Published online Dec 26, 2018. doi: 10.12998/wjcc.v6.i16.1087
Peer-review started: September 25, 2018
First decision: October 11, 2018
Revised: October 23, 2018
Accepted: October 31, 2018
Article in press: November 1, 2018
Published online: December 26, 2018
Processing time: 91 Days and 17.1 Hours
Endoscopic retrograde cholangiopancreatography (ERCP) is one of the most frequently used image-guided procedures in gastrointestinal endoscopy. Post-ERCP pancreatitis is an important concern, and prophylaxis, cannulation and other related technical procedures have been well documented by endoscopists. In addition, medical radiation exposure is of great concern in the general population because of its rapidly increasing frequency and its potential carcinogenic effects. International organizations and radiological societies have established diagnostic reference levels, which guide proper radiation use and serve as global standards for all procedures that use ionizing radiation. However, data on gastrointestinal fluoroscopic procedures are still lacking because the demand for these procedures has recently increased. In this review, we present the current status of quality indicators for ERCP and the methods for measuring radiation exposure in the clinical setting as the next quality indicator for ERCP. To reduce radiation exposure, knowledge of its adverse effects and the procedures for proper measurement and protection are essential. Additionally, further studies on the factors that affect radiation exposure, exposure management and diagnostic reference levels are necessary. Then, we can discuss how to manage medical radiation use in these complex fluoroscopic procedures. This knowledge will help us to protect not only patients but also endoscopists and medical staff in the fluoroscopy unit.
Core tip: Endoscopic retrograde cholangiopancreatography (ERCP) is one of the most frequently performed image-guided procedures in gastrointestinal endoscopy. Among several quality measures of endoscopic procedures, including ERCP, radiation exposure is still not well documented. In the general population, medical radiation exposure is of great concern because of its rapid increase and potential carcinogenesis. International organizations have established diagnostic reference levels for proper use, which are now global standards. Therefore, radiation exposure represents the next quality indicator for ERCP. We must understand the adverse effects, the requirements for protection and other influencing factors. This knowledge will help us to protect patients, medical staff and endoscopists.
- Citation: Hayashi S, Takenaka M, Hosono M, Nishida T. Radiation exposure during image-guided endoscopic procedures: The next quality indicator for endoscopic retrograde cholangiopancreatography. World J Clin Cases 2018; 6(16): 1087-1093
- URL: https://www.wjgnet.com/2307-8960/full/v6/i16/1087.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i16.1087
Endoscopic retrograde cholangiopancreatography (ERCP) is one of the most frequently used image-guided procedures in gastrointestinal endoscopy. Post-ERCP pancreatitis (PEP) is a major concern, and prophylaxis, cannulation and other related technical procedures have been well documented by endoscopists. Thus, many studies and guidelines have been reported for ERCP. Recently, the quality of endoscopic procedures has been a key focus in gastrointestinal endoscopy with the aim of promoting the best procedures. Generally, quality indicators for endoscopic procedures are assessed at three time points: preprocedure, intraprocedure and postprocedure[1].
Radiation exposure during these procedures seems to be of less concern; such exposure is not well documented, and little data on this topic has been collected to date[2]. However, in the general population, medical radiation exposure is of great concern because of its rapidly increasing frequency and its potential carcinogenic effects, which can be evaluated based on the linear no-threshold model[3-6]. International organizations, such as the International Commission on Radiological Protection (ICRP), the International Atomic Energy Agency, and the United Nations Scientific Committee on the Effects of Atomic Radiation and radiological societies have attempted to keep medical radiation exposure as low as reasonably achievable (ALARA) by establishing diagnostic reference levels (DRLs)[7,8].
The concept of DRLs was first introduced by ICRP 73[9], and ICRP 103 and ICRP 105 emphasized the important role of DRLs as a tool for optimizing patient protection during diagnostic procedures[8,10]. ICRP 135 recommends that all individuals who are involved in subjecting a patient to a medical exposure should be familiar with the DRL process as a tool for optimizing protection[11]. Currently, the DRL is the global standard for all procedures that use ionizing radiation. The DRL guidelines have been updated in each region by each radiological society. However, there is still not enough data available on radiation exposure for gastrointestinal fluoroscopic procedures, such as ERCP, interventional endoscopic ultrasound, small bowel endoscopy, and enteral stent placement, which are still being developed and have recently been used with increasing in frequency.
In this review, we present the current status of quality indicators for ERCP, including the affiliated fluoroscopic procedures, especially in terms of medical radiation and DRLs. Then, we discuss how to approach radiation exposure management for this image-guided procedure, which is inherently complex[12].
ERCP is the major image-guided, high-risk procedure in gastrointestinal endoscopy, and its objective has changed from diagnostic to therapeutic purposes[13]. ERCP has various therapeutic applications, and although these applications are relatively less invasive than the previously employed surgical procedures, they are more invasive than the previous applications of ERCP[14]. Therefore, gastrointestinal societies have set guidelines for ERCP and tried to improve the quality of the procedure[1]. The American Society for Gastrointestinal Endoscopy (ASGE) refers to quality indicators in the following three categories: (1) indication, sedation and informed consent are preprocedure quality indicators; (2) cannulation, the procedure success rate, the radiation dose and fluoroscopy time are intraprocedure quality indicators; and (3) reporting and adverse events are postprocedure quality indicators[1]. Among these quality indicators, indication is one of the most important factors for avoiding unnecessary procedures. PEP is a major adverse event and can become life threatening[15-17]. Selective deep cannulation is an important component of successful ERCP and is also related to PEP[18]. There are, however, few statements about radiation exposure as a quality indicator.
Among the quality indicators for ERCP, the ASGE recommends that the fluoroscopy time and radiation dose be measured and emphasizes reducing patient exposure according to the ALARA principle, but no numerical levels are provided (Table 1). The European Society of Gastrointestinal Endoscopy (ESGE) provided specific numerical levels of radiation exposure for ERCP in its guidelines for radiation protection in digestive endoscopy in 2012; the recommended entrance skin dose (ESD) was 55-347 mGy, and the recommended kerma-area product (KAP) was 3-333 Gy.cm2 based on six previous reports that included a total of 608 procedures[19-25]. The ESGE, however, has also commented that the available information regarding DRLs for ERCP is limited[2].
| Society | Year | Procedure | Numerical number | Metric | Unit |
| ESGE[2] | 2012 | ERCP | 55-347 | ESD | mGy |
| 3-333 | KAP | Gy.cm2 | |||
| ASGE[1] | 2015 | ERCP | Not listed | Radiation dose | mGy |
| FT | |||||
| ASGE-DDW supplement[39] | 2018 | ERCP | Not listed | Dose RP | mGy |
| DAP | μGy.m2 | ||||
| Dose rate | mGy/min | ||||
| Japan DRLs[32] | 2015 | IVR | 20 | Dose rate | mGy/min |
| EC DRLs[30] | 2014 | ERCP | 30-45 | DAP | Gy.cm2 |
| UK NDRL[35] | 2016 | Biliary intervention | 43 | DAP | Gy.cm2 |
| 14 | FT | min | |||
| German DRL[31] | 2013 | ERCP | 2500 | DFP | μGy.m2 |
| ARPANSA DRL survey[62] | ongoing | ERCP/IVR | Not listed | Reference dose | Gy |
| DAP | Gy.cm2 | ||||
| Frame rate | fr/sec | ||||
| Total frames | number | ||||
| ACC/HRS/NASCI/SCAI/SCCT expert consensus[63] | 2018 | Cardiovascular intervention | Not listed | Air kerma | Gy |
| KAP, DAP | Gy.cm2 |
Presently, although endoscopists can use the available guidelines for ERCP to assess the procedural indication, the ordinal PEP rate, the perforation rate and the cannulation rate as quality indicators[1], most endoscopists cannot determine how much radiation exposure actually occurs during ERCP or determine the proper level of radiation exposure for a specific procedure. Thus, radiation exposure is an important quality indicator that requires further investigation due to the issues discussed in the following sections.
To understand medical radiation exposure, it is first necessary to understand the background and current status of medical radiation. Ionizing radiation has contributed to medical innovations since its discovery, including methods such as X-ray, fluoroscopy, computed tomography (CT), scintigraphy and radiotherapy, and the use of these procedures has recently increased due to increasing demand. On the other hand, we have recognized the adverse effects of medical radiation, which have been reported since approximately 2000.
The National Council of Radiation Protection and Measurements reported that the annual medical radiation exposure in the United States general population had increased from 15% in the early 1980s to 48% in 2006[26]. Similarly, the United Nations Scientific Committee on the Effects of Atomic Radiation reported that medical radiation is increasing with the progression of medical care worldwide, and the number of medical units is growing, as represented by CT and other diagnostic procedures[7]. Consequently, we are concerned about the adverse effects of radiation related to increasing medical radiation exposure.
The adverse effects of radiation are mainly divided into two types: deterministic risks and stochastic risks. The former category incorporates the threshold dose, as represented by skin injury[27]. The Food and Drug Administration stated that the typical threshold for the absorbed radiation dose is 2 Gy[28], and the ICRP recommends that the maximum cumulative absorbed dose for repeated procedures should be 1 Gy[29]. The latter risk category is related to the amount of total radiation exposure (linear no-threshold model), as represented by the cancer risk[6]. A total radiation exposure of 1 Sv is estimated to carry a 5% lifetime risk of cancer[12]. We should minimize both risks by understanding the threshold, the limit dose and the cumulative dose used for each patient.
To understand the radiation dose actually used and determine whether the dose is high in each procedure, we must set a reference level. This concept is precisely encompassed by DRLs, which serve as the current quality indicators for ERCP. The concept of DRLs was introduced by ICRP 73[9] in 1996, and concrete numerical levels were set by ICRP 103 in 2007[8]. Currently, DRLs are the global standards for all procedures that use ionizing radiation, and DRLs have been determined for almost all diagnostic procedures. Every procedure utilizing X-ray, CT or scintigraphy has been updated in each region[30-35].
Detailed DRLs have been established for therapeutic image-guided procedures, such as percutaneous coronary intervention and interventional radiology, but not for endoscopic procedures, including ERCP (Table 1). Generally, DRLs are set by the 75th percentile value and are determined from a large amount of radiation dose data for each procedure[11]. However, therapeutic interventions have objectives and outcomes that differ from those of diagnostic procedures.
Procedural variations, including variations in procedure time, fluoroscopy time and radiation dose, can result in a wide range of values[36], and a single DRL has not yet been established for ERCP because each DRL is designated for an individual CT location, such as the head, spine, chest or abdomen. Therefore, a sufficient amount of data and an applicable, simple classification scheme are necessary to set the DRL for ERCP.
An applicable classification scheme for the wide range of established DRLs seems to be necessary. In German DRLs, the angio-therapy classification divides aneurism treatment into three locations: the thoracic artery, the infrarenal artery and the suprarenal abdominal aorta. Similarly, percutaneous transluminal angioplasties are divided into three locations: the pelvis, the thigh with the knee and the lower leg with the foot[31]. Hence, simply dividing the procedure into three or four classifications may be preferable for ERCP[37]. We also previously reported a simple classification based on disease site (common bile duct stones, proximal malignant biliary obstruction, distal malignant biliary obstruction and other). Consequently, different classifications result in clearly divided outcomes and may be helpful for accurately determining DRLs[36].
Image-guided procedures such as ERCP present another problem in determining DRLs. ERCP inherently requires fluoroscopy and characteristically includes both standard radiography and cineradiography, which utilizes rapidly changing levels of radiation exposure. The moment-to-moment dynamic outcomes are generally explained by the following four fundamental factors: (1) magnification; (2) frame rate; (3) focus area and (4) moving field of view. These four factors automatically change the output from moment to moment. The flexibility of fluoroscopy makes it difficult to predict the final exposure level from the initial settings, in contrast to roentgenography or CT. Consequently, there are many difficulties in this field, and the ICRP has characterized image-guided procedures by their complexity[12]. We must be aware of the inherent nature of ERCP when evaluating the data and establishing appropriate DRLs.
Dose metrics and units for radiation exposure in medical imaging modalities such as radiography, CT and fluoroscopy have been systematically defined by international organizations[11,38] and are used globally in the management of patient radiation doses. Among these metrics, those used in fluoroscopy are more diverse because of the wide variety of clinical applications; in addition, dose metrics and units have not been clearly specified for some fluoroscopic procedures. Consequently, various DRLs and guidelines use varying dose metrics and units, which results in confusion for endoscopists (Table 1). Moreover, there are many definitions of the relevant measures, which present difficulty for endoscopists who are not familiar with these definitions.
The ESGE refers to ESD in mGy and KAP in Gy.cm2, while the ASGE refers only to radiation dose and fluoroscopy time without providing numerical levels[1,2]. Faigel[39] and his colleagues[40] reported fluoroscopy time, dose-area product (DAP) in μGy.m2 and dose reference point (dose RP) in mGy. Among the radiological societies, only the European Commission reported the radiation dose of ERCP as DAP in Gy.cm2[30], and the German DRL was provided as the Dosis-flächen-produkt (DFP, or dose-area product) in μGy.m2[31]. In the field of interventional radiology, the Japanese DRL provides the dose rate in mGy/min[32], the UK National DRL is presented as the DAP in Gy.cm2 and the American College of Cardiology expert consensus uses air kerma in Gy and DAP with KAP in Gy.cm2[41]. Therefore, establishing a uniform measurement among the medical societies might be the first step in establishing DRLs, which represent the next quality indicators for ERCP.
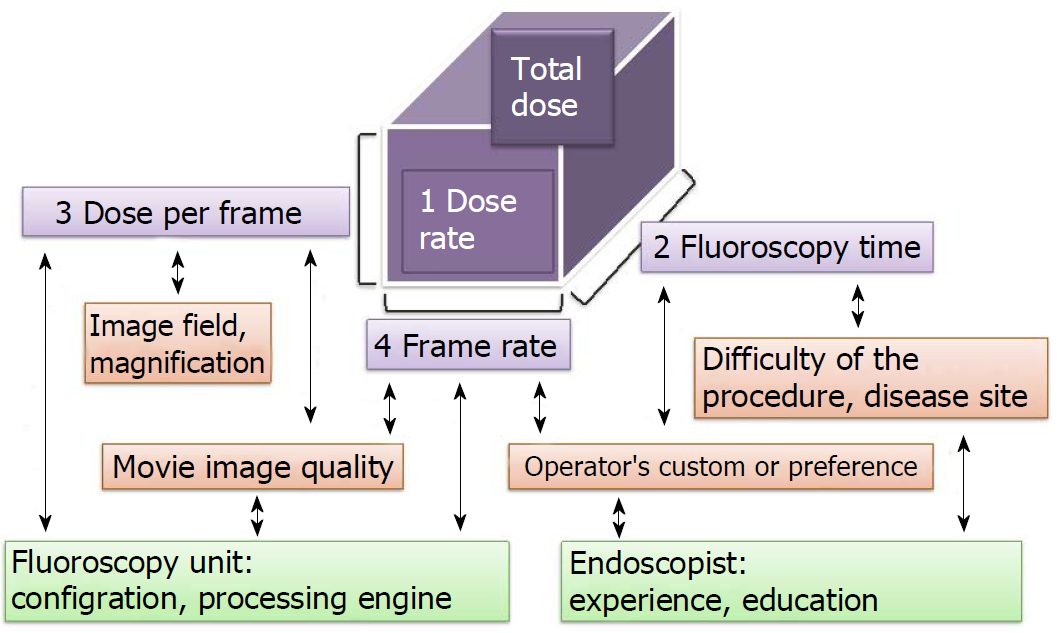
The total radiation dose (ESD, air kerma or dose RP) is approximated by the integrated value of fluoroscopy time, dose per frame and frame rate, as shown in Figure 1. Several factors affecting the radiation dose during image-guided procedures have been reported. For example, high-volume endoscopists can achieve lower radiation exposure[42-45]. In addition, brief educational program for endoscopists or a flashing warning light in the fluoroscopy unit can be effective for reducing radiation exposure[46,47] because fluoroscopy time is related to radiation exposure[40,48]. With regard to the fluoroscopy unit, pulsation, static fluoroscopy, C-arm, low pulse rate and the distance between the monitor and the endoscope can help to reduce the total radiation dose[19,49-54].
Recently, some image-enhancing technologies, centre volume and local DRL guidelines have also been shown to influence the total radiation dose delivered to patients[36,55-58]. The simplest and most effective ways to reduce the total radiation dose are: (1) using a low frame rate; (2) using low magnification and (3) employing a short fluoroscopy time. A lower frame rate can reduce the dose per second, which impairs the image quality, resulting in a jumpy image or an afterimage. Similarly, lower magnification reduces the dose per frame but also results in lower spatial resolution. These two factors must be considered according to the ALARA principle. A better processing engine, such as a graphics processing unit, can help this problem. Finally, fluoroscopy time is strongly associated with the procedure time and the difficulty of the procedure[59,60]. Fluoroscopy time is often managed by the operators according to their preferences, but communicating the need for caution or providing education to operators can improve the fluoroscopy time and radiation exposure[46,47,61].
We need to set DRLs for all fluoroscopic procedures in the gastrointestinal field, including ERCP, interventional endoscopic ultrasound, balloon-assisted enteroscopy, enteral stenting and ileus tubing. Consequently, endoscopists will know how much radiation to use and whether the delivered radiation level is higher or lower than the reference level. Then, we will be able to discuss how to manage medical radiation in fluoroscopic procedures. Developing DRLs will help us to protect not only patients but also medical staff and endoscopists in the fluoroscopy unit.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Dhaliwal HS, Kitamura K, Neri V S- Editor: Dou Y L- Editor: Filipodia E- Editor: Wu YXJ
| 1. | Adler DG, Lieb JG 2nd, Cohen J, Pike IM, Park WG, Rizk MK, Sawhney MS, Scheiman JM, Shaheen NJ, Sherman S, Wani S. Quality indicators for ERCP. Gastrointest Endosc. 2015;81:54-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 145] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 2. | Dumonceau JM, Garcia-Fernandez FJ, Verdun FR, Carinou E, Donadille L, Damilakis J, Mouzas I, Paraskeva K, Ruiz-Lopez N, Struelens L. Radiation protection in digestive endoscopy: European Society of Digestive Endoscopy (ESGE) guideline. Endoscopy. 2012;44:408-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 86] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 3. | Berrington de González A, Darby S. Risk of cancer from diagnostic X-rays: estimates for the UK and 14 other countries. Lancet. 2004;363:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1191] [Cited by in RCA: 1078] [Article Influence: 51.3] [Reference Citation Analysis (0)] |
| 4. | Jaffe D, Bowden GT. Ionizing radiation as an initiator: effects of proliferation and promotion time on tumor incidence in mice. Cancer Res. 1987;47:6692-6696. [PubMed] |
| 5. | Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, Giles GG, Wallace AB, Anderson PR, Guiver TA. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1349] [Cited by in RCA: 1391] [Article Influence: 115.9] [Reference Citation Analysis (0)] |
| 6. | Shore RE, Beck HL, Boice JD, Caffrey EA, Davis S, Grogan HA, Mettler FA, Preston RJ, Till JE, Wakeford R. Implications of recent epidemiologic studies for the linear nonthreshold model and radiation protection. J Radiol Prot. 2018;38:1217-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 7. | United Nations Scientific Committee on the Effects of Atomic Radiation. Sources and effects of ionizing radiation. 2008; Available from: http://www.unscear.org/unscear/publications/2008_1.html. |
| 8. | The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37:1-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 1070] [Article Influence: 62.9] [Reference Citation Analysis (0)] |
| 9. | Radiological protection and safety in medicine. A report of the International Commission on Radiological Protection. Ann ICRP. 1996;26:1-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 215] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 10. | ICRP Publication 105. Radiation protection in medicine. Ann ICRP. 2007;37:1-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Vañó E, Miller DL, Martin CJ, Rehani MM, Kang K, Rosenstein M, Ortiz-López P, Mattsson S, Padovani R, Rogers A; Authors on behalf of ICRP. ICRP Publication 135: Diagnostic Reference Levels in Medical Imaging. Ann ICRP. 2017;46:1-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 291] [Cited by in RCA: 507] [Article Influence: 72.4] [Reference Citation Analysis (0)] |
| 13. | Carr-Locke DL. Overview of the role of ERCP in the management of diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2002;56:S157-S160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Huang RJ, Thosani NC, Barakat MT, Choudhary A, Mithal A, Singh G, Sethi S, Banerjee S. Evolution in the utilization of biliary interventions in the United States: results of a nationwide longitudinal study from 1998 to 2013. Gastrointest Endosc. 2017;86:319-326.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 15. | Dumonceau JM, Andriulli A, Elmunzer BJ, Mariani A, Meister T, Deviere J, Marek T, Baron TH, Hassan C, Testoni PA. Prophylaxis of post-ERCP pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - updated June 2014. Endoscopy. 2014;46:799-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 378] [Cited by in RCA: 398] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 16. | ASGE Standards of Practice Committee, Chandrasekhara V, Khashab MA, Muthusamy VR, Acosta RD, Agrawal D, Bruining DH, Eloubeidi MA, Fanelli RD, Faulx AL, Gurudu SR, Kothari S, Lightdale JR, Qumseya BJ, Shaukat A, Wang A, Wani SB, Yang J, DeWitt JM. Adverse events associated with ERCP. Gastrointest Endosc. 2017;85:32-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 405] [Cited by in RCA: 533] [Article Influence: 66.6] [Reference Citation Analysis (0)] |
| 17. | Hayashi S, Nishida T, Shimakoshi H, Shimoda A, Amano T, Sugimoto A, Takahashi K, Mukai K, Matsubara T, Yamamoto M. Combination of two-hour post-endoscopic retrograde cholangiopancreatography amylase levels and cannulation times is useful for predicting post-endoscopic retrograde cholangiopancreatography pancreatitis. World J Gastrointest Endosc. 2016;8:777-784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Testoni PA, Mariani A, Aabakken L, Arvanitakis M, Bories E, Costamagna G, Devière J, Dinis-Ribeiro M, Dumonceau JM, Giovannini M. Papillary cannulation and sphincterotomy techniques at ERCP: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy. 2016;48:657-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 290] [Cited by in RCA: 383] [Article Influence: 42.6] [Reference Citation Analysis (1)] |
| 19. | Staniszewska MA, Kujawski K, Kopeć R, Sasak K. ERCP procedures as a source of radiation risk to a single gastroenterologist. Med Pr. 2017;68:735-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Olgar T, Bor D, Berkmen G, Yazar T. Patient and staff doses for some complex x-ray examinations. J Radiol Prot. 2009;29:393-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Brambilla M, Marano G, Dominietto M, Cotroneo AR, Carriero A. Patient radiation doses and references levels in interventional radiology. Radiol Med. 2004;107:408-418. [PubMed] |
| 22. | Tsalafoutas IA, Paraskeva KD, Yakoumakis EN, Vassilaki AE, Maniatis PN, Karagiannis JA, Koulentianos ED. Radiation doses to patients from endoscopic retrograde cholangiopancreatography examinations and image quality considerations. Radiat Prot Dosimetry. 2003;106:241-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Larkin CJ, Workman A, Wright RE, Tham TC. Radiation doses to patients during ERCP. Gastrointest Endosc. 2001;53:161-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 89] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 24. | Heyd RL, Kopecky KK, Sherman S, Lehman GA, Stockberger SM. Radiation exposure to patients and personnel during interventional ERCP at a teaching institution. Gastrointest Endosc. 1996;44:287-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 54] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Chen MY, Van Swearingen FL, Mitchell R, Ott DJ. Radiation exposure during ERCP: effect of a protective shield. Gastrointest Endosc. 1996;43:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 26. | Schauer DA, Linton OW. NCRP Report No. 160, Ionizing Radiation Exposure of the Population of the United States, medical exposure--are we doing less with more, and is there a role for health physicists? Health Phys. 2009;97:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 265] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 27. | Henry MF, Maender JL, Shen Y, Tschen JA, Subrt P, Schmidt JD, Hsu S. Fluoroscopy-induced chronic radiation dermatitis: a report of three cases. Dermatol Online J. 2009;15:3. [PubMed] |
| 28. | Avoidance of serious x-ray-induced skin injuries to patients during fluoroscopically-guided procedures. United Stated Food and Drug Administration 1994;. Available from: http://www.fda.gov/cdrh/sep9_94.pdf. |
| 29. | Valentin J. Avoidance of radiation injuries from medical interventional procedures. Ann ICRP. 2000;30:7-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 297] [Cited by in RCA: 336] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 30. | European Commission. Diagnostic Reference Levels in Thirty-six European Countries. 2014; Available from: https://ec.europa.eu/energy/sites/ener/files/documents/RP180%20part2.pdf. |
| 31. | Bundesamt fur Strahlenschutz. Bekanntmachung der aktualisierten diagnostischen Referenzwerte für diagnostische und interventionelle Röntgenanwendungen. 2016;22 Available from: https://www.bfs.de/DE/themen/ion/anwendung-medizin/diagnostik/referenzwerte/bekanntmachung-referenzwerte.html. |
| 32. | Watanabe H, Ishii K, Hosono M, Imabayashi E, Abe K, Inubushi M, Ohno K, Magata Y, Ono K, Kikuchi K. Report of a nationwide survey on actual administered radioactivities of radiopharmaceuticals for diagnostic reference levels in Japan. Ann Nucl Med. 2016;30:435-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Roch P, Aubert B. French diagnostic reference levels in diagnostic radiology, computed tomography and nuclear medicine: 2004-2008 review. Radiat Prot Dosimetry. 2013;154:52-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 62] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 34. | Blanco S, Mora P, Almonte N, Benavente T, Benson N, Blanco D, Cárdenas J, Defaz Gómez Y, Edding O, Escobar C. Determination of diagnostic reference levels in general radiography in Latin America. Radiat Prot Dosimetry. 2013;156:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 35. | National-DRLs. National diagnostic reference levels (NDRLs) - GOV UK 2016. Available from: https://www.gov.uk/government/publications/diagnostic-radiology-national-diagnostic-reference-levels-ndrls/national-diagnostic-reference-levels-ndrls. |
| 36. | Hayashi S, Higaki Y, Tomita R, Shimakoshi H, Shimoda A, Osugi N, Sugimoto A, Takahashi K, Mukai K, Nakamatsu D. 940 Disease Site and Processing Engine Affect Radiation Exposure Dose during Ercp. Gastrointestinal endoscopy. 2018;AB137. [DOI] [Full Text] |
| 37. | Choi MH, Jung SE, Yoon SB, Lee IS, Byun JY. Location of Disease on Imaging may Predict Radiation Exposure During Endoscopic Retrograde Cholangiopancreatography. Radiat Prot Dosimetry. 2017;177:280-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 38. | Patient dosimetry for x rays used in medical imaging. J ICRU. 2005;5:iv-vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 39. | Faigel D. ASGE Program. Gastrointest Endosc. 2018;87:AB1-AB45. [DOI] [Full Text] |
| 40. | Kachaamy T, Harrison E, Pannala R, Pavlicek W, Crowell MD, Faigel DO. Measures of patient radiation exposure during endoscopic retrograde cholangiography: beyond fluoroscopy time. World J Gastroenterol. 2015;21:1900-1906. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 41. | Hirshfeld JW Jr, Ferrari VA, Bengel FM, Bergersen L, Chambers CE, Einstein AJ, Eisenberg MJ, Fogel MA, Gerber TC, Haines DE, Laskey WK, Limacher MC, Nichols KJ, Pryma DA, Raff GL, Rubin GD, Smith D, Stillman AE, Thomas SA, Tsai TT, Wagner LK, Wann LS. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in Cardiovascular Imaging: Best Practices for Safety and Effectiveness: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;71:e283-e351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 88] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 42. | Uradomo LT, Lustberg ME, Darwin PE. Effect of physician training on fluoroscopy time during ERCP. Dig Dis Sci. 2006;51:909-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 43. | Gonzalez-Gonzalez JA, Martínez-Vazquez MA, Maldonado-Garza HJ, Garza-Galindo AA. Radiation doses to ERCP patients are significantly lower with experienced endoscopists. Gastrointest Endosc. 2011;73:415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 44. | Liao C, Thosani N, Kothari S, Friedland S, Chen A, Banerjee S. Radiation exposure to patients during ERCP is significantly higher with low-volume endoscopists. Gastrointest Endosc. 2015;81:391-8.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 45. | Jorgensen JE, Rubenstein JH, Goodsitt MM, Elta GH. Radiation doses to ERCP patients are significantly lower with experienced endoscopists. Gastrointest Endosc. 2010;72:58-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 46. | Barakat MT, Thosani NC, Huang RJ, Choudhary A, Kochar R, Kothari S, Banerjee S. Effects of a Brief Educational Program on Optimization of Fluoroscopy to Minimize Radiation Exposure During Endoscopic Retrograde Cholangiopancreatography. Clin Gastroenterol Hepatol. 2018;16:550-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 47. | Zeng HZ, Liu Q, Chen HL, Liu W, Zeng QS, Wu CC, Hu B. A pilot single-center prospective randomized trial to assess the short-term effect of a flashing warning light on reducing fluoroscopy time and radiation exposure during ERCP. Gastrointest Endosc. 2018;88:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 48. | Boix J, Lorenzo-Zúñiga V. Radiation dose to patients during endoscopic retrograde cholangiopancreatography. World J Gastrointest Endosc. 2011;3:140-144. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 37] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 49. | Martin CJ. A review of factors affecting patient doses for barium enemas and meals. Br J Radiol. 2004;77:864-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 50. | Churrango G, Deutsch JK, Dinneen HS, Churrango J, Samiullah S, Ahlawat SK. Minimizing Radiation Exposure During ERCP by Avoiding Live or Continuous Fluoroscopy. J Clin Gastroenterol. 2015;49:e96-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 51. | Hansen JW, Foy A, Schmidt T, Ghahramani M, Chambers CE. Fluoroscopy pulse rate reduction during diagnostic and therapeutic imaging in the cardiac catheterization laboratory: An evaluation of radiation dose, procedure complications and outcomes. Catheter Cardiovasc Interv. 2017;89:665-670. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 52. | Abdelaal E, Plourde G, MacHaalany J, Arsenault J, Rimac G, Déry JP, Barbeau G, Larose E, De Larochellière R, Nguyen CM. Effectiveness of low rate fluoroscopy at reducing operator and patient radiation dose during transradial coronary angiography and interventions. JACC Cardiovasc Interv. 2014;7:567-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 83] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 53. | Jowhari F, Hopman WM, Hookey L. A simple ergonomic measure reduces fluoroscopy time during ERCP: A multivariate analysis. Endosc Int Open. 2017;5:E172-E178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 54. | Boland GW, Murphy B, Arellano R, Niklason L, Mueller PR. Dose reduction in gastrointestinal and genitourinary fluoroscopy: use of grid-controlled pulsed fluoroscopy. AJR Am J Roentgenol. 2000;175:1453-1457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 55. | Huo Y, Christoph M, Forkmann M, Pohl M, Mayer J, Salmas J, Sitzy J, Wunderlich C, Piorkowski C, Gaspar T. Reduction of radiation exposure during atrial fibrillation ablation using a novel fluoroscopy image integrated 3-dimensional electroanatomic mapping system: A prospective, randomized, single-blind, and controlled study. Heart Rhythm. 2015;12:1945-1955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 56. | Hoffmann R, Langenbrink L, Reimann D, Kastrati M, Becker M, Piatkowski M, Michaelsen J. Image noise reduction technology allows significant reduction of radiation dosage in cardiac device implantation procedures. Pacing Clin Electrophysiol. 2017;40:1374-1379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 57. | Hayashi S, Nishida T, Shimakoshi H, Shimoda A, Amano T, Sugimoto A, Takahashi K, Mukai K, Matsubara T, Yamamoto M. Mo2020 Novel Processing Engine for X-Ray Fluoroscopic Images (Faice-V Ns1) Can Reduce Radiation Exposure in the Procedure of ERCP But Keep the Quality of Images. Gastrointestinal endoscopy. 2017;AB524. [DOI] [Full Text] |
| 58. | Saukko E, Henner A, Nieminen MT, Ahonen SM. The establishment of local diagnostic reference levels in endoscopic retrograde cholangiopancreatography: a practical tool for the optimisation and for quality assurance management. Radiat Prot Dosimetry. 2017;173:338-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 59. | Seo D, Kim KH, Kim JS, Han S, Park K, Kim J. Evaluation of radiation doses in patient and medical staff during endoscopic retrograde cholangiopancreatography procedures. Radiat Prot Dosimetry. 2016;168:516-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 60. | Alkhatib AA, Jalil AA, Harrison ME. ERCP and fluoroscopy time. Am J Gastroenterol. 2014;109:447-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 61. | Wong CS, Huang B, Sin HK, Wong WL, Yiu KL, Chu Yiu Ching T. A questionnaire study assessing local physicians, radiologists and interns’ knowledge and practice pertaining to radiation exposure related to radiological imaging. Eur J Radiol. 2012;81:e264-e268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 62. | Image guided interventional procedures survey. ARPANSA. Available from: https://www.arpansa.gov.au/research-and-expertise/surveys/national-diagnostic-reference-level-service/igip/igip-survey. |
| 63. | Hirshfeld JW Jr, Ferrari VA, Bengel FM, Bergersen L, Chambers CE, Einstein AJ, Eisenberg MJ, Fogel MA, Gerber TC, Haines DE, Laskey WK, Limacher MC, Nichols KJ, Pryma DA, Raff GL, Rubin GD, Smith D, Stillman AE, Thomas SA, Tsai TT, Wagner LK, Wann LS. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in Cardiovascular Imaging-Best Practices for Safety and Effectiveness, Part 1: Radiation Physics and Radiation Biology: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol. 2018;71:2811-2828. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |