Published online Sep 16, 2017. doi: 10.12998/wjcc.v5.i9.360
Peer-review started: September 23, 2016
First decision: November 2, 2016
Revised: April 30, 2017
Accepted: June 6, 2017
Article in press: June 8, 2017
Published online: September 16, 2017
Processing time: 144 Days and 3.7 Hours
Mesenteric cysts are rare, benign gastrointestinal cystic lesions, which are often non-troublesome and present as an incidental radiological finding. However, surgery is often performed in the acute setting to remove lesions that are symptomatic. This report highlights the case of a large, symptomatic mesenteric cyst managed successfully with initial conservative measures followed by planned elective surgery. A 44-year-old female presented with a four-day history of generalised abdominal pain associated with distension, fever, diarrhoea and vomiting. Computer tomography revealed a large (21.7 cm × 11.8 cm × 14 cm) mesenteric cyst within the left abdomen cavity. She was admitted and treated conservatively with intravenous fluids and antibiotics for four days, which lead to complete symptom resolution. Follow-up at intervals of one and three months revealed no return of symptoms. An elective laparotomy and excision of the mesenteric cyst was then scheduled and performed safely at nine months after the initial presentation. Compared to acute surgery, acute conservative management followed by planned elective resection of a symptomatic mesenteric cyst may prove safer. The withholding of an immediate operation may potentially avoid unnecessary operative risk and should be considered in patients without obstructive and peritonitic symptoms. Our case demonstrated the safe use of initial conservative management followed by planned elective surgery of a mesenteric cyst found in the acute setting, which was symptomatic but was not obstructive or causing peritonitic symptoms.
Core tip: Mesenteric cysts are often asymptomatic and present as an incidental finding, and acute operative removal is usually performed on symptomatic cases. However for selected cases, an initial conservative approach followed by planned elective surgery can be opted for, particularly in the absence of peritonitis and bowel obstruction. A safer and planned elective procedure would reduce the risk of operative complications. Acute drainage of the cyst should also be avoided due to the high risk of recurrence and infection.
- Citation: Leung BC, Sankey R, Fronza M, Maatouk M. Conservative approach to the acute management of a large mesenteric cyst. World J Clin Cases 2017; 5(9): 360-363
- URL: https://www.wjgnet.com/2307-8960/full/v5/i9/360.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i9.360
Mesenteric cysts are rare, benign intra-abdominal cystic lesions of the gastrointestinal mesentery, with an incidence of 1/100000 in adults and 1/20000 in children, and a female to male ratio of 2:1, which commonly present in the second decade of life[1]. Lesions are most commonly located in the small bowel (66%) and large bowel (33%), with the ascending colon being most frequently affected, and rarely found in the descending colon, sigmoid colon and rectum. They only occasionally extend to the retroperitoneum[1]. The size of a cyst can vary from a few millimetres to 30cm in diameter, containing up to 2500 mL of fluid[2]. Mesenteric cysts are often asymptomatic and discovered as an incidental finding from radiological investigations, but may present with acute or chronic abdominal pain (55%-81%), palpable mass (44%-61%), distension (17%-61%), nausea and vomiting (45%), constipation (27%) and diarrhoea (6%)[1]. In severe cases, it can lead to bowel obstruction, obstructive uropathy, volvulus, and peritonitis usually from a haemorrhagic or infective cyst[3]. Surgical excision of the mesenteric cyst, with or without resection of any neighouring visceral organs is the common management approach in the acute setting, with marsupialisation reserved for cases that may require wide resection of adjacent organs, but the recurrence rate is high[4]. Drainage is no longer advised due to infection and recurrence risks[5].
This article highlights a case of a symptomatic mesenteric cyst found in the acute setting managed successfully by conservative measures without the need for acute surgical intervention. This has not been previously reported in the literature. We postulate that the conservative approach to mesenteric cysts in the acute setting followed by planned elective surgery for selected cases may prove to be a beneficial and safe approach.
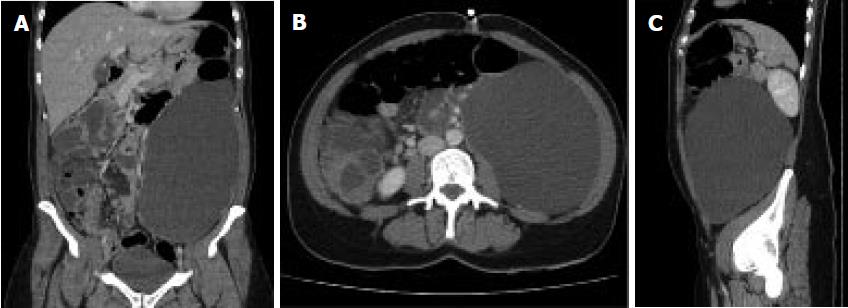
A 44-year-old female presented to our surgical assessment unit with a four-day history of generalised abdominal pain and distension, and associated fever, vomiting, diarrhoea and reduced oral intake. She did not have any symptoms of haematemesis, rectal bleeding and mucus discharge, or any urinary and gynecological symptoms. She had no significant past medical or surgical history. On examination she was haemodynamically stable with a pyrexia of 38-39 °C. Her abdomen was distended but soft, with tenderness over the epigastrium and right-side of the abdomen, with no obvious palpable masses or shifting dullness. Normal bowel sounds were present on auscultation. Rectal examination was normal. Routine blood tests were within normal limits aside from an elevated CRP (C-reactive protein) of 120. Blood cultures, urine-dip, urine pregnancy test, electrocardiography (ECG) and chest X-ray (CXR) was unremarkable. Contrast computed tomography (CT) revealed a huge thin-walled fluid collection with no abnormal enhancement and was separated from any visceral organs, measuring 21.7 cm (craniocaudal) × 11.8 cm (transverse) × 14 cm (antero-posterior) which was occupying the left side of abdomen and upper pelvis (Figure 1). No other abnormalities were found. The lesion was reported presumably as a mesenteric cyst with a suggested element of chronicity due to the calcified nature of the cyst wall.
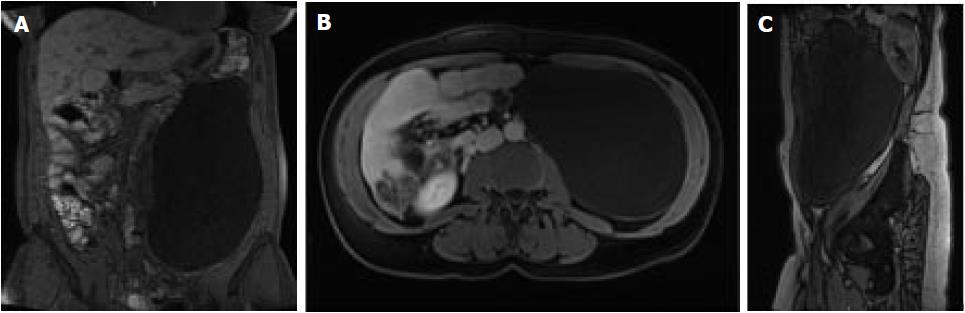
Initial management included intravenous fluids, analgesia, antiemetics and broad-spectrum antibiotics for symptom relief and suspected concurrent infective gastroenteritis. Explorative surgery was withheld in view of her improving clinical status and inflammatory markers when repeated hours later. She was admitted for four days and discharged with a course of oral antibiotics and no acute surgical intervention. One month after discharge, a pelvic magnetic resonance imaging scan was performed to investigate a possible retroperitoneal origin of the cyst. But the scan further confirmed the acute CT findings of a large simple left-side abdominal cyst (22 cm × 13 cm × 11.5 cm) extended superiorly to the inferior splenic margin which abutted the left kidney, it had no relation to any retroperitoneal structures, such as the ovaries or kidneys (Figure 2). Follow-up at one and three months revealed no worrying clinical features, and a subsequent decision for elective operation was made to excise the lesion. An elective laparotomy and excision of mesenteric cyst was performed at nine months after the initial presentation. There were no post-operative complications and follow-up at six weeks was unremarkable. Finally, histology of the excised lesion confirmed the diagnosis of a mesenteric cyst.
Mesenteric cysts are rare, benign intra-abdominal lesions found in the intestinal mesentery. The aetiology is unclear, but the most accepted theory to date describes a benign proliferation of ectopic mesenteric lymphatic tissue failing to communicate with the core lymphatic system[6]. In almost all reported cases, the management approach for a symptomatic mesenteric cyst is acute surgical resection, often performed laparoscopically, or in some cases using marsupialisation to avoid extensive bowel resection. Surgical drainage is avoided due to infection and recurrence[4,5]. The use of conservative management in the acute setting followed by elective surgery had not been previously reported.
Our case demonstrated the safety of conservative management for a symptomatic cyst in the acute setting without the need for immediate surgical intervention. This avoided any potential complications associated with acute surgery. Emergency surgery yields higher risks of complications, such as damage to surrounding structures, visceral perforation, intra-abdominal sepsis, and wound infection. Furthermore, the possibility of cyst regression may fundamentally avoid the need for any operation at all, which means potentially avoiding long-term postoperative complications, such as abdominal adhesions and herniations. However, such a conservative approach should only be reserved for stable patients without symptoms of bowel obstruction, ischaemic bowel, obstructive uropathy, volvulus, and peritonitis.
However by withholding surgery, the risk of adverse sequelae such as bowel obstruction or peritonitis from cyst rupture is inherent, but with limited literature evaluating the disease course of conservatively managed mesenteric cysts, this risk is difficult to quantify currently. A literature search reveals a case-series conducted on seventeen children, which stated the importance of early diagnosis and treatment to prevent significant complications[3]. Nevertheless, we believe that the decision to operate in the acute setting should only be considered if absolutely necessary. The calcified nature of the cyst wall in our case suggests an element of chronicity and stability of the lesion, possibly a process of chronic inflammation, which supports the decision of not operating immediately. Of particular note, the clinical finding of right-sided abdominal tenderness in our participant did not correlate with the left-sided mesenteric cyst finding, which serves to highlight the often subtle nature of mesenteric cyst presentation.
The uncomplicated nature of the elective laparotomy and excision of mesenteric cyst performed nine months after the initial acute presentation highlights the advantage of a delayed planned operation. A randomised controlled trial to compare the benefit of such an approach would be ethically challenging. Overall, the benefit of conservative management in the acute setting avoids an unplanned operation, which may have significant operative and postoperative complications.
In conclusion, This case report aims to provide future clinicians with the confidence to manage large uncomplicated mesenteric cysts conservatively in the acute setting, thus avoiding the need for an emergency operation that potentially yields a higher risk of peri and post-operative complications compared to a planned operation. The decision to manage conservatively compared to surgically in the acute setting should be considered on an individual basis. Undoubtedly, the definitive treatment is the excision of the mesenteric cyst, but a planned elective surgical approach may be significantly safer than an emergency one.
A 44-year-old female with no significant medical history presented with a four-day history of generalised abdominal pain associated with distension, fever, diarrhoea and vomiting.
Abdomen was distended but soft, with tenderness over the epigastrium and right-sided region, with no palpable mass or shifting dullness, and bowel sounds on auscultation was normal.
Omental cyst, pancreatic or non-pancreatic pseudocyst, echinococcal cyst, enteric duplication cyst, cystic mesothelioma, and ovarian cyst, as well as ascites and lymphoma.
All blood tests were within normal limits aside from a raise C-reactive protein (CRP) of 120, and blood cultures, urine-dip, pregnancy test and electrocardiography (ECG) were unremarkable.
Contrast computed tomography showed a huge thin-walled intra-abdominal fluid collection measuring 21.7 cm × 11.8 cm × 14 cm occupying the left side of abdomen and upper pelvis, suggestive of a mesenteric cyst.
Histological confirmation of mesenteric cyst after elective excision.
Initial conservative management with fluid support in the acute setting, followed by elective surgical excision of lesion.
Surgical excision of the mesenteric cyst, with or without resection of neighouring organs, was the most common approach in the acute setting. Marsupialisation was reserved for cases that may require wide resection of adjacent organs, but the recurrence rate is high. Drainage is no longer advised due to infection and recurrence risks.
Mesenteric cysts are rare, benign gastrointestinal cystic lesions, which are often non-troublesome and present as an incidental radiological finding.
Initial conservative approach to mesenteric cysts with a planned elective surgical excision should be adopted in selected cases, such as in the absence of peritonitis and bowel obstruction.
This article is interesting and informative on a sensible topic, and the clinical problem is clearly presented in following parts of the article.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hermann J, Miliaras S, Niu CY, Zeiler M S-Editor: Kong JX L-Editor: A E-Editor: Zhao LM
| 1. | Liew SC, Glenn DC, Storey DW. Mesenteric cyst. Aust N Z J Surg. 1994;64:741-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Aydinli B, Yildirgan MI, Kantarci M, Atamanalp SS, Basoglu M, Ozturk G, Onbas O, Oren D. Giant mesenteric cyst. Dig Dis Sci. 2006;51:1380-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Prakash A, Agrawal A, Gupta RK, Sanghvi B, Parelkar S. Early management of mesenteric cyst prevents catastrophes: a single centre analysis of 17 cases. Afr J Paediatr Surg. 2010;7:140-143. [RCA] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Kurtz RJ, Heimann TM, Holt J, Beck AR. Mesenteric and retroperitoneal cysts. Ann Surg. 1986;203:109-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 203] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 5. | Vu JH, Thomas EL, Spencer DD. Laparoscopic management of mesenteric cyst. Am Surg. 1999;65:264-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 6. | Richard R. Mesenteric and omental cysts, 6th ed, Pediatric Surgery. Grosfeld JL, O’Neill JA Jr, Coran AG Jr, Fonkalsrud EW, editors. Philadelphia: Mosby Elsevier 2006; 1399-1406. |