Published online Nov 26, 2018. doi: 10.12998/wjcc.v6.i14.842
Peer-review started: September 10, 2018
First decision: October 11, 2018
Revised: October 16, 2018
Accepted: October 23, 2018
Article in press: October 23, 2018
Published online: November 26, 2018
Processing time: 78 Days and 5.6 Hours
Choledochocele (also known as type III choledochal cyst according to Todani’s classification) is a cystic dilation of the distal segment of the common bile duct protruding into the duodenal lumen. Cases are rare and the etiology remains unclear. It is usually misdiagnosed as peptic ulcer, as in the patient whose case is described here. Multislice spiral computed tomography and magnetic resonance cholangiopancreatography may be comparable to endoscopic retrograde cholangiography for diagnosis of choledochocele. Both endoscopic therapy and open surgical management are safe options, and size of the cyst plays a role in the decision-making for which approach to apply. A 50-year-old woman admitted to our hospital with upper abdominal pain caused by choledochocele with large size was successfully treated by open surgical management. We present the details of her case in this case report and discuss the recent literature on such cases and their therapeutic management.
Core tip: Choledochocele, also known as the type III choledochal cyst according to Todani’s classification, is a rare disease. We present the case of an adult female with a large-size choledochocele that was successfully treated by open surgery. We also provide a detailed discussion of the recent literature on such cases and their therapeutic management.
- Citation: Yang J, Xiao GF, Li YX. Open surgical treatment of choledochocele: A case report and review of literature. World J Clin Cases 2018; 6(14): 842-846
- URL: https://www.wjgnet.com/2307-8960/full/v6/i14/842.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i14.842
Choledochocele (also known as type III choledochal cyst according to Todani’s classification[1]), is a cystic dilation of the distal segment of the common bile duct protruding into the duodenal lumen. Considered rare, these cases comprise less than 2% of all reported cases of choledochal cyst[2]. The rarity of the disease serves to obscure its diagnosis and treatment.
The case described herein, accompanied by a review of the current literature, will help to increase our knowledge about this rare disease.
A 50-year-old woman was admitted to our department with an > 10-year history of repeated upper abdominal pain, but without vomiting, jaundice, chills and fever. During that period, she had been admitted to the gastroenterology outpatient clinic several times, where she was diagnosed with and treated for chronic nonatrophic gastritis; yet, her symptom was never alleviated.
Physical examination produced no positive findings, except a mild tenderness on the upper abdomen. Routine blood panel, liver function markers, blood amylase and tumor marker test results were normal. Abdominal ultrasound showed gallstones and nondilated intrahepatic and extrahepatic bile ducts. As such, the cause of the patient’s presenting symptom remained undetermined.
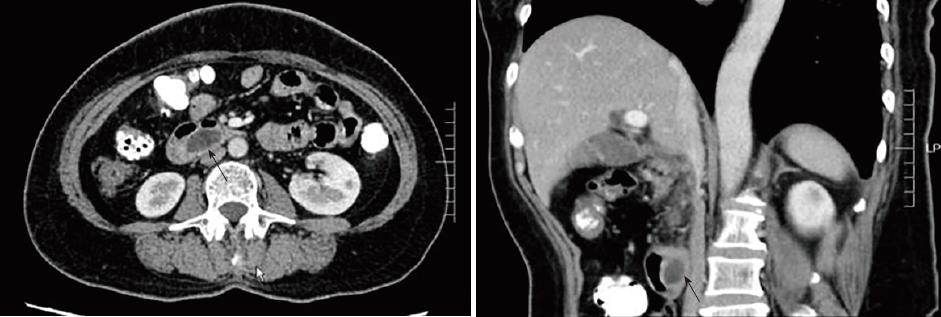
Multislice spiral computed tomography showed a 3.0 cm-long, 1.5 cm-wide cystic lesion at the junction of the descending and horizontal portion of the duodenum (Figure 1). Duodenoscopy was performed and showed a huge submucosal mass connected to the major duodenal papilla; the distal segment of the common bile duct was not evident in endoscopic retrograde cholangiopancreatography (ERCP) (Figure 2). We considered these findings to indicate a choledochocele, and we decided to treat with open surgical management.
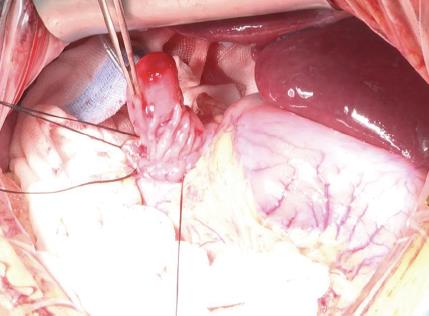
The cystic lesion became grossly visible when the descending part of the duodenum was incised longitudinally, and complete cystectomy was performed (Figure 3). Then, the orifices of the common bile duct and pancreatic duct were found and each marked with 6-Fr silicon tube. Sphincteroplasty was performed under the guidance of the silicon tube. Cholecystectomy was also carried out to address the gallstones. An abdominal cavity drainage tube and a duodenostomy tube were placed. A T-tube was also placed, to facilitate external drainage of bile. Lastly, a nasojejunal nutrition tube was placed perioperatively, and enteral nutrition support was started on the 3rd day after surgery. The operation time was 4 h and intraoperative blood loss was 120 mL. Postoperative pathological examination of the resected tissue showed duodenal mucosa with regional low-grade intraepithelial neoplasia inside the choledochocele.
At 1 wk postoperation, the nasojejunal nutrition tube was removed and the duodenostomy tube was occluded; at this time, oral feeding was initiated and tolerated without event. The postoperative period remained uneventful, and the patient was discharged at 10 d after the operation. At 45 d postoperation, the T-tube and duodenostomy tube were removed. At the 1-year follow-up, the patient had survived and was asymptomatic.
The first case of choledochocele was reported by Wheeler[3] in 1915. The report described the anomaly as a small, tense cyst occupying a position in or about the orifice of the common bile duct[3]. Since then, with the development of medical techniques like endoscopy and imaging, the number of publications on choledochocele has steadily increased.
In 1993, Masetti et al[4] reviewed 116 cases of choledochocele reported in the literature to date. In 2015, Lobeck et al[5] reviewed 71 individual case reports as well as 42 institutional reviews, totaling 254 cases of choledochocele; unfortunately, the authors did not affirm whether or not there were duplications between the included cases. A single case series of choledochocele including 28 patients was reported by Ziegler et al[6] in 2009, representing the largest institution-based collection of case data. In this article, we summarized 22 case report studies of adult choledochocele patients receiving treatment between 1995 and 2015 in PubMed database (Table 1).
| Author | Clinical presentation | Treatment | Malignancy | Symptom relief |
| Eisenman 1995 | Abdominal pain | ET | Not noted | Yes |
| Tajiri 1996 | Abdominal pain | OST | No | Yes |
| Tanno 1996 | Jaundice, fever | ET | Not noted | Yes |
| Krepel 1997 | Anaemia, Abdominal pain | OST | No | Yes |
| Iwata 1998 | Abdominal pain, fever | OST | No | Not noted |
| Chatila 1999 | Abdominal pain | ET | No | Yes |
| Adamek 2000 | Nausea, abdominal pain | ET | Not noted | Yes |
| Groebli 2000 | Abdominal pain | OST | Not noted | Not noted |
| Can 2006 | Abdominal pain | OST | Not noted | Yes |
| Moparty 2006 | Abdominal pain | OST | Not noted | Not noted |
| Berger 2007 | Abdominal pain, nausea | ET | No | Yes |
| Hackert 2007 | Abdominal pain | OST | No | Not noted |
| Izumiya 2007 | Abdominal pain | ET | Not noted | Yes |
| Kawakami 2007 | None | ET | No | - |
| Lakhtakia 2007 | Abdominal pain, vomit | ET | No | Yes |
| Kaye 2008 | Abdominal pain | OST | Not noted | Yes |
| Park 2009 | Abdominal pain | ET | No | Yes |
| Amezaga 2010 | Jaundice, anorexia | ET | Not noted | Yes |
| Cakmakci 2012 | Abdominal pain | OST | Not noted | Yes |
| Darji 2012 | Abdominal pain, vomit | ET | Not noted | Not noted |
| Zhu 2014 | Abdominal pain, vomit | ET | Not noted | Yes |
| Villa 2015 | Abdominal pain | ET | Not noted | Yes |
In Japan, choledochocele has been regarded as the type III choledochal cyst (according to Todani’s classification[1]) and reportedly accounts for the lowest proportion of choledochal cyst case series[2]. However, both Ziegler et al[6] and Dong et al[7] considered that the choledochal cysts should not include the choledochocele because patients with choledochocele differ from those with choledochal cyst in age, sex, presentation, pancreatic ductal anatomy, and their management. Choledochoceles were classified as type A and type B based on the anatomic appearance by Sarris and Tsang, and the type A Choledochoceles were further divided into 3 subtypes (intraluminal with common opening for the common bile duct and pancreatic duct, intraluminal with separate openings for the common bile duct and pancreatic duct and completely intramural)[8]. Other classifications had also been proposed like Kagiyama[9] and Horaguchi[10], however none has been widely accepted.
The etiology of the choledochocele remains unclear. Tanaka[11] suggested that the mechanism for formation was failed regression of a bile duct during embryogenesis. However, Sterling[12] considered that some choledochocele appear to be acquired and proposed that papillary stenosis or sphincter of Oddi dysfunction may cause obstruction to bile flow, resulting in increased pressure within the distal bile duct, which could then evaginate into the duodenum. Sarris and Tsang[8], in the review of 24 patients, reported that the epithelium inside the choledochocele was duodenal mucosa in 63% of the cases and biliary tract epithelium or unclassifiable glandular epithelium in 37% of the cases.
In histopathology, the presence of intestinal mucosa creates controversy as to whether choledochocele is a type of duodenal duplication cyst or a unique entity. Congenital intraluminal duodenal diverticulum has been suggested in relation to the pathogenesis of choledochocele in young children, because most cases describe duodenal mucosa. However, unlike congenital forms, in older patients a papillary stenosis may cause dilatation of the ampulla by way of an inflammatory process induced by stasis of bile and pancreatic juice. Thus, biliary tract epithelium and undifferentiated epithelium are predominant later on[13].
Abdominal pain is the most common symptom of choledochocele, others include nausea, vomiting and jaundice. Image examination plays an important role in the diagnosis. Noninvasive B-ultrasound examination can detect cystic mass in the duodenal cavity; however, the image could be disturbed by intestinal gas. Usually, there are no specific findings, as in our case. Endoscopic ultrasound could show the wall layers of the cyst as well as the connection with the pancreaticobiliary tree, it also might guide both classification of the lesion and treatment decisions[14]. Some think the confirmation of a choledochocele appears to be best made by ERCP.
In the literature, ERCP has been performed in 67% of the reported cases, and this method holds the benefit of simultaneous treatment implementation. Multislice spiral computed tomography and magnetic resonance cholangiopancreatography are considered to have comparable specificity and sensitivity, and may replace ERCP for diagnosis[15,16]. In our patient, both endoscopic and radiologic techniques were used to obtain an optimal image.
Open surgical management, like transduodenal complete cyst excision with sphincteroplasty, was performed by Wheeler on the original choledochocele case (a 65-year-old male patient) with success, and is still frequently performed. In 1974, endoscopic sphincterotomy treatment was implemented for the first time by Mane et al[17], on a 21-year-old female patient. Since then, endoscopy has been recognized as a feasible alternative treatment with satisfactory results. Both therapies have been applied successfully in pediatric patients[18,19].
The choice of treatment method is still uncertain, however, and size of the cyst plays a role in the clinical decision-making process. Three centimeters in diameter may be the cut-off value, above which transduodenal cyst resection should be performed[5]. However, the fundamental purpose of choledochocele treatment should be to maintain normal outflow of bile and pancreatic juice, with the additional objective of minimizing risk of malignancy. The large diameter of the cyst lesion in our patient led us to decide to perform open surgery. Almost all of the patients have relieved after treatment either by endoscopy or surgery. Malignant transformation of a choledochocele has been rarely reported[20], and wasn’t happened in the case reports we reviewed in the table. However, choledochocele might be accompanied or caused by pancreaticobiliary maljunction, in such a condition, biliary tract malignancy was more frequent according to Horaguchi’s report[10]. Nonetheless, sustaining follow-up could be beneficial for patients who are asymptomatic or accidentally discovered.
In conclusion, choledochocele is a rare disease and the choice of treatment method is still controversial. For choledochocele with large-size (i.e., > 3 cm in diameter), we suggest treatment with open surgical management, according to our case’s successful outcome.
A 50-year-old woman with upper abdominal pain lasting for more than 10 year.
Choledochocele.
No positive laboratory test results were found.
A 3.0 cm-long, 1.5 cm-wide cystic lesion at the junction of the descending and horizontal portion of the duodenum.
Duodenal mucosa with regional low-grade intraepithelial neoplasia inside the choledochocele.
Open surgical management involving cyst excision with sphincteroplasty.
Choledochocele is considered a rare disease, and cases are seldom reported.
Choledochocele, also known as the type III choledochal cyst according to Todani’s classification, is a cystic dilation of the distal segment of the common bile duct protruding into the duodenal lumen, and accounts for < 2% of all reported cases of choledochal cyst.
Choledochocele is a rare disease and usually misdiagnosed as peptic ulcer. For the choledochocele with large size (i.e., > 3 cm in diameter), we suggest treatment with open surgical management, according to our case’s successful outcome.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Hashimoto R, Sandhu DS, Tsolakis AV S- Editor: Dou Y L- Editor: A E- Editor: Song H
| 1. | Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 934] [Cited by in RCA: 835] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 2. | Yamaguchi M. Congenital choledochal cyst. Analysis of 1,433 patients in the Japanese literature. Am J Surg. 1980;140:653-657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 321] [Cited by in RCA: 272] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Wheeler W. An unusual case of obstruction to the common bile‐duct (choledochocele?). Brit J Surg. 1940;27:446-448. [RCA] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 4. | Masetti R, Antinori A, Coppola R, Coco C, Mattana C, Crucitti A, La Greca A, Fadda G, Magistrelli P, Picciocchi A. Choledochocele: changing trends in diagnosis and management. Surg Today. 1996;26:281-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Lobeck IN, Dupree P, Falcone RA Jr, Lin TK, Trout AT, Nathan JD, Tiao GM. The presentation and management of choledochocele (type III choledochal cyst): A 40-year systematic review of the literature. J Pediatr Surg. 2017;52:644-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Ziegler KM, Pitt HA, Zyromski NJ, Chauhan A, Sherman S, Moffatt D, Lehman GA, Lillemoe KD, Rescorla FJ, West KW. Choledochoceles: are they choledochal cysts? Ann Surg. 2010;252:683-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Dong JH, Zheng XH, Xia HT, Zhao XQ, Liang B, Yang T, Zeng JP, Huang ZQ. Cystic dilation of bile duct: new clinical classification and treatment strategy. Zhonghua Xiaohuawaike Zazhi. 2013;12:370-377. [DOI] [Full Text] |
| 8. | Sarris GE, Tsang D. Choledochocele: case report, literature review, and a proposed classification. Surgery. 1989;105:408-414. [PubMed] |
| 9. | Kagiyama S, Okazaki K, Yamamoto Y, Yamamoto Y. Anatomic variants of choledochocele and manometric measurements of pressure in the cele and the orifice zone. Am J Gastroenterol. 1987;82:641-649. [PubMed] |
| 10. | Horaguchi J, Fujita N, Kobayashi G, Noda Y, Ito K, Takasawa O. Clinical study of choledochocele: is it a risk factor for biliary malignancies? J Gastroenterol. 2005;40:396-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Tanaka T. Pathogenesis of choledochocele. Am J Gastroenterol. 1993;88:1140. [PubMed] |
| 12. | Sterling JA. Diverticula in the terminal portion of the common bile duct. Am J Pathol. 1949;25:325-337. [PubMed] |
| 13. | Schimpl G, Sauer H, Goriupp U, Becker H. Choledochocele: importance of histological evaluation. J Pediatr Surg. 1993;28:1562-1565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 14. | Law R, Topazian M. Diagnosis and treatment of choledochoceles. Clin Gastroenterol Hepatol. 2014;12:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 46] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Groebli Y, Meyer JL, Tschantz P. Choledochocele demonstrated by computed tomographic cholangiography: report of a case. Surg Today. 2000;30:272-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Park DH, Kim MH, Lee SK, Lee SS, Choi JS, Lee YS, Seo DW, Won HJ, Kim MY. Can MRCP replace the diagnostic role of ERCP for patients with choledochal cysts? Gastrointest Endosc. 2005;62:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 79] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 17. | Deyhle P, Schnaars P, Meyer HJ, Nüesch HJ, Akovbiantz A. Electrosurgical removal of a choledochocele through an endoscope introduced by mouth (author’s transl). Dtsch Med Wochenschr. 1974;99:71-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Mane S, Arlikar J, Dhende N. Choledochocele: An unusual presentation in a premature neonate. J Indian Assoc Pediatr Surg. 2012;17:28-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Saeki I, Takahashi Y, Matsuura T, Takahata S, Tanaka M, Taguchi T. Successful endoscopic unroofing for a pediatric choledochocele. J Pediatr Surg. 2009;44:1643-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Ladas SD, Katsogridakis I, Tassios P, Tastemiroglou T, Vrachliotis T, Raptis SA. Choledochocele, an overlooked diagnosis: report of 15 cases and review of 56 published reports from 1984 to 1992. Endoscopy. 1995;27:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 47] [Article Influence: 1.6] [Reference Citation Analysis (0)] |