Published online Oct 26, 2018. doi: 10.12998/wjcc.v6.i12.542
Peer-review started: July 31, 2018
First decision: August 20, 2018
Revised: August 27, 2018
Accepted: August 28, 2018
Article in press: August 30, 2018
Published online: October 26, 2018
Processing time: 87 Days and 8.9 Hours
Advances in preoperative localization studies and demands for scarless surgery have promoted the investigation for remote techniques in parathyroid surgery. Transoral vestibular approach seems to provide the most comfortable and safest access to the neck. In this paper, we report our initial experience with robotic transoral vestibular parathyroidectomy (RTVP) in four patients with primary hyperparathyroidism. The surgery was performed with the Da Vinci system through three trocars introduced from the lower lip vestibule. The procedure was converted to open in two patients due to inappropriate preoperative localization. The mean operative time was 169 min. No postoperative complications were seen. Patients were discharged on postoperative day 1. RTVP is a feasible and safe technique, which allows better surgical exposure and manipulation of the instruments. The advantages of transoral vestibular approach can be enhanced by robotics. Further studies are needed to analyze complications and costs.
Core tip: In this paper we present the first national transoral parathyroidectomy cases and to our knowledge, these are the first transoral vestibular robotic parathyroidectomy cases without thyroidectomy. Our results indicate that correct preoperative localization and experience is essential for success in minimally invasive parathyroidectomy.
- Citation: Ozdenkaya Y, Ersavas C, Arslan NC. Robotic transoral vestibular parathyroidectomy: Two case reports and review of literature. World J Clin Cases 2018; 6(12): 542-547
- URL: https://www.wjgnet.com/2307-8960/full/v6/i12/542.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i12.542
Transverse neck incision is the standard in endocrine neck surgery. Despite satisfactory surgical outcome, surgeons have been searching for alternative approaches because the cosmetic results are disappointing, particularly in young female patients. Open minimally invasive parathyroidectomy was substituted for bilateral neck exploration with less complications and a smaller scar[1]. Nevertheless, demands for scarless surgery have prompted surgeons to continue to try alternative approaches. Several endoscopic or robotic techniques were described for thyroidectomy and/or parathyroidectomy including trans-axillary, trans-areolar and retroauricular approaches, however none of them have become widespread due to the necessity of extensive dissection, limitations in exposure, morbidities, and the presence of small but visible incisions[2-5]. The transoral approach, which allows better exposure to the surgical field, easy identification of recurrent laryngeal nerve (RLN), and comfortable extraction of the specimen has emerged to overcome these limitations[6]. Transoral parathyroidectomy was first described through the mouth floor but was not widely accepted due to complications and poor patient compliance[7-9]. Endoscopic transoral vestibular parathyroidectomy is a feasible and safe technique, which provides a direct approach to the glands with excellent cosmetic results[10-13].
Robotic endocrine neck surgery was initially introduced in South Korea[14]. Several reports suggested the safety and comfort of robotic endocrine neck surgery through axilla and/or breasts when compared with conventional laparoscopy[3,15,16]. Robotic transoral vestibular approach to the neck may combine the advantages of robotics and natural orifice surgery. There are two studies in the literature reporting robotic transoral vestibular parathyroidectomy (RTVP) including only four cases[17,18]. In this paper we present the first national transoral parathyroidectomy cases and to our knowledge, these are the first RTVP parathyroidectomy cases without thyroidectomy.
All cases underwent RTVP by a single surgeon in our institution between January and February 2018. Based on patients’ demands for scarless surgery, RTVP was discussed with the patients and written informed consent was received. Etiology was primary hypoparathyroidism (PHPT) in all patients. Details of the patient characteristics are given in Table 1.
| Case | Age | Sex | BMI(kg/m2) | Etiology | Preop. PTH (pq/mL) | Intraop. PTH(pq/mL) | Blood loss (mL) | Op. time (min) | Conversion to open | Hospital stay (d) | Final diagnose |
| 1 | 37 | F | 35.3 | PHPT | 161 | 6.9 | 50 | 205 | Yes | 1 | Right inferior parathyroid adenoma (15 mm × 10 mm × 8 mm) |
| 2 | 38 | M | 32.4 | PHPT | 97 | 21 | 40 | 196 | Yes | 1 | Left inferior parathyroid adenoma (18 mm × 12 mm × 10 mm) |
| 3 | 43 | F | 26.6 | PHPT | 815 | 33 | 20 | 162 | None | 1 | Left inferior parathyroid adenoma (32 mm × 13 mm × 7 mm) |
| 4 | 66 | F | 27.5 | PHPT | 281 | 70 | 20 | 176 | None | 1 | Left inferior parathyroid adenoma (18 mm × 12 mm × 10 mm) |
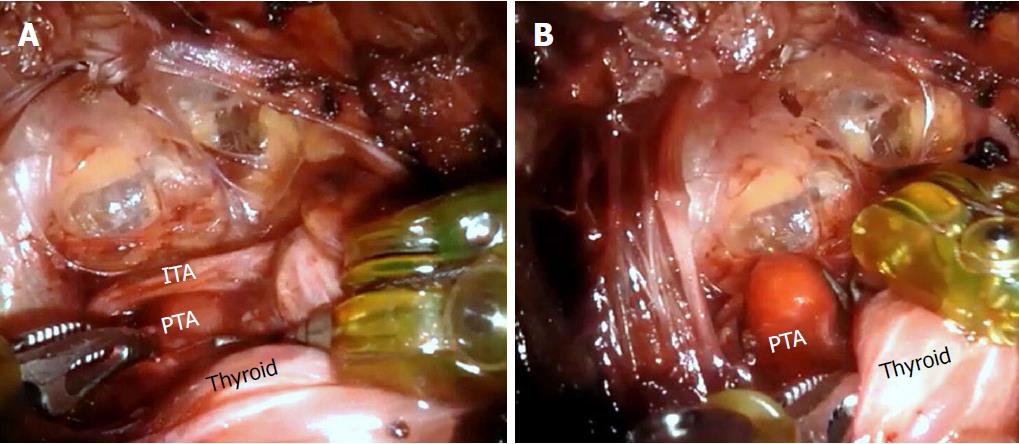
Patients were placed in supine position and intubated with nerve monitoring endotracheal tube. Intravenous antibiotic prophylaxis of 1 g of amoxicillin plus clavulanic acid was administered. Hyperextended neck position was adjusted. Skin and oral antisepsis were provided with chlorhexidine. The lower lip vestibule was incised at the center. Subcutaneous tissue was dissected bluntly until the mandible was reached. One to five hundred thousand epinephrine of 40 cc was injected to create a subplatysmal plane. The surgeon introduced a 12 mm central and two 5 mm lateral trocars and CO2 insufflation at 6 mmHg was started. Da Vinci Xi system (Intuitive Surgical, Sunnyvale, CA, United States) was docked. Blunt and sharp dissection with hook cautery was performed until reaching sternal notch in the inferior and sternocleidomastoids in the laterals. Strap muscles were lateralized and hanged to the skin with silk sutures. The related thyroid lobe was mobilized and enlarged parathyroid gland was removed using endoscopic dissector (Figure 1). The integrity of RLN was identified visually and by nerve monitoring during the surgery. The specimen was extracted through a midline incision (Figure 2). The success of the resection was confirmed with intraoperative quick parathyroid hormone (PTH) level decrease. The surgical site was irrigated, and incisions were closed with polyglactin sutures. A compression dressing was applied.
In patient 1 and patient 2, we converted to open surgery due to inconsistency between preoperative localization studies and intraoperative findings. Preoperative scintigraphy was negative in both patients. In patient 1, ultrasound indicated an enlarged left superior gland that was completely normal in intraoperative exploration. Similarly in patient 2, ultrasound reported an enlarged left superior gland. We kept exploring other glands, but the operative time and tissue dissection had been excessive. These were our first cases and the BMIs of both patients were over 30 kg/m2. Therefore, we decided to perform open neck exploration. We found a right inferior parathyroid adenoma in patient 1 and a left inferior parathyroid adenoma in patient 2. The success of both surgeries confirmed by quick PTH decrease. Intraoperative bleeding was insignificant (< 25 mL) in all cases.
All patients were discharged on postoperative day 1 after calcium and PTH levels were checked. Oral cephalexin (500 mg) twice a day was continued for five days. On postoperative day 7, patients were seen at an outpatient visit and vocal cords were examined by flexible laryngoscopy. The minimum follow-up was six months with a range between six and eight months. No postoperative complications were seen. Cosmetic satisfaction was excellent in the two patients whose surgery was completed endoscopically.
Developments in preoperative localization studies have enabled minimally invasive techniques in PHPT treatment. Considering a substantial number of these patients are young women, remote access to the neck without visible scars has been the focal point for surgeons. Several techniques such as transaxillary or inframammary approaches have been described, however it is difficult to qualify those as minimally invasive due to the requirement of extensive dissection[2,4]. A good minimally invasive technique should provide not only invisible or short incisions, but also a short distance between the incision and surgical site, which avoids excessive dissection and direct access to the surgical site. Instrumental collision should be minimum with a good operative exposure to safely identify important anatomical structures. For this purpose, transoral neck surgery has been described.
Witzel et al[6] and Karakas et al[7] reported the first experimental trials on fresh human cadavers and pigs through transoral sublingual approach. Karakas et al[7] published the first transoral sublingual parathyroidectomies in humans in 2010 and 2014[9]. Of the seven patients, two required a conversion to open surgery, two had transient hypoglossal nerve palsy, and one had transient RLN palsy. Since then, sublingual thyroid and/or parathyroid surgery have been studied but have not been popularized due to difficulty and complications[19].
The transoral vestibular approach to the neck was first described by Richmon et al[20] in a cadaveric study of two robotic thyroidectomies. They concluded that introducing the camera from the oral vestibule was more comfortable than sublingual approach and robotics might overcome the limitations of conventional endoscopic neck surgery. Further studies have been published on endoscopic transoral vestibular thyroidectomy using either a gasless technique or CO2 insufflation. The most common complication was persistent paresthesia of the chin skin (mental nerve injury)[21,22]. In 2016, Anuwong[11] published a transoral endoscopic vestibular thyroidectomy series of 60 cases. He reported no mental nerve injury. Two patients had transient hoarseness and a late postoperative hematoma. In another study, 46 patients who underwent transoral endoscopic vestibular thyroidectomy were compared with open thyroidectomy in Graves’ disease. Operative time was longer and pain was less in the endoscopic group, where other results were similar[23].
The conformation of transoral vestibular approach has been evolving parallel with thyroidectomy. In 2016, Udelsman et al[12] reported two transoral endoscopic vestibular parathyroidectomies without any complications. In 2017, Sasanakietkul et al[10] published the results of 12 transoral endoscopic vestibular parathyroidectomies. This group is extremely experienced in endoscopic neck surgery. The mean operative time was 107.5 min for PHPT patients in their study. They reported RLN injury in one patient, which resolved spontaneously in one month. No mental nerve injury or infections were seen. Recently, another report from India was published[13]. This study included 12 patients with PHPT who underwent transoral endoscopic vestibular parathyroidectomy. The mean operative time was 112 min and there were no postoperative complications. In our robotic procedures, the mean operative time was 169 min. The docking of the robot and preliminary learning curve are the reasons for this difference. In our cases, we did not have any complications.
Transoral vestibular approach seems to be the best option for remote access neck surgery. The feasibility and safety of the procedure have been shown in numerous studies. We believe that the superiority of this technique can be enhanced by robotics. Conventional endoscopy has well known limitations including interposition of the instruments, inadequate 2-dimensional exposure, unfavorable surgical comfort, and a long learning curve. Robotic transoral vestibular surgery provides a 3-dimentional magnified view through a direct access to the neck, which enables superior identification of important anatomical structures. Robotics also minimized the collision with articulated instruments and a stable platform. There are scarce data in the literature focused on robotic transoral vestibular approach. Russell et al[18] performed six robotic thyroid lobectomy, one with parathyroidectomy, through transoral vestibular access. Another case report of RTVP by Bearelly et al[17] described excision of an ectopic retropharyngeal parathyroid, but the approach was through the posterior pharynx. To our knowledge, our report presents the first pure RTVP cases[24]. Transoral vestibular approach can also provide convenience in neck dissection and surgery of thyroid malignancies, however there is no data about parathyroid malignancies in the literature[24,25]. The steps of the surgery should be well defined for patient safety before adoption of this technique[26]. A recent study comparing robotic and laparoscopic transoral vestibular approach revealed similar safety and feasibility but longer operative time for robotic surgery, which indicates the role of learning curve[27].
In our institution, we have performed robotic surgery for more than five years for procedures, including bariatric and adrenal procedures. The application of robotics to endocrine neck surgery just started in 2018. Out of four cases, we converted to open surgery in two, due to incorrect preoperative localization of the glands. The limited experience and extended operative time drove us to convert to open. Relatively high BMI of those patients might have been another contributing factor. We did not perform a cost analysis. Despite these limitations, we did not see any postoperative complications. Cosmetic results were excellent even in early postoperative period.
The transoral vestibular approach appears to be the future of minimally invasive parathyroidectomy. A robotic approach through the transoral vestibular access may overcome the limitations of initially described endoscopic transoral vestibular technique. The potential benefits of RTVP may theoretically decrease the incidence of postoperative complications. Further studies including wide series and cost analysis are needed.
The patients presented with asymptomatic hypercalcemia.
All the patients were diagnosed with parathyroid adenoma.
Neck ultrasound and parathyroid scintigraphy were performed to identify the etiology of primary hyperparathyroidism.
Calcium and parathormone levels were elevated and intraoperative decrease of parathormone was observed in all cases.
Single parathyroid adenoma was detected in all cases.
Diagnose of parathyroid adenoma was confirmed by postoperative histopathologic examination.
Robotic transoral vestibular parathyroidectomy was performed.
Udelsman R, Anuwong A, Oprea AD, Rhodes A, Prasad M, Sansone M, Brooks C, Donovan PI, Jannitto C, Carling T. Trans-oral Vestibular Endocrine Surgery: A New Technique in the United States. Ann Surg 2016; 264: e13-e16 [PMID: 27649533]
Robotic transoral vestibular approach is a safe and feasible method for well-located parathyroid adenomas.
CARE Checklist (2013) statement: The authors have read the CARE Checklist (2013), and the manuscript was prepared according to CARE checklist (2013).
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chen YK, Vieyra JP S- Editor: Ji FF L- Editor: Filipodia E- Editor: Tan WW
| 1. | Singh Ospina NM, Rodriguez-Gutierrez R, Maraka S, Espinosa de Ycaza AE, Jasim S, Castaneda-Guarderas A, Gionfriddo MR, Al Nofal A, Brito JP, Erwin P. Outcomes of Parathyroidectomy in Patients with Primary Hyperparathyroidism: A Systematic Review and Meta-analysis. World J Surg. 2016;40:2359-2377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 81] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 2. | Ikeda Y, Takami H, Niimi M, Kan S, Sasaki Y, Takayama J. Endoscopic thyroidectomy and parathyroidectomy by the axillary approach. A preliminary report. Surg Endosc. 2002;16:92-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 89] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Jackson NR, Yao L, Tufano RP, Kandil EH. Safety of robotic thyroidectomy approaches: meta-analysis and systematic review. Head Neck. 2014;36:137-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 110] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 4. | Choi JY, Lee KE, Chung KW, Kim SW, Choe JH, Koo do H, Kim SJ, Lee J, Chung YS, Oh SK. Endoscopic thyroidectomy via bilateral axillo-breast approach (BABA): review of 512 cases in a single institute. Surg Endosc. 2012;26:948-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 5. | Chung EJ, Park MW, Cho JG, Baek SK, Kwon SY, Woo JS, Jung KY. A prospective 1-year comparative study of endoscopic thyroidectomy via a retroauricular approach versus conventional open thyroidectomy at a single institution. Ann Surg Oncol. 2015;22:3014-3021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Witzel K, von Rahden BH, Kaminski C, Stein HJ. Transoral access for endoscopic thyroid resection. Surg Endosc. 2008;22:1871-1875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 195] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 7. | Karakas E, Steinfeldt T, Gockel A, Schlosshauer T, Dietz C, Jäger J, Westermann R, Sommer F, Richard HR, Exner C. Transoral thyroid and parathyroid surgery--development of a new transoral technique. Surgery. 2011;150:108-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Karakas E, Steinfeldt T, Gockel A, Westermann R, Bartsch DK. Transoral parathyroid surgery--feasible! Surg Endosc. 2011;25:1703-1705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Karakas E, Steinfeldt T, Gockel A, Mangalo A, Sesterhenn A, Bartsch DK. Transoral parathyroid surgery--a new alternative or nonsense? Langenbecks Arch Surg. 2014;399:741-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 10. | Sasanakietkul T, Jitpratoom P, Anuwong A. Transoral endoscopic parathyroidectomy vestibular approach: a novel scarless parathyroid surgery. Surg Endosc. 2017;31:3755-3763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 11. | Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg. 2016;40:491-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 344] [Article Influence: 38.2] [Reference Citation Analysis (0)] |
| 12. | Udelsman R, Anuwong A, Oprea AD, Rhodes A, Prasad M, Sansone M, Brooks C, Donovan PI, Jannitto C, Carling T. Trans-oral Vestibular Endocrine Surgery: A New Technique in the United States. Ann Surg. 2016;264:e13-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 13. | Bhargav PRK, Sabaretnam M, Amar V, Devi NV. Applicability of transoral endoscopic parathyroidectomy through vestibular route for primary sporadic hyperparathyroidism: A South Indian experience. J Minim Access Surg. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Kang SW, Lee SC, Lee SH, Lee KY, Jeong JJ, Lee YS, Nam KH, Chang HS, Chung WY, Park CS. Robotic thyroid surgery using a gasless, transaxillary approach and the da Vinci S system: the operative outcomes of 338 consecutive patients. Surgery. 2009;146:1048-1055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 300] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 15. | Foley CS, Agcaoglu O, Siperstein AE, Berber E. Robotic transaxillary endocrine surgery: a comparison with conventional open technique. Surg Endosc. 2012;26:2259-2266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 16. | He Q, Zhu J, Zhuang D, Fan Z. Robotic total parathyroidectomy by the axillo-bilateral-breast approach for secondary hyperparathyroidism: a feasibility study. J Laparoendosc Adv Surg Tech A. 2015;25:311-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Bearelly S, Prendes BL, Wang SJ, Glastonbury C, Orloff LA. Transoral robotic-assisted surgical excision of a retropharyngeal parathyroid adenoma: a case report. Head Neck. 2015;37:E150-E152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Russell JO, Clark J, Noureldine SI, Anuwong A, Al Khadem MG, Yub Kim H, Dhillon VK, Dionigi G, Tufano RP, Richmon JD. Transoral thyroidectomy and parathyroidectomy - A North American series of robotic and endoscopic transoral approaches to the central neck. Oral Oncol. 2017;71:75-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 116] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 19. | Benhidjeb T, Witzel K, Stark M, Mann O. Transoral thyroid and parathyroid surgery: still experimental! Surg Endosc. 2011;25:2411-2413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Richmon JD, Pattani KM, Benhidjeb T, Tufano RP. Transoral robotic-assisted thyroidectomy: a preclinical feasibility study in 2 cadavers. Head Neck. 2011;33:330-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 32] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Nakajo A, Arima H, Hirata M, Mizoguchi T, Kijima Y, Mori S, Ishigami S, Ueno S, Yoshinaka H, Natsugoe S. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc. 2013;27:1105-1110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 140] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 22. | Wang C, Zhai H, Liu W, Li J, Yang J, Hu Y, Huang J, Yang W, Pan Y, Ding H. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery. 2014;155:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 125] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 23. | Jitpratoom P, Ketwong K, Sasanakietkul T, Anuwong A. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves’ disease: a comparison of surgical results with open thyroidectomy. Gland Surg. 2016;5:546-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 89] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 24. | Shan L, Liu J. A Systemic Review of Transoral Thyroidectomy. Surg Laparosc Endosc Percutan Tech. 2018;28:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 25. | Razavi CR, Fondong A, Tufano RP, Russell JO. Central neck dissection via the transoral approach. Ann Thyroid. 2017;2:pii: 11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Russell JO, Anuwong A, Dionigi G, Inabnet WB 3rd, Kim HY, Randolph G, Richmon JD, Tufano RP. Transoral Thyroid and Parathyroid Surgery Vestibular Approach: A Framework for Assessment and Safe Exploration. Thyroid. 2018;28:825-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 27. | Razavi CR, Khadem MGA, Fondong A, Clark JH, Richmon JD, Tufano RP, Russell JO. Early outcomes in transoral vestibular thyroidectomy: Robotic versus endoscopic techniques. Head Neck. 2018;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |