra- and postoperative periods were uneventful. Postoperative imaging demonstrated that the new double J stent was in the right position. The patient was discharged 7 d after the operation and was symptom free at the 4-mo follow-up.
Core tip: Ureteral double J stent displacement into the vena cava is a rare complication in urology. Only six cases have been reported in the literature and all stents were removed by various methods that excluded laparoscopy. Here, we report our experience with a case that involved laparoscopy.
- Citation: Mao XW, Xu G, Xiao JQ, Wu HF. Ureteral double J stent displaced into vena cava and management with laparoscopy: A case report and review of the literature. World J Clin Cases 2018; 6(16): 1160-1163
- URL: https://www.wjgnet.com/2307-8960/full/v6/i16/1160.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i16.1160
Ureteral double J stents are usually used for maintaining urine flow from the kidney to the bladder, preventing stenosis, and surgery of ureteral injuries[1]. Traditionally, the procedure is performed under cystoscopic guidance with or without the aid of X-rays. Unavoidably, the double J stent will cause complications that include encrustation, fragmentation, distal and proximal migration, and lower urinary tract symptoms[2]. Most of them are mild and self-limited and can be alleviated by conservative interventions. However, the double J stent is rarely displaced into the vena cava through the ureter. Stent displacement can be managed by percutaneous removal, or open surgery combined with vascular surgery[3-8]. Here, we present a case of double J stent displacement into the vena cava and successful laparoscopic removal.
A 69-year-old patient with recurrent left flank pain and vomiting for 15 d was admitted to our hospital. He had a history of urinary stones and received extracorporeal shock wave lithotripsy for a left ureteral stone 8 and 3 years ago. Bilateral ureteral double J stents were placed due to anuria 1 d before the patient was referred to us. Postoperative X-rays demonstrated malpositioning of the left ureteral double J stent (Figure 1). Caval migration was highly suspected. Computed tomography (CT) showed that the left double J stent penetrated the bladder, then the left common iliac vein, and finally the inferior vena cava (IVC) (Figure 2). The upper end of the double J stent was at the level of the right renal vessels and not the heart, which made the case more complicated[8].
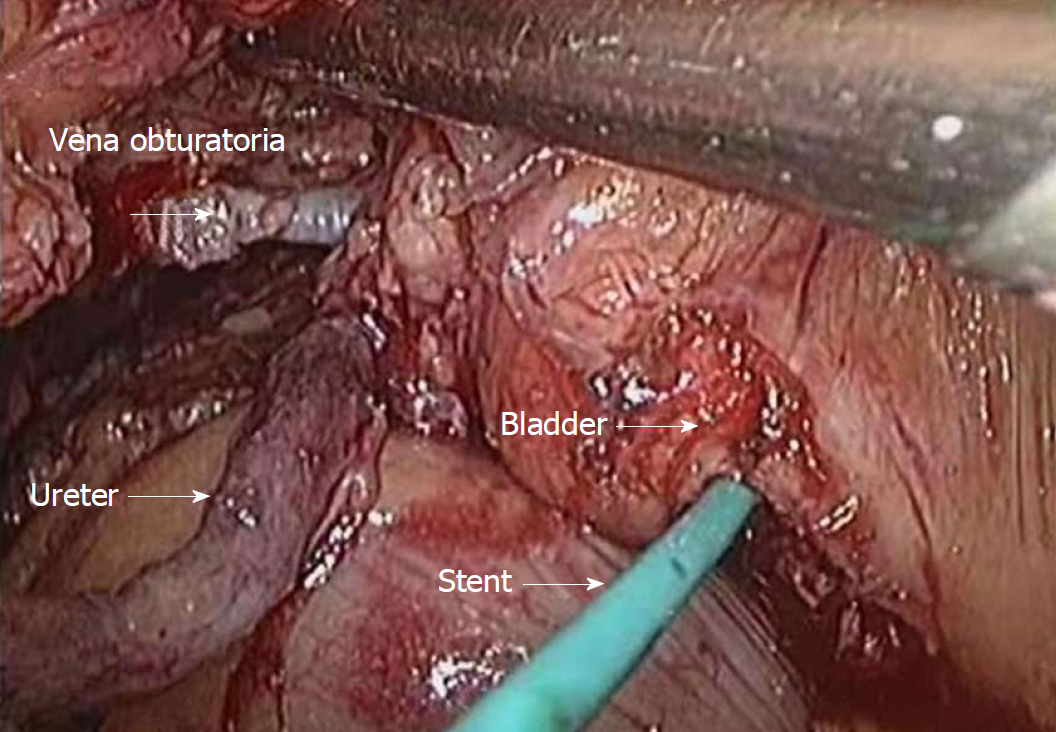
We planned to remove the migrated catheter laparoscopically based on the following factors. First, it was likely that the catheter had migrated into the vena cava from a small vessel, indicating that it would be feasible to perform the surgery laparoscopically. Second, the surgeon had performed a large number of laparoscopic operations and had experienced several similar cases, although not entirely the same. Our surgical plan was divided into four main steps: removing the catheter, repairing the vessel, repairing the ureter, and replacing the stent. Laparoscopic surgery was performed through three ports: optical access at a site 1 cm left of the umbilicus, 5 mm operative accesses on the lesion side, and one 10 mm access at the intersection of the umbilicus and anterior axillary line. After incising the peritoneum and reflecting the left colon, the ureter was identified. We noted by laparoscopic touch that the stent was not inside the ureter. Therefore, we opened the bladder and pulled the stent from the inside. A slight movement of one small vein near the bladder was observed. The vein, which proved to be the vena obturatoria, was thoroughly dissected and the stent was found inside the vein (Figure 3). The double J stent was removed from the vein from inside the bladder, and one Hem-o-lok clip was placed in the distal vein. Meanwhile, a minor ureteral injury was detected and repaired with 5/0 vicryl sutures. A new 6F double J stent was introduced into the ureter. The bladder was closed with 2/0 vicryl sutures. Finally, a small drain was inserted via the 5 mm port.
Postoperatively, the patient was started on anticoagulation therapy for 3 d and had an uneventful recovery. Postoperative X-rays confirmed that the new double J stent was in the right position. The patient was discharged 7 d after the operation. The new double J stent was removed cystoscopically 4 wk after surgery. The patient was followed for 3 mo and 1 year after surgery, and no sequelae were found with CT and ultrasound.
Ureteral stent placement, either antegrade or retrograde, is a prevalent intervention procedure. It causes various complications, including encrustation, fracture, and migration proximally and distally. Rare complications include stent knotting and vascular migration (Table 1)[3,6,7,9]. The presence of the stent within a ureter adjacent to a pulsating vascular structure, either a normal vessel or graft, appears to favor erosion[10]. Michalopoulos et al[4] first reported a case of intravascular migration of a stent placed intraoperatively in the right ureter that migrated into the venous circulation.
| First author | Year of publication | No. of patients | Clinical manifestation | Management | Upper end of stent | Primary disease |
| Michalopoulos et al[4] | 2002 | 1 | Pulmonary thromboembolism | Percutaneous removal through right femoral vein | IVC | Renal stone operation |
| Garrido et al[5] | 2008 | 1 | Loin pain and fever | Removal through percutaneous nephrostomy | IVC | Gynecologic surgery |
| Ioannou et al[6] | 2009 | 1 | Microscopic hematuria | Open surgery through left retroperitoneal approach | IVC | Obstructive pyelonephritis |
| Falahatkar et al[3] | 2012 | 1 | Urinary incontinence | Percutaneous removal through left femoral vein | Right atrium | Hysterectomy |
| Sabnis et al[7] | 2013 | 1 | History of ureteroscopy | Exploration through Gibson’s incision | Right atrium | Ureteral stone operation |
| Hastaoglu et al[8] | 2014 | 1 | Hematuria | Open surgery under cardiopulmonary bypass | Right ventricle | Ureteral stone operation |
In our patient, due to ureteral twisting or fragile bladder mucosa, the surgeon might have had difficulty placing the guidewire, which possibly penetrated directly out of the lower part of the ureter, and then into the adjacent vessel. If so, this would have caused gross hematuria and poor surgical vision. Subsequently, a ureteral stent was introduced through the guidewire and ultimately displaced into the IVC. It should be noted that the procedure has to be performed under X-ray monitoring, which may detect such a complication. Accordingly, it would be possible for the surgeon to correct it during the operation. However, it was unusual in our case that displacement into the circulation did not cause severe bleeding but rather moderate gross hematuria, so it appeared that the procedure was uneventful. The diagnosis of stent displacement can be established by postoperative plain abdominal radiography and CT imaging.
Endovascular management of arterioureteral fistula has been previously described[11-14]. It seems to be an ideal treatment in such a situation. Nevertheless, to make it clear, we decided to perform laparoscopic exploration since the lower end of the stent was still inside the bladder. Furthermore, the bladder should be explored to confirm its integrity. As stent migration did not cause severe bleeding, we believed that the operation could be attempted by laparoscopy. During the procedure, we observed that the stent went into the left common iliac vein through the vena obturatoria, which is a small vein. Undoubtedly, if the stent had penetrated directly into the adjacent major vein, open surgery would have been more feasible and safer.
In conclusion, the displacement of ureteral stents into the vascular system is a rare complication in urology. The key to prevention includes scopic guidance with X-ray monitoring, a high degree of suspicion, and early intervention. Treatment options include endovascular, percutaneous or open surgery, as well as laparoscopy.
A rare case of ureteral stent displacement into the vena cava.
After admission, kidney, ureter, bladder X-ray (KUB) combined with computed tomography (CT) scan confirmed that the left ureteral stent was in the inferior vena cava (IVC).
Theoretically, faulty ureteral stent positioning or placement outside of the ureter is not a rare complication. However, stent displacement into the IVC makes the case more complex and dangerous. CT scans can confirm the diagnosis.
The laboratory tests showed normal plasma levels of hemoglobin (115 g/L, normal range 110-150 g/L) and minor gross hematuria (RBC3+).
CT reconstruction combined with KUB showed the left ureteral stent in the IVC. The upper pole of the stent was at the kidney level and the lower pole was inside the bladder.
Pathological examination was not necessary in this case.
Based on previous experiences, we performed the operation laparoscopically and removed the stent successfully.
Ureteral stent displacement is defined as the stent not being in the right position but somewhere outside the ureter. Typically, the stent may only be placed in the nearby fat tissue and does not cause severe complications and sequelae.
The ureteral stent has to be placed under X-ray guidance. Displacement of the stent should be suspected when unusual or unexpected bleeding occurs after endoscopic surgery.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Desai DJ, Mazaris E S- Editor: Wang JL L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Brotherhood H, Lange D, Chew BH. Advances in ureteral stents. Transl Androl Urol. 2014;3:314-319. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Ahallal Y, Khallouk A, El Fassi MJ, Farih MH. Risk factor analysis and management of ureteral double-j stent complications. Rev Urol. 2010;12:e147-e151. [PubMed] |
| 3. | Falahatkar S, Hemmati H, Gholamjani Moghaddam K. Intracaval migration: an uncommon complication of ureteral Double-J stent placement. J Endourol. 2012;26:119-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Michalopoulos AS, Tzoufi MJ, Theodorakis G, Mentzelopoulos SD. Acute postoperative pulmonary thromboembolism as a result of intravascular migration of a pigtail ureteral stent. Anesth Analg. 2002;95:1185-1188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Garrido Abad P, Fernández Arjona M, Fernández González I, Santos Arrontes D, Pereira Sanz I. [Proximal migration of a Double J catheter: case report and review of the literature]. Arch Esp Urol. 2008;61:428-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Ioannou CV, Velegrakis J, Kostas T, Georgakarakos E, Touloupakis E, Anezinis P, Katsamouris AN. Caval migration of a ureteral J-stent after simultaneous ureter and iliac vein perforation during its placement for obstructive pyelonephritis. Int Angiol. 2009;28:421-424. [PubMed] |
| 7. | Sabnis RB, Ganpule AP, Ganpule SA. Migration of double J stent into the inferior vena cava and the right atrium. Indian J Urol. 2013;29:353-354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Hastaoglu IO, Tokoz H, Kavlak E, Bilgen F. Double J ureteral stent displaced through the right ventricle. Interact Cardiovasc Thorac Surg. 2014;18:853-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Sighinolfi MC, De Stefani S, Micali S, Mofferdin A, Baisi B, Celia A, Bianchi G. A knotted multi-length ureteral stent: a rare complication. Urol Res. 2005;33:70-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Bergqvist D, Pärsson H, Sherif A. Arterio-ureteral fistula--a systematic review. Eur J Vasc Endovasc Surg. 2001;22:191-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 117] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Asham EH, Walsh M, Adiseshiah M. An unusual case of haematuria treated by endoluminal repair. Eur J Vasc Endovasc Surg. 1999;17:89-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | el Khader K. [Complications of double J ureteral stents]. J Urol (Paris). 1996;102:173-175. [PubMed] |
| 13. | Gibbons M, O’Donnell S, Lukens M, Meglin A, Costabile RA. Treatment of a ureteroiliac artery fistula with an intraluminal endovascular graft. J Urol. 1998;159:2083-2084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Vandersteen DR, Saxon RR, Fuchs E, Keller FS, Taylor LM Jr, Barry JM. Diagnosis and management of ureteroiliac artery fistula: value of provocative arteriography followed by common iliac artery embolization and extraanatomic arterial bypass grafting. J Urol. 1997;158:754-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |