Published online Nov 26, 2018. doi: 10.12998/wjcc.v6.i14.836
Peer-review started: September 12, 2018
First decision: October 11, 2018
Revised: October 12, 2018
Accepted: October 23, 2018
Article in press: October 22, 2018
Published online: November 26, 2018
Processing time: 76 Days and 1.5 Hours
Pelvic osteotomy is commonly used to adjust acetabula dysplasia for congenital dislocation of the hip, whereas congenital insensitivity to pain with anhidrosis (CIPA) is a rare hereditary disease that often has the characteristics of joint development deformity and easy fracture. This article reports the case involving a CIPA patient who was surgically treated by Chiari pelvic osteotomy and proximal femoral rotation osteotomy for congenital dislocation of the left hip joint and was provided long-term follow-up for redislocation and bilateral femoral head absorption.
Core tip: Reports of congenital insensitivity to pain with anhidrosis (CIPA) cases are relatively rare, and there is no standard treatment prescription. We report a case of postoperative redislocation of the hip in a patient with CIPA in this article, and try to explore the causes of this situation and look for a solution.
- Citation: Wang R, Liu Y, Zhou YY, Wang JY, Xu ZJ, Chen SY, Wang QQ, Yuan P. Postoperative redislocation of the hip in a patient with congenital insensitivity to pain with anhidrosis: A case report and review of literature. World J Clin Cases 2018; 6(14): 836-841
- URL: https://www.wjgnet.com/2307-8960/full/v6/i14/836.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i14.836
Congenital insensitivity to pain with anhidrosis (CIPA) is a rare autosomal recessive genetic disease, mainly caused by mutations in the neurotrophic tyrosine receptor kinase 1 (NTRK1) gene. Patients often experience repeated fractures and joint deformations. There is no standard treatment prescription. In this article, we report a case of postoperative redislocation of the hip in a patient with CIPA.
The present female patient was born in 2000 and had suffered multiple fractures in succession throughout the entire body as well as bilateral hip joint dislocation. Since she was four and a half years old, she had experienced fractures involving the left heel, left tibia, left femur, and right femur. The left tibia and right femur fractures occurred twice. She also suffered from repeated, long-term and unexplained high fevers from 2 mo old to 6 years old. Subsequently, the fevers were controlled, except during admissions when the patient reported anxiety. Although she showed a congenital insensitivity to pain, her temperature sensation was normal. When the patient was 2 years old, she began to show a self-mutilation tendency by biting the tip of her tongue twice. Moreover, when she was 10 years old, she bit an entire fingernail and approximately 1/3 of the finger. After her parents prevented her actions, no additional similar behaviors were exhibited. The patient’s intelligence level was normal, and she presented a light-colored sclera, anhidrosis, tears when crying, and no obviously unusual skin thickness, elasticity or color. She was preliminarily diagnosed with CIPA, incomplete osteogenesis, and other hereditary bone-forming disorders.
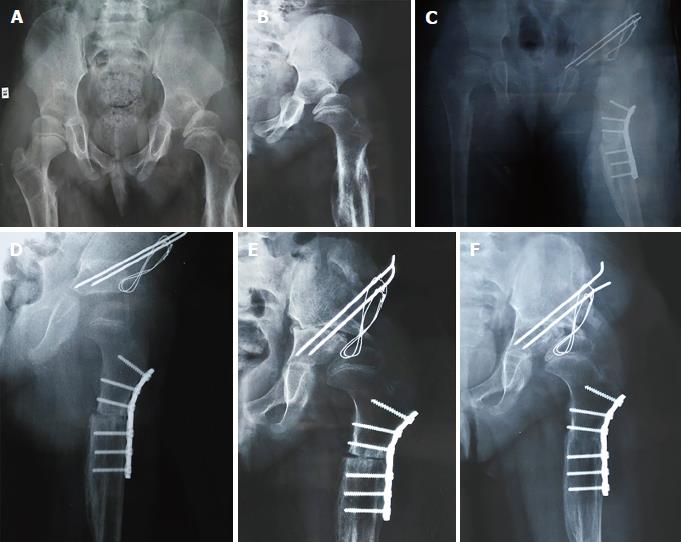
When the patient was 6 years old, she experienced an upper left femur fracture caused by a slight strike. Her parents chose conservative treatment, and the bone healed well. Subsequently, a left hip dislocation occurred when she was 7 years old (Figure 1A), and 2 mo of conservative treatment did not improve the situation (Figure 1B). Thus, she was admitted to our hospital for further treatment. The admission check showed the following: general situation, normal; left hip joint activity, slightly limited; no pain; Allis and Trendelenburg syndrome, positive; and left lower limb shortened by approximately 2 cm. A pelvic X-ray showed the following: healed deformity after fracture of the upper segment of the left femur; dislocation of the left hip; slightly flattening of the ipsilateral femoral head; left acetabular index of 28° and center-edge (CE) angle of 14°; right acetabular index of 20° and CE angle of 26°; left femoral head approximately 0.4 cm longer than the right; discontinuous left Shenton line; and Crown type II and Tonnis II degree of left hip dislocation.
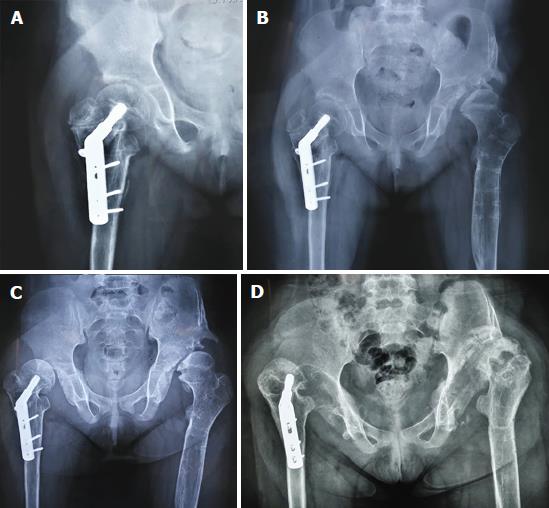
The patient has been followed to the present. After the operation, it was found during the follow-up that the internal fixation position was good. The bone grew and healed well. Pelvic X-rays (Figure 1C) at 1 d after the operation showed that the acetabulum contained well; the left acetabular index was 21°, and the CE angle was 23°. The left femoral head was equal to the right in height, and the left Shenton line was continuous. One month after the operation (Figure 1D), it was found that the acetabular relationship was good, and the fracture healed well with internal fixation. Two months after the operation (Figure 1E), wear-and-tear absorption of bone was observed on the outside edge of the top portion of the left acetabulum. The left femoral head moved upward, with the acetabular index reaching up to the 33°; the left femoral head was 0.7 cm higher than the right, and the Shenton line was discontinuous. All of these findings could be described as clinical type Crown type 1 and Tonnis 2°. The patient’s family requested conservative treatment. Five months after the operation (Figure 1F), it was found that the end of the osteotomy healed well, the upper margin of the left acetabulum was further absorbed, the level of the femoral head was not significantly increased, and the fracture healed well. Taking into account the patient’s repeated fracture history and acetabular absorption, we told the patient to reduce weight bearing on the lower limbs. One year after the left hip surgery, she was readmitted for open reduction and internal fixation due to a right femoral intertrochanteric fracture (Figure 2A) after trauma. Fourteen months after the left hip surgery (2 mo after the right femur surgery, Figure 2B), the left pelvis and upper part of the femur were removed from the internal fixation device; then, the left femoral head was moved further upward to a position 0.9 cm higher than the right. The clinical classification was Crown type 2 and Tonnis 3°, and left acetabular wear increased. The false joint occurred in the left acetabulum, and there was no further visible absorption. Then at 1 year after the operation (Figure 2C), the patient was found to have a right hip dislocation for the first time even after a manual joint reset, and her family members requested conservative treatment. The dislocation degree of the right hip joint was Crown type 2/Tonnis 2°, the right acetabular index was 20°, and the bilateral femoral head was not significantly changed. One year after the operation on the right femoral intertrochanteric region (Figure 2D), the double femoral head was completely absorbed, and the bilateral acetabulum lost its normal shape.
The results of a genetic test (Table 1) in January 2018 showed the following: (1) NTRK1 (intron 14) gene mutation (mutation classification: pathogenic); (2) NTRK1 (exon 14) genetic variation (mutation classification: likelihood of disease); and (3) GORAB (exon 4) gene mutation (mutation classification: probability of disease). Among these findings, the NTRK1 gene suggested CIPA, and the GORAB gene mutation suggests senile skin with bone dysplasia. According to the genetic test results and clinical symptoms, the patient was considered to have CIPA.
| Gene (Location) | Nucleic acid variation (Amino acid variation) | Heterozygosity | Disease (Genetic model) | Pathogenicity | Parent source |
| NTRK1 (exon 14) | NM_002529 | Com_het | Congenital sensory neuropathy (AR) | Likely pathogenic | Maternal |
| c.A1787G (p.Asp596Gly) | |||||
| NTRK1 (intron 14) | NM_002529 | Com_het | Congenital insensitivity to pain with anhidrosis (AR) | Pathogenic | Paternal |
| c.1806-2A>G | |||||
| GORAB (exon 4) | NM_002529 | Het | Senile skin with dysplasia of bone (AR) | Likely pathogenic | Maternal |
| c.G733A (p.Ala245Thr) |
CIPA is a rare autosomal recessive genetic disease, mainly caused by mutations in the NTRK1 gene; NGF is a neurotrophic factor, and TrkA is an NGF receptor tyrosine kinase encoded by the NTRK1 gene. The Ngf-Trka system supports the survival and maintenance of NGF-dependent neurons in the development process and plays a key role in pain, itching and inflammation[1]. Clinical manifestations include impaired temperature sensation and insensitivity to deep and shallow pain, but other feelings are rarely affected. They also show no sweating and exhibit different levels of mental disorders. Because there is no sweat, this condition often presents with unexplained fever; moreover, as there is no sensitivity to pain, patients display different degrees of self-injuring tendencies, often biting their tongue, lips, oral mucosa, and fingers, which often results in bruises, scars, and skin infections. In addition, patients often experience repeated fractures and joint deformations. Many have Charcot joint and fractures occur in the early years. Fractures and deformities can occur in bone joints throughout the body but are more prevalent in the lower extremities; most of the causes of fracture and dislocation are not well documented and are often due to minor injuries. Liu et al[2] through genetic studies showed that mutations in different locations of the NTRK1 gene have different effects on intelligence levels; gene mutations in the core of the protein often have a greater impact on intelligence, and dislocation mutations located in the peripheral NTRK1 protein do not endanger important structural domains and tend to cause mild symptoms, usually without mental impairment. In 1996, Szöke et al[3] reported that CIPA patients show hip joint disease; Bar-on confirmed his data and stated that fractures often occur in the lower extremities and that patients often present age-independent joint dislocation and risk of infection[4]. In the preset case, the intelligence level was normal, there was no sweat, but there was insensitivity to pain, high fever of unknown origin, easy fracturing, joint dysplasia or other typical characteristics. The genetic testing is in line with the CIPA gene variant phenotype, and thus, with the clinical diagnosis of CIPA. This patient’s intellectual development has not been affected; however, lower extremity fractures and joint symptoms were obvious.
Congenital dislocation of the hip, formerly known as primary dislocation of the hip, was later renamed “developmental dislocation of the hip” (DDH). The indicated cases include hip relaxation, acetabular dysplasia, dislocation of the hip and subluxation.
The treatment principle for DDH is early diagnosis and early treatment, as this can often mean that less invasive treatment is possible, and outcomes are significantly improved if treatment is initiated at an early stage and certainly before 6 wk of age[5]. Two to three-year-old children often undergo nonsurgical treatment, with a closed reduction after the use of frog-shaped gypsum or fixation of subbranches. Some countries such as Germany have universal screening programmes and have seen a decrease in the rates of surgical reduction in DDH[6]. Patients over 3 years old are treated by surgery. The goal of the surgical treatment in previously untreated juvenile hip displacement is to achieve a stable and concentric reduction of the femoral head with the best range of motion and without severe complications related to avascular necrosis and stiffness of hip joint[7]. The commonly used surgical methods are: (1) Salter iliac osteotomy; (2) Chiari pelvic osteotomy; (3) Pemberton articular iliac osteotomy; and (4) multiple osteotomy of the pelvis. Femoral shortening and derotation osteotomy was classically reserved for children older than 3 years and has now been shown to be a useful and prudent procedure in younger patients[8].
In the case of this patient, the pelvic film showed outward movement from the left femoral head, but there was no obvious dislocation when she was 6 year old. At 7 years of age, there was left hip dislocation. Chiari osteotomy seemed to be the most appropriate surgical method, so Chiari pelvic osteotomy and proximal femoral rotation plus osteotomy were used to treat dislocation of the hip, postoperatively and 1 mo after surgery; the reduction effect was good and more satisfactory. However, after 2 mo of surgery, resorption of the upper margin of the acetabular bone was found, the acetabular index recovered, and the femoral head moved upward. During the subsequent review, the acetabular absorption gradually increased, and the femoral head gradually moved upward. At the age of 9 years, the right hip dislocation was found without definite inducement, and conservative treatment was adopted. After 1 year, the bilateral femoral head was completely necrotic, and the normal anatomical morphology disappeared. The patient’s family described the fracture healing time as occurring before the age of 10 years old, with an average of 3 mo to achieve satisfactory results such as walking normally, after which the period of fracture healing was significantly prolonged, on average, up to 5-6 mo.
The authors conclude that, in cases with fractures after slight trauma, no sensitivity to pain and no sweat symptoms, the exact diagnosis is CIPA according to the results of a gene test. CIPA patients often have congenital and acquired joint deformities, Charcot disease, and easy-fracture characteristics. In this case, there were no obvious surgical mistakes, and after the operation, the left hip was well restored, no special drugs were administered, and the acetabular index recovered after the upper margin of the acetabulum, resulting in dislocation of the left hip after the operation. The postoperative absorption of the lateral acetabular margin may have been due to the high pressure on the top of the acetabulum caused by the femoral head; however, the characteristics of CIPA patients with dysplasia of bone and joint development should also be considered, and spontaneous dislocation of the right hip with no definite inducement was also considered. There was femoral head dislocation on both sides and necrotic absorption after 1-year period, which may be caused by defective blood transport caused by dislocation, but the patient’s family reported significantly slowed fracture healing. Thus, CIPA, with a likelihood of worsening skeletal symptoms, must also be considered.
In conclusion, reports of CIPA cases are relatively rare, and there is no standard treatment prescription. Whether these patients are prone to recurrent dislocation or femoral head resorption after hip dislocation surgery requires further study. This operation did not achieve the desired therapeutic effect in the present patient; therefore, in such unique cases, the development of the operation plan should take full account of the bone characteristics, joint development and deformity, employing strictly accurate operative indications. If the surgical indication is clear, full communication with the patients and their families is essential. Drug therapy and rehabilitation therapy can be used perioperatively to improve the bone and joint condition and to develop the most appropriate comprehensive treatment plan.
Reports of congenital insensitivity to pain with anhidrosis (CIPA) cases are few, and reports of CIPA patients with congenital dislocation of the hip are fewer. As a result, the operative risk and postoperative complications are unknown. In this article, we report a postoperative redislocation of the hip in a patient with CIPA and discuss the causes of the postoperative outcome.
CIPA.
CIPA.
Chiari pelvic osteotomy and proximal femoral rotation osteotomy.
This case shows possible postoperative complications of CIPA patients with congenital dislocation of the hip, which may play a guiding role in the future treatment. For such patients, we suggest that we pay more attention to the particularity of its joints and try comprehensive treatment. More research is needed to prove our conjecture.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: von Engelhardt LA S- Editor: Dou Y L- Editor: Wang TQ E- Editor: Song H
| 1. | Indo Y. NGF-dependent neurons and neurobiology of emotions and feelings: Lessons from congenital insensitivity to pain with anhidrosis. Neurosci Biobehav Rev. 2018;87:1-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Liu Z, Liu J, Liu G, Cao W, Liu S, Chen Y, Zuo Y, Chen W, Chen J, Zhang Y. Phenotypic heterogeneity of intellectual disability in patients with congenital insensitivity to pain with anhidrosis: A case report and literature review. J Int Med Res. 2018;46:2445-2457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Szöke G, Rényi-Vámos A, Bider MA. Osteoarticular manifestations of congenital insensitivity to pain with anhydrosis. Int Orthop. 1996;20:107-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 4. | Bar-On E, Weigl D, Parvari R, Katz K, Weitz R, Steinberg T. Congenital insensitivity to pain. Orthopaedic manifestations. J Bone Joint Surg Br. 2002;84:252-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Tomlinson J, O’Dowd D, Fernandes JA. Managing Developmental Dysplasia of the Hip. Indian J Pediatr. 2016;83:1275-1279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Ihme N, Altenhofen L, von Kries R, Niethard FU. Hip ultrasound screening in Germany. Results and comparison with other screening procedures. Orthopade. 2008;37:541-546, 548-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Cigala F, Lotito FM, Sadile F. Surgical treatment of late congenital dislocation of the hip (after 4 years of age). Hip Int. 2007;17 Suppl 5:S44-S50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Glorion C. Surgical reduction of congenital hip dislocation. Orthop Traumatol Surg Res. 2018;104:S147-S157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |