Published online Dec 6, 2018. doi: 10.12998/wjcc.v6.i15.936
Peer-review started: September 27, 2018
First decision: October 18, 2018
Revised: October 25, 2018
Accepted: November 7, 2018
Article in press: November 7, 2018
Published online: December 6, 2018
Processing time: 70 Days and 10.3 Hours
To compare the effect and postoperative trauma of ultrasound-guided percutaneous microwave ablation and surgical resection in the treatment of papillary thyroid microcarcinoma (PTMC).
Eighty-seven patients with PTMC treated at Fudan University affiliated Shanghai Fifth People’s Hospital were enrolled as subjects. The patients were divided into a microwave ablation group (41 cases) and a surgical group (46 cases). The operative time, intraoperative blood loss, length of hospital stay, serum C-reactive protein (CRP), interleukin-6 (IL-6), tumor necrosis factor-α (TNF-α), thyroid-related hormonal changes, and complications 7 d and 30 d after surgery were observed.
The operative time, intraoperative blood loss, and length of hospital stay in the surgical group were significantly higher than those in the microwave ablation group (P < 0.05). The levels of CRP, IL-6, and TNF-α in the surgical group were significantly higher than those in the microwave ablation group (P < 0.05). The free triiodothyronine (FT3) and free thyroxin (FT4) levels in the surgical group were significantly lower than those in the microwave ablation group (P < 0.05). However, the postoperative thyroid stimulating hormone (TSH) level was significantly higher than that in the microwave ablation group (P < 0.05). There were significant interactions between the FT3, FT4, and TSH 7 d and 30 d after operation and the treatment methods (P < 0.05). There was no significant difference in the complications between the two groups (P > 0.05).
Microwave ablation for papillary microcarcinoma of the thyroid gland has less trauma to the body, quicker recovery, and no scars. It can effectively shorten the length of hospital stay and improve the quality of life of patients.
Core tip: Although thyroidectomy is the standard treatment for papillary thyroid microcarcinoma (PTMC), it causes great trauma to the patient’s body. In recent years, there have been reports on microwave ablation for patients with PTMC, but the efficacy is not certain. This study aimed to compare the efficacy and the impact on body trauma using ultrasound-guided percutaneous microwave ablation for PTMC and surgical resection. The results showed that microwave ablation for PTMC has less trauma, quicker recovery, and no scars, which can effectively shorten the hospitalization time and improve the quality of life.
- Citation: Xu B, Zhou NM, Cao WT, Gu SY. Comparative study on operative trauma between microwave ablation and surgical treatment for papillary thyroid microcarcinoma. World J Clin Cases 2018; 6(15): 936-943
- URL: https://www.wjgnet.com/2307-8960/full/v6/i15/936.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i15.936
With the popularization of thyroid ultrasonography and the wide application of ultrasound-guided fine needle aspiration, the detection rate of papillary thyroid microcarcinoma (PTMC) is increasing over time[1,2]. At present, thyroidectomy is still the standard treatment method. However, the patient’s physical and psychological trauma caused by surgery is extremely high. Hemorrhage during the operation may easily damage the adjacent vital structures such as the parathyroid gland and the recurrent laryngeal nerve, causing complications such as hoarseness after surgery and leading to greater damage to the patient[3-5]. With the rapid development of minimal invasive techniques, ultrasound-guided microwave ablation has the advantages of small injury, short treatment time, effective curative effect, little effect on the surrounding structure and patient appearance, rapid recovery after ablation, no need for lifelong medication, etc. However, it is mainly used for treatment of thyroid benign nodules[6-8]. In recent years, microwave ablation has also been reported for some patients with PTMC and achieved good results[9-11]. However, the current clinical value of ultrasound-guided microwave ablation for PTMC has not yet reached a consensus and it cannot accurately judge whether this new treatment can replace traditional surgery. Therefore, the present study aimed to compare the impact of ultrasound-guided percutaneous microwave ablation of PTMC vs surgical resection on body trauma.
Totally 87 patients with PTMC diagnosed by ultrasound guided fine-needle aspiration biopsy (FNAB) at Fudan University Affiliated Shanghai Fifth People’s Hospital from January 2012 to October 2017 were included. The maximum diameter of nodules was less than 1.0 cm. Microwave ablation or surgery was selected based on the patient’s own condition and their wishes. The microwave ablation group consisted of 41 patients including 12 males and 29 females and aged from 24 to 65 years with an average age of 45.11 ± 7.28 years (Table 1). The inclusion criteria were: (1) Papillary microcarcinoma of the thyroid gland confirmed by FNAB; (2) Maximum tumor diameter ≤ 1.0 cm, not close to the capsule (distance > 2.0 mm), no obvious abnormality of the contralateral thyroid gland, and no large neck lymphadenopathy or metastatic lymph nodes; and (3) Ultrasound imaging had a clear needle path. Patients with severe heart or lung diseases or poor general condition which cannot tolerate surgery or those who rejected the surgery or were anxious about the disease for treatment were excluded.
| Group | Case | Age (yr) | Gender | Maximum diameter of nodule (mm) | |
| Male | Female | ||||
| Surgery group | 46 | 46.2 ± 11.5 | 16 | 30 | 8.13 ± 1.22 |
| Microwave | 41 | 45.8 ± 10.2 | 12 | 29 | 8.87 ± 1.01 |
| Ablation group | |||||
| t/χ2-value | 0.171 | 0.302 | -3.061 | ||
| P-value | 0.865 | 0.583 | 0.003 | ||
The GE Voluson E8 ultrasound diagnostic device with a line array probe (frequency from 5 to 10 MHz) was used. Microwave ablation was performed using Nanjing Kangyou KY-2000 microwave ablation instrument and the frequency was 2450 MHz with continuous adjustable output power from 10 to 100 W. Microwave ablation instrument is connected with a 16 G cold-cycle Thy-ablation microwave antenna through a low loss coaxial cable.
Surgery group: A 5 cm long transverse incision was made 2 cm above the sternal fossa. Radical resection of the PTMC (the affected side of the thyroid and isthmus resection + lymph node dissection of the affected side VI) was adopted. Negative pressure drainage was performed after surgery.
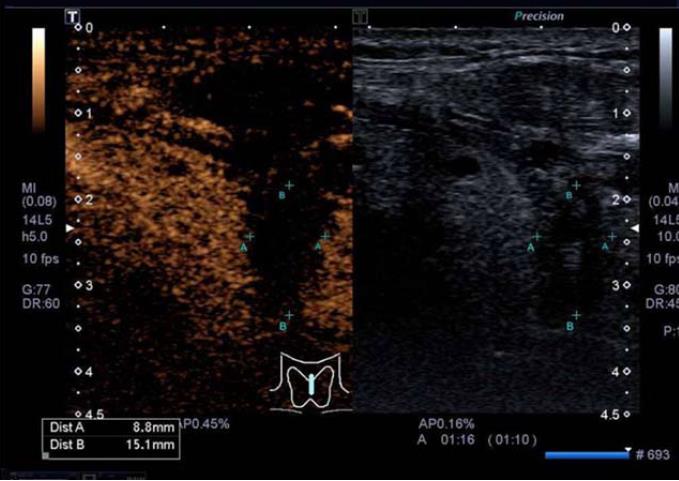
Microwave ablation group: After the patient was intubated under general anesthesia, the patient was kept in a supine position. The saline was injected around the thyroid capsule according to the location of the tumor to form a “liquid barrier.” After ultrasound guided percutaneous puncture, the microwave antenna was placed into the tumor (Figure 1). The ablation power was set at 50 W and the ablation time was set at 60-300 s. Extensive ablation of the tumor was performed. After the tumor was ablated, the ablation needle was slowly withdrawn to prevent the tumor cells from being transplanted along the needle path. Ultrasound angiography was used postoperatively to determine if ablation was complete (Figure 2).
The operative time, intraoperative loss blood, length of hospital stay, serum C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α) 24 h after operation, thyroid hormone-related changes, and complications 7 d and 30 d after operation were observed.
SPSS19.0 software was used for data analyses. Measured data are expressed as mean ± SD and the two groups were compared using the independent samples t-test. The number of cases or percentages of count data is expressed and comparison between the two groups was performed using the χ2 test. Repeated measures analysis of variance was used to compare the levels of hormones [T3, T4, thyroid stimulating hormone (TSH)] preoperatively, 7 d after surgery, and 30 d after surgery. P < 0.05 was considered statistically significant.
The surgical time, blood loss volume, and length of hospital stay in the surgical group were significantly higher than those in the microwave ablation group (P < 0.05) (Table 2).
| Group | Case | Length of hospital stay (d) | Blood loss volume (mL) | Surgical time (min) |
| Surgery group | 46 | 4.18 ± 0.55 | 33.12 ± 5.07 | 78.81 ± 12.19 |
| Microwave | 41 | 1.77 ± 0.71 | 10.32 ± 1.65 | 25.02 ± 4.14 |
| Ablation group | ||||
| t-value | 17.832 | 27.511 | 26.892 | |
| P-value | 0 | 0 | 0 |
The levels of CRP, IL-6, and TNF-α in the surgical group were significantly higher than those in the microwave ablation group (P < 0.05) (Table 3).
| Group | Case | CRP (mg/L) | IL-6 (ng/L) | TNF-α (ng/L) |
| Surgery group | 46 | 12.05 ± 2.57 | 14.44 ± 4.61 | 51.39 ± 2.86 |
| Microwave | 41 | 0.71 ± 0.39 | 4.02 ± 1.78 | 43.55 ± 5.03 |
| Ablation group | ||||
| t-value | 27.951 | 13.591 | 9.059 | |
| P-value | 0 | 0 | 0 |
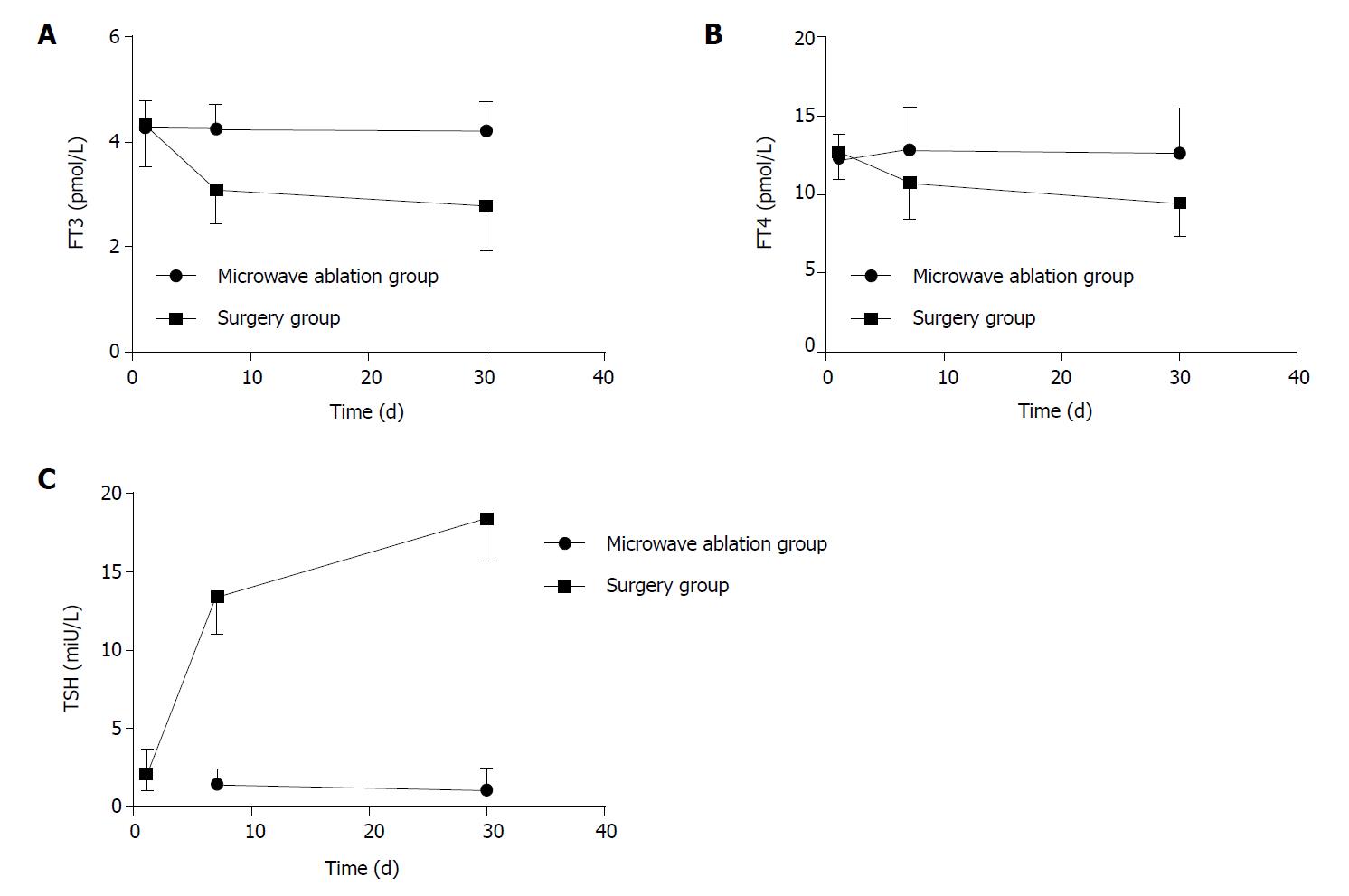
The hormone levels of the two groups (including the hormone levels of T3, T4, and TSH) were recorded before, 7 d after, and 30 d after surgery (Tables 4-6 and Figure 3). According to preoperative data analysis, there was no significant difference in thyroid hormone levels between the microwave ablation group and the surgery group (P > 0.05). Repeated measurement analysis of variance within the group found that free triiodothyronine (FT3) levels decreased significantly postoperatively compared with preoperative values (P < 0.05). In contrast, TSH levels increased significantly postoperatively compared with preoperative values (P < 0.05). Free thyroxin (FT4) levels had no significant changes after surgery (P > 0.05). Comparison between groups revealed that the FT3 and FT4 levels in the surgery group were significantly lower than those in the microwave ablation group (P < 0.05). The postoperative TSH level was significantly higher than that in the microwave ablation group (P < 0.05). There were significant interactions between the FT3, FT4, and TSH changes 7 and 30 d postoperatively and the treatment plan (P < 0.05).
| FT3 (pmol/L) | Preoperative | 7 d after surgery | 30 d after surgery |
| Microwave ablation group | 4.28 ± 0.49 | 4.25 ± 0.45 | 4.22 ± 0.53 |
| Surgery group | 4.33 ± 0.78 | 3.09 ± 0.64 | 2.78 ± 0.84 |
| FT4 (pmol/L) | Preoperative | 7 d after surgery | 30 d after surgery |
| Microwave ablation group | 12.33 ± 1.51 | 12.87 ± 2.66 | 12.67 ± 2.83 |
| Surgery group | 12.72 ± 1.68 | 10.77 ± 2.25 | 9.45 ± 2.07 |
| TSH (mIU/L) | Preoperative | 7 d after surgery | 30 d after surgery |
| Microwave ablation group | 2.11 ± 1.47 | 1.42 ± 0.91 | 1.08 ± 1.35 |
| Surgery group | 2.09 ± 1.01 | 13.44 ± 2.37 | 18.43 ± 2.67 |
In the recovery process of the two groups, patients had different degrees of pharyngeal discomfort, hoarseness, pain, parathyroid injury, incision infection, or other complications. Those patients returned to normal after 3 mo. There were no significant difference in the complications between the two groups (P > 0.05) (Table 7).
| Group | Microwave ablation group (n = 41) | Surgery group (n = 46) | χ2 | P |
| Pharyngeal discomfort | 0 | 1 | 1.508 | 0.219 |
| Hoarseness | 1 | 2 | ||
| Pain | 0 | 1 | ||
| parathyroid injury | 0 | 0 | ||
| Incision infection | 0 | 1 | ||
| Cough after drinking water | 1 | 2 | ||
| Incidence of complications | 4.9% | 15.2% |
The direction of modern surgical development is minimally invasive treatment that is to achieve the purpose of treatment with minimal surgical trauma and to minimize the impact of surgical trauma on the body. At present, the standard treatment for single PTMC is still surgical lobectomy, which is unacceptable to some patients because of its disadvantages such as large trauma, long recovery time, and medication for life[12-15]. Given that papillary thyroid cancer has “moderate” biological behavior, it is slow-growing and some patients carry no progression during their lifetime. Therefore, it is particularly necessary to find a therapeutic method that is effective, safe, minimally invasive, and more aesthetically pleasing. Microwave ablation is guided by ultrasound to make the microwave ablation electrode enter into the target tissue and ablate it through rapid hyperthermia coagulation necrosis, necrotic tissue will be absorbed by the body over time and ultimately achieve the purpose of treatment with the advantages of minimal trauma, rapid recovery, easy to use, etc[16-19]. This study compared the impact of ultrasound-guided percutaneous microwave ablation and surgical resection of PTMC on body trauma in order to explore the clinical value of ultrasound-guided microwave ablation of PTMC.
The surgical time, intraoperative blood loss, and length of hospital stay in the surgery group were significantly higher than those in the microwave ablation group (P < 0.05), indicating that microwave ablation of PTMC can significantly reduce the trauma to the patient. It is known that microwave ablation and surgical trauma as external environmental stimuli can both cause the body’s non-infectious stress response. The size and duration of stress response after surgery reflect the severity of surgical trauma[20,21]. Therefore, lower trauma during surgery can reduce the body’s stress response. In terms of reflecting the stress response of the body, it is known that CRP is synthesized by the liver and can be significantly elevated under stress conditions. The more severe the trauma, the more obvious the increase of CRP[22,23]. IL-6 is a multi-functional cytokine that is mainly produced by monocytes/macrophages and T cells and is extremely low in normal human plasma. Many pathological factors can affect the production of IL-6. Surgical trauma is one of the important factors. IL-6 is now considered to be a sensitive index of reactive tissue damage[24,25]. Similarly, TNF-α can be used as a marker to analyze the secretion of cytokines and is a sensitive marker for early trauma in tissues[26,27]. In this study, the level of stress response of postoperative patients was more accurately measured by measuring the levels of these three indicators in postoperative patients. The results revealed that the levels of CRP, IL-6, and TNF-α in the surgical group were significantly higher than those in the microwave ablation group at 24 h after operation (P < 0.05). The stress response of the patients in the surgery group was even stronger, and the microwave ablation significantly reduced the patient’s body trauma. This is because ultrasound-guided microwave ablation is guided by ultrasound under real-time guidance and avoids major organs such as large blood vessels in the puncture path. The microwave ablation electrode is rapidly and accurately implanted in the thyroid tumor lesions for ablation. It has the advantages of simpler operation, shorter time, less intraoperative blood loss, and less traumatic emergency response[28,29]. Those advantages can prompt the recovery of the patient’s health as soon as possible, shorten the patient’s hospitalization time, and improve the patient’s quality of life.
During surgical treatment of PTMC, changes in the thyroid function of the patient should cause extra attention. In this study, thyroid hormone levels were measured before, 7 d after, and 30 d after surgery in patients with microwave ablation and surgery. Thyroid function was dynamically monitored in each patient to better reflect postoperative dynamic changes of the thyroid function. Repeated-measures analysis of variance revealed that the FT3 and FT4 levels in the surgical group had a significant decrease after surgery, and the TSH increased significantly. Considering that most of the thyroid tissue was removed by surgery, the patients lost some of the endogenous thyroid function. The patients revealed a more obvious performance of hypothyroidism. In the microwave ablation group, the level of TSH slightly decreased after surgery, but the change was not obvious and there was no significant increase after surgery for a long time. This indicates that microwave ablation can better protect normal thyroid tissue than surgical resection, which is similar to the study of Baek et al[30]. It is worth noting that there was no significant change in the FT3 and FT4 levels at the 7th and 30th days after surgery in the microwave ablation group compared with the surgical group. This indicates that microwave ablation is relatively infrequent in the thyroid. Thyroid function was still maintained at a certain level after surgery and no significant reduction in thyroid function occurred. This has important implications for patients in the clinic. If the patient’s thyroid function remains stable after surgery, long-term use of thyroid hormone drugs can be avoided and the quality of life of patients can be improved.
The incidence of postoperative complications was observed in the study. The results revealed that postoperative complications occurred in 2 out of 41 patients who underwent microwave ablation. The overall incidence of complications was 4.9% in the microwave ablation group. The overall incidence of complications in the surgery group was 15.2%. There was no significant difference between the two groups (P > 0.05). Considering that the sample size was small in this study, the difference was not obvious and large sample data are needed. Long-term efficacy and complications should be further observed.
In summary, the use of microwave ablation for the treatment of PTMC has little risk of traumatic stress and safety. This technology can effectively shorten the length of hospital stay and improve the quality of life of patients. Due to the small damage caused by microwave ablation, the postoperative thyroid function is not significantly affected, which has a high clinical value.
The detection rate of papillary thyroid microcarcinoma (PTMC) has increased over time. Because thyroidectomy is prone to various complications, it can cause physical and mental harm to the patient. With the rapid development of minimally invasive techniques, microwave ablation is the main method of minimally invasive thyroid treatment, and is often used for the treatment of benign thyroid nodules. However, whether this method is indicated for the treatment of patients with PTMC is still controversial.
In this study, microwave ablation was used to treat patients with PTMC. It is hoped that microwave ablation can achieve the same effect as thyroid surgery, and can reduce the complications caused by thyroid surgery.
The aim of this study was to compare the efficacy of thyroidectomy and microwave ablation in the treatment of PTMC and their trauma to the patient’s body, to find a more appropriate treatment for patients.
Eighty-seven patients diagnosed with papillary thyroid carcinoma were enrolled. There were 46 cases in the surgical group and 41 cases in the microwave ablation group. Microwave ablation and thyroidectomy were performed in each group. The operative time, intraoperative blood loss, hospitalization time, serum C-reactive protein (CPR), interleukin-6 (IL-6), and tumor necrosis factor-α (TNF-α) were observed in the two groups. The changes of thyroid-related hormones and the postoperative complications of the two groups were observed 7 d and 30 d after surgery.
The operative time, intraoperative blood loss, hospitalization time, CPR, IL-6, and TNF-α in the surgical group were significantly higher than those in the microwave ablation group. The free triiodothyronine (FT3) and free thyroxin (FT4) levels in the surgical group were significantly lower than those in the microwave ablation group, while thyroid stimulating hormone (TSH) was significantly higher than that in the microwave ablation group. The complications of the two groups were similar.
Microwave ablation for the treatment of PTMC has less stress response and higher safety. It can effectively shorten the hospitalization time of patients and improve the life quality. The thyroid function of patients after operation is not affected, so microwave ablation treatment of PTMC has a high clinical value.
With the development of minimally invasive treatment, minimally invasive treatment methods are increasingly applied to various diseases, so that patients can achieve therapeutic goals with minimal surgical trauma, and minimize the impact of surgical trauma on the body. Minimally invasive surgery is a new technological innovation that still requires large sample and multi-center clinical research support to evaluate long-term safety and efficacy.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Arisawa T, Kim ES, Knittel T S- Editor: Wang JL L- Editor: Wang TQ E- Editor: Tan WW
| 1. | Ito Y, Oda H, Miyauchi A. Insights and clinical questions about the active surveillance of low-risk papillary thyroid microcarcinomas. Endocr J. 2016;63:323-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Tarasova VD, Tuttle RM. Current Management of Low Risk Differentiated Thyroid Cancer and Papillary Microcarcinoma. Clin Oncol (R Coll Radiol). 2017;29:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Dobrinja C, Pastoricchio M, Troian M, Da Canal F, Bernardi S, Fabris B, de Manzini N. Partial thyroidectomy for papillary thyroid microcarcinoma: Is completion total thyroidectomy indicated? Int J Surg. 2017;41 Suppl 1:S34-S39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Chung YS, Choe JH, Kang KH, Kim SW, Chung KW, Park KS, Han W, Noh DY, Oh SK, Youn YK. Endoscopic thyroidectomy for thyroid malignancies: comparison with conventional open thyroidectomy. World J Surg. 2007;31:2302-2306; discussion 2307-2308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 137] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 5. | Kang JB, Kim EY, Park YL, Park CH, Yun JS. A comparison of postoperative pain after conventional open thyroidectomy and single-incision, gasless, endoscopic transaxillary thyroidectomy: a single institute prospective study. Ann Surg Treat Res. 2017;92:9-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Liu YJ, Qian LX, Liu D, Zhao JF. Ultrasound-guided microwave ablation in the treatment of benign thyroid nodules in 435 patients. Exp Biol Med (Maywood). 2017;242:1515-1523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 56] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 7. | Jin H, Fan J, Liao K, He Z, Li W, Cui M. A propensity score matching study between ultrasound-guided percutaneous microwave ablation and conventional thyroidectomy for benign thyroid nodules treatment. Int J Hyperthermia. 2018;1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Wu W, Gong X, Zhou Q, Chen X, Chen X, Shi B. US-guided percutaneous microwave ablation for the treatment of benign thyroid nodules. Endocr J. 2017;64:1079-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Li J, Liu Y, Liu J, Qian L. Ultrasound-guided percutaneous microwave ablation versus surgery for papillary thyroid microcarcinoma. Int J Hyperthermia. 2018;34:653-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 73] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 10. | Sun H, Dionigi G. Influence of specialized clinic on initial treatment choice in localized thyroid cancer. Eur J Surg Oncol. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Teng D, Sui G, Liu C, Wang Y, Xia Y, Wang H. Long-term efficacy of ultrasound-guided low power microwave ablation for the treatment of primary papillary thyroid microcarcinoma: a 3-year follow-up study. J Cancer Res Clin Oncol. 2018;144:771-779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 72] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 12. | Mazzaferri EL. Managing thyroid microcarcinomas. Yonsei Med J. 2012;53:1-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Morris LG, Sikora AG, Tosteson TD, Davies L. The increasing incidence of thyroid cancer: the influence of access to care. Thyroid. 2013;23:885-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 384] [Article Influence: 32.0] [Reference Citation Analysis (0)] |
| 14. | Rodrigues AC, Penna G, Rodrigues E, Castro P, Sobrinho-Simões M, Soares P. The Genetics of Papillary Microcarcinomas of the Thyroid: Diagnostic and Prognostic Implications. Curr Genomics. 2017;18:244-254. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 15. | Boucai L, Bernet V, Shaha A, Shindo ML, Stack BC, Tuttle RM. Surgical considerations for papillary thyroid microcarcinomas. J Surg Oncol. 2017;116:269-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Yue W, Wang S, Wang B, Xu Q, Yu S, Yonglin Z, Wang X. Ultrasound guided percutaneous microwave ablation of benign thyroid nodules: safety and imaging follow-up in 222 patients. Eur J Radiol. 2013;82:e11-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 17. | Qin M, Zou F, Zheng M, Zhao H. Systemic stress responses after laparoendoscopic single-site hepatectomy: a perspective controlled study. Hepatogastroenterology. 2012;59:1204-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Yu Y, Yanli H, Jing Z, Zhiyu H, Xia MA, Ruifang XU. Ultrasound-guided percutaneous microwave ablation for subserosal uterine fibroids. J Minim Invasive Gynecol. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Wang Z, Tang X, Qi X, Shi Y, Chi J, Li P, Zhai B. Feasibility, safety, and efficacy of ultrasound-guided percutaneous microwave ablation for giant hepatic hemangioma. Int J Hyperthermia. 2018;1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Hsiao CY, Huang KW. Irreversible Electroporation: A Novel Ultrasound-guided Modality for Non-thermal Tumor Ablation. J Med Ultrasound. 2017;25:195-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Yan J, Qiu T, Lu J, Wu Y, Yang Y. Microwave ablation induces a lower systemic stress response in patients than open surgery for treatment of benign thyroid nodules. Int J Hyperthermia. 2018;34:606-610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Yue WW, Wang SR, Lu F, Sun LP, Guo LH, Zhang YL, Li XL, Xu HX. Radiofrequency ablation vs. microwave ablation for patients with benign thyroid nodules: a propensity score matching study. Endocrine. 2017;55:485-495. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 23. | De Bernardi IC, Floridi C, Muollo A, Giacchero R, Dionigi GL, Reginelli A, Gatta G, Cantisani V, Grassi R, Brunese L. Vascular and interventional radiology radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: literature review. Radiol Med. 2014;119:512-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Yao X, Huang J, Zhong H, Shen N, Faggioni R, Fung M, Yao Y. Targeting interleukin-6 in inflammatory autoimmune diseases and cancers. Pharmacol Ther. 2014;141:125-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 489] [Article Influence: 40.8] [Reference Citation Analysis (0)] |
| 25. | Vainer N, Dehlendorff C, Johansen JS. Systematic literature review of IL-6 as a biomarker or treatment target in patients with gastric, bile duct, pancreatic and colorectal cancer. Oncotarget. 2018;9:29820-29841. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 76] [Cited by in RCA: 107] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 26. | Natkaniec M, Dworak J, Hankus J, Sanak M, Pędziwiatr M, Major P, Lichołai S, Budzyński A. Influence of TNF-α promoter variability on stage and grade in individuals with colorectal cancer. Pol J Pathol. 2018;69:150-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 27. | Shen J, Xiao Z, Zhao Q, Li M, Wu X, Zhang L, Hu W, Cho CH. Anti-cancer therapy with TNFα and IFNγ: A comprehensive review. Cell Prolif. 2018;51:e12441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 114] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 28. | Ha EJ, Baek JH, Lee JH. The efficacy and complications of radiofrequency ablation of thyroid nodules. Curr Opin Endocrinol Diabetes Obes. 2011;18:310-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 29. | Kim JH, Baek JH, Lim HK, Ahn HS, Baek SM, Choi YJ, Choi YJ, Chung SR, Ha EJ, Hahn SY, Jung SL, Kim DS, Kim SJ, Kim YK, Lee CY, Lee JH, Lee KH, Lee YH, Park JS, Park H, Shin JH, Suh CH, Sung JY, Sim JS, Youn I, Choi M, Na DG; Guideline Committee for the Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. 2017 Thyroid Radiofrequency Ablation Guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018;19:632-655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 259] [Cited by in RCA: 444] [Article Influence: 63.4] [Reference Citation Analysis (0)] |
| 30. | Baek JH, Kim YS, Lee D, Huh JY, Lee JH. Benign predominantly solid thyroid nodules: prospective study of efficacy of sonographically guided radiofrequency ablation versus control condition. AJR Am J Roentgenol. 2010;194:1137-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 225] [Article Influence: 15.0] [Reference Citation Analysis (0)] |