Published online Jul 16, 2017. doi: 10.12998/wjcc.v5.i7.292
Peer-review started: September 28, 2016
First decision: November 10, 2016
Revised: March 8, 2017
Accepted: March 16, 2017
Article in press: March 17, 2017
Published online: July 16, 2017
Processing time: 289 Days and 12.3 Hours
Dural sinus thrombosis following a head trauma is a rare condition, described in literature along with the lack of consensus regarding diagnosis and management. We present a case of a fifty-year-old man with a head injury and combined supratentorial-subtentorial epidural hematoma who was treated conservatively through the administration of low molecular weight heparin. The diagnosis and management of this condition are discussed based on a literature review. The early diagnosis may prevent potentially treatable poor outcomes.
Core tip: Dural sinus thrombosis (DST) is a rare although serious clinicopathological entity that causes approximately 0.5% of all stroke cases. Head trauma may be identified as a possible cause of DST. The lack of consensus regarding the most appropriate therapeutic strategy prompted us to describe this unusual case of transverse sinus thrombosis caused by a combined supra-subtentorial haematoma. The absence of symptoms of the patient convinced us to assume a conservative behaviour which consisted in the administration of low molecular weight heparin after the computed tomography scan had documented the stability of the extradural collection. Our strategy leads to the recanalization of the sinus.
- Citation: Pescatori L, Tropeano MP, Mancarella C, Prizio E, Santoro G, Domenicucci M. Post traumatic dural sinus thrombosis following epidural hematoma: Literature review and case report. World J Clin Cases 2017; 5(7): 292-298
- URL: https://www.wjgnet.com/2307-8960/full/v5/i7/292.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i7.292
Dural sinus thrombosis (DST) is a rare although serious clinicopathological entity that causes approximately 0.5% of all stroke cases[1]. Superior sagittal sinus as well as transverse sinus are more affected than other dural sinuses[1]. Head trauma may be identified as a possible cause of DST. In particular, depressed skull fractures occurring at the site of the dural sinuses as well as epidural or subdural hematoma have been found to be associated with DST[2-6]. Here we describe the case of a man who reported the occlusion of the transverse sinus as the consequence of the development of a combined supratentorial-subtentorial epidural hematoma. The patient was treated conservatively through the administration of low molecular weight heparin (LMWH). We discuss the physiopathologycal hypothesis, the clinic-radiological aspects as well as the management options reviewing the literature.
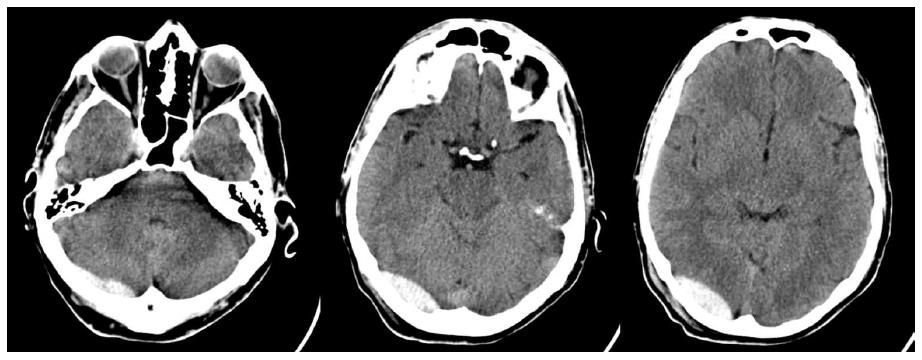
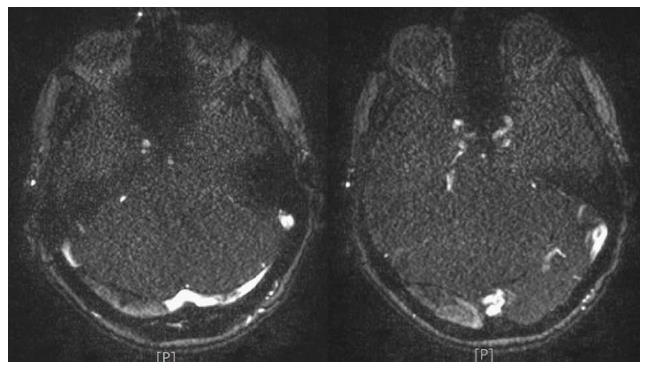
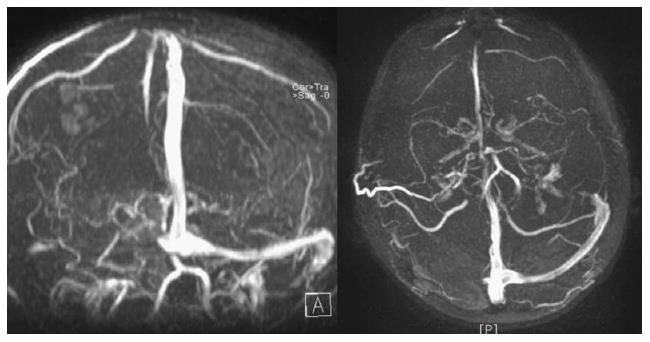
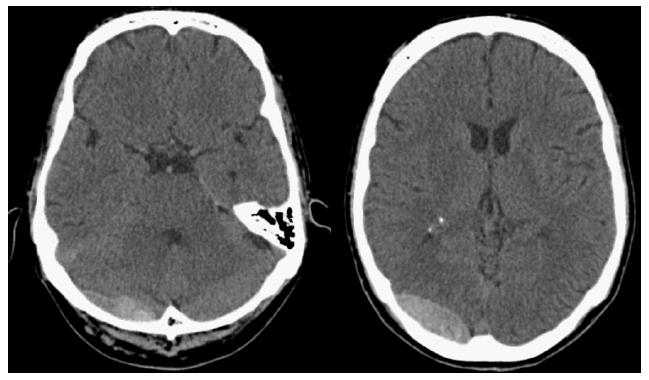
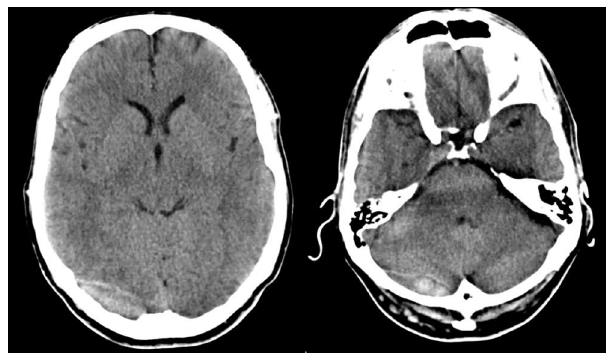
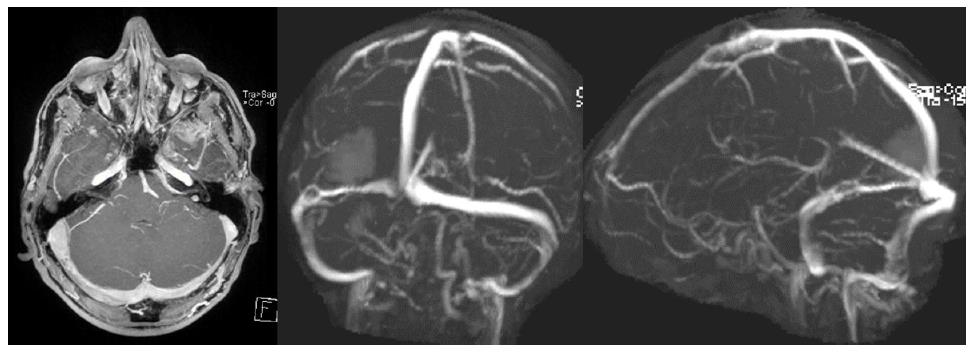
This is the case of a fifty-year-old man who was hospitalized after being involved in a car accident in which he reported a concussive head trauma. Except for the trauma he did not have a significant history of illness. The patient was subjected to a brain computed tomography (CT) scan which showed the presence of a combined right supra-subtentorial hematoma (Figure 1). Clinical evaluation of the patient did not reveal any neurological signs except for a mild headache. Because of the site of the hematoma, an involvement of the transverse sinus was suspected. As a consequence a brain magnetic resonance imaging (MRI) with arterial and venous reconstruction was performed. The MRI confirmed the presence of the hematoma involving the supratentorial and the subtentorial compartment. Furthermore the venous study did not show any appreciable signal of blood flow within the right transverse sinus. This radiological finding was likely to be due to the occlusion of the sinus (Figures 2 and 3). Because of the absence of neurological signs as well as the patency of the contralateral dural sinuses system, a conservative management was adopted. A CT scan performed 48 h after the accident showed a slight increase in the size of the hematoma (Figure 4). As a consequence, administration of LMWH was delayed. By the 10th post-traumatic day two more brain CT scan had been performed which had shown the progressive decrease in the size of the hematoma (Figure 5). This reduction encouraged us to begin the administration of LMWH. On 15th post-traumatic day the patient was discharged at home. During the subsequent 23 d the patient did not experience any symptoms related to the trauma. On 24th post-traumatic day, he began to complain of mild headache, vertigo and nausea. Since the symptoms were not responsive to oral analgesics and antiemetic drugs, the patient came back to the Emergency Department of our Hospital. A new brain CT scan was performed. It showed a further reduction of the size of both hematomas. Given the clinical history, a new brain MRIs can with venous angiographic reconstruction was performed. The new MRI confirmed the further decrease in the size of the epidural hematomas. Angiographic reconstructions of the dural sinuses showed that, although characterized by a less intensity in comparison with the contralateral sinus, the blood flow signal within the previously occluded transverse sinus was now visible. These radiological findings were likely to be due to the partial recanalization of the sinus (Figure 6). Symptoms progressively disappeared and after a brief period of hospitalization the patient was discharged at home.
DST is a rare although serious clinicopathological entity that causes approximately 0.5% of all stroke cases. The signs and symptoms are extremely varied and non specific. Cerebral sinus thrombus formation due to head injury has been postulated to be caused by a sinus endothelial injury, thrombus extension from scalp abrasions, or damage to the emissary veins[7]. Sinus thrombosis can often occur with thrombosis of the cerebral veins, leading to cytotoxic and vasogenic edema[8]. The sinus thrombi lead directly to the decreased absorption of cerebrospinal fluid because of the increased sinus venous pressure, resulting in intracranial hypertension. Patients with cerebral sinus thrombosis most often present with severe headache that can be gradual or acute in nature. Patients can also have symptoms of increased intracranial pressure, including nausea and vomiting. Some patients have seizures. In 1946, Ecker described the first case of head injury associated with DST. Since then, other trauma-induced DSTs have been reported in cases of head injuries[5,9,10]. Ochagavia announced that the incidence of DST was 4% after penetrating head trauma[10]. However, Stiefel et al[11] reported that he found DST with an incidence of 6.8% in the pediatric age group. There are two series on post traumatic DST in children but sporadic case reports in adults and in children have been published[4,6,12-25]. Overall, there are 32 cases including 22 children and 10 adults (Table 1). The higher number of children can be explained by the fact that the venous collateral system is not completely mature in their cerebrum. In only 3 cases (1 adult and 2 children) there was an epidural hematoma (EH). It was always associated with skull fracture. Our case is the first case reported, to our knowledge, in which the epidural hematoma was not associated to skull fracture and had a supra and subtentorial localization. In our case, although it is difficult to establish if the occlusion of the sinus was owed to the extrinsic compression of the hematoma on the sinus wall or to the development of a thrombus within the sinus, it is possible that both the phenomenon contributed to the occlusion through a cause-effect process. The extrinsic compression of the hematoma probably caused a deceleration of the blood flow within the sinus. As a consequence, according to the principles of blood stasis, modifications of the vascular wall and blood rheology enunciated by Virchow, it is likely that a thrombus within the transverse sinus developed. The initial imaging study in the evaluation of patients with possible DST is usually a brain CT scan. Magnetic resonance imaging, as well as MR angiography and venography, provide us with the most sensitive tools for detecting DST. The combination of these imaging modalities constitutes the study of choice in the diagnosis of DST. In fact the images shown by our MRI are compatible with an occlusion of the transverse sinus. There is no consensus on the overall treatment concerning surgical, radiosurgical, endovascular or conservative treatment. Identification and treatment of the underlying causes should represent the first step in the treatment of dural sinus occlusion. In case of extrinsic compression such as depressed skull fractures as well as epidural or subdural hematoma surgical removal of the identified source of compression has been advocated by several authors[12,14], even if only 1 case of post-traumatic DST related to EH, reported in literature, was underwent to surgical treatment[26]. In our case, despite the presence of the epidural hematoma without mass effect as well as the occlusion of the sinus, the complete absence of neurological symptoms encouraged us to adopt a conservative behaviour. Despite the role of antithrombotic therapy has been widely examined and several studies have been published in this sense, its use in post-traumatic DST still remain controversial, because of increased risk for venous hemorrhagic infarction[26]. A meta-analysis conducted by Coutinho et al[27] which included 2 randomized controlled studies investigating the role of unfractionated heparin as well as LMWH, concluded that the anticoagulant treatment can be considered safe and is associated with a better overall outcome in patients affected with DST. The EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients conducted by Einhäupl et al[28] in 2010 concludes that patients with cerebral sinus thrombosis without contraindications for anticoagulant should be treated either with body weight-adjusted subcutaneous LMWH or with dose adjusted intravenous heparin. In addition the study concluded that the use of LMWH should be considered safe despite the presence of intracranial haemorrhage. Although conscious of current literature, we decided to postpone the administration of subcutaneous LMWH because of the growth of the epidural hematoma that had been shown by a control CT scan performed 48 h after trauma. Once seriated CT scan demonstrated the progressive reduction in the size of the hematoma subcutaneous LMWH heparin was administered and continued after discharge. LMWH pharmacologically doesn’t possess thrombolytic action; given this the main purpose of their administration is to prevent recurrent thrombosis and appositional thrombus growth. Data collected from different studies confirm that DST patients display a high spontaneous and intrinsic thrombolytic potential, with recanalization rates of 60% during the first 20 d as happened in our case. Thereafter, recanalization rates increase insignificantly[26]. The second MRI with angiographic and venous reconstruction performed during the second hospitalization showed that the blood flow within the transverse sinus had reappeared. The administration of LMWH as well as the progressive reabsorption of the epidural hematoma are related to the recanalization of the transverse sinus. The consequent reorganization of the venous blood flow within the dural sinus system was may explain the physiopathology of the posterior cranial fossa symptoms characterized by vertigo and headache.
| Ref. | Age, sex | Symptom | Skull fracture | Intracranial lesion | Treatment | Follow-up |
| Hesselbrock et al[8] | 44, M | IICPS, seizure | ? | Contusion | Supportive | Unknown |
| Taha et al[22] | 5 (3M/2F) children | Various | 3 cases | Contusion | Supportive | 4 RC 1 no RC |
| Ochagavia et al[10] | 27, M | Herniation due to IICPS | - | Edema | - | dead |
| Ferrera et al[17] | 24, M | IICPS | + | Venous infarct | Surgery | Unknown |
| Stiefel et al[11] | 8 (5F/3M) children | IICPS | All cases | - | - | 6 RC 1 no RC 1 dead |
| Meena et al[9] | 40, M | IICPS, seizure, hemiparesi | - | - | AC | Unknown |
| Satoh et al[21] | 2, F | IICPS | - | - | Supportive | RC |
| Brors et al[13] | 32, M | Cranial nerve palsy | + | Contusion | AC | RC |
| Erdogan et al[16] | 1, M | IICPS | - | Venous infarct, SH | Supportive | Unknown |
| Owler et al[4] | 18, M | IICPS, hemiparesi | - | Venous infarct | Supportive, surgery | Unknown |
| Sousa et al[19] | 7, F | IICPS | - | - | supportive | Unknown |
| Muthukumar et al[25] | 7, F | IICPS | + | - | AC | Unknown |
| Saad et al[20] | 10, F | IICPS | - | - | AC | Unknown |
| Yuen et al[23] | 4, F | IICPS | + | - | Supportive | RC |
| Dalgiç et al[15] | 35, M | IICPS | - | - | AC | RC |
| 25, M | Facial palsy | + | EH | AC | No RC | |
| Caplan et al[14] | 27, M | IICPS, paraesthesias | + | Contusion | AC | Unknown |
| Bakar et al[12] | 18, M | IICPS | + | Edema | Surgery | Unknown |
| Beer-Furlan et al[26] | 3, M | IICPS | + | EH | Surgery | Dead |
| Lebowitz et al[18] | 6, M | IICPS | - | SH | AC | No RC |
| Yun et al[24] | 10, M | IICPS | + | EH | Supportive | RC |
| Our case | 50, M | IICPS | - | EH | Supportive, AC | RC |
DST is a rare although serious condition described in literature along with a lack of consensus regarding diagnosis and management. Most reports show good outcome and recovery, but DST might be related to a poor recovery and even lead to death. DST may be caused by post-traumatic depressed skull fractures or intracerebral hematomas compressing the sinus wall and altering the blood flow within the sinus until thrombosis, so additional diagnostic investigations should be performed in terms of DST in head trauma cases that have other risk factors. The administration of anticoagulant therapy still remains controversial but in association with the progressive reabsorption of the hematoma it could allow the recanalization of the dural sinus.
A fifty-year-old man was hospitalized after being involved in a car accident in which he reported a concussive head trauma.
Except for a mild headache, the patient didn’t show neurological signs.
Haemorrhage, concussion injury, cerebral contusion.
All labs were within normal limits.
Computed tomography (CT) scan showed the presence of a combined right supra-subtentorial hematoma, while the magnetic resonance imaging scan showed the occlusion of the transverse sinus.
Once seriated CT scan demonstrated the progressive reduction in the size of the hematoma subcutaneous heparin or low molecular weight heparin was administered and continued after discharge.
Dural sinus thrombosis (DST) following a head trauma is a rare condition, described in literature along with the lack of consensus regarding diagnosis and management.
Dural venous sinus thrombosis is a subset of cerebral venous thrombosis. It is the presence of a blood clot in the dural venous sinuses that causes approximately 0.5% of all stroke cases. The symptoms depend mainly on which sinus is involved.
In case of head trauma the DST should always be considered. This entity is often underestimated. Recognizing this condition can prevent misdiagnosis and suggest the best treatment option. The administration of anticoagulant therapy could allow the recanalization of the dural sinus.
This is a rare and interesting case, which could highlight a differential diagnosis for clinical doctors.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Byrd SE, Leonardi MA, Liu JL, Yoshida S S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Filippidis A, Kapsalaki E, Patramani G, Fountas KN. Cerebral venous sinus thrombosis: review of the demographics, pathophysiology, current diagnosis, and treatment. Neurosurg Focus. 2009;27:E3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Kinal ME. Traumatic thrombosis of dural venous sinuses in closed head injuries. J Neurosurg. 1967;27:142Y145. |
| 3. | Meltzer H, LoSasso B, Sobo EJ. Depressed occipital skull fracture with associated sagittal sinus occlusion. J Trauma. 2000;49:981. [PubMed] |
| 4. | Owler BK, Besser M. Extradural hematoma causing venous sinus obstruction and pseudotumor cerebri syndrome. Childs Nerv Syst. 2005;21:262-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Tamimi A, Abu-Elrub M, Shudifat A, Saleh Q, Kharazi K, Tamimi I. Superior sagittal sinus thrombosis associated with raised intracranial pressure in closed head injury with depressed skull fracture. Pediatr Neurosurg. 2005;41:237-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Uzan M, Ciplak N, Dashti SG, Bozkus H, Erdincler P, Akman C. Depressed skull fracture overlying superior sagittal sinus as a cause of benign intracranial hypertension: Case report. J Neurosurg. 1998;88:598-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005;352:1791-1798. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 959] [Cited by in RCA: 875] [Article Influence: 43.8] [Reference Citation Analysis (0)] |
| 8. | Hesselbrock R, Sawaya R, Tomsick T, Wadhwa S. Superior sagittal sinus thrombosis after closed head injury. Neurosurgery. 1985;16:825-828. [PubMed] |
| 9. | Meena AK, Jayalaxmi SS, Murthy JM. Cortical sinovenous thrombosis following closed head injury. Neurol India. 2000;48:195-196. [PubMed] |
| 10. | Ochagavia AR, Boque MC, Torre C, Alonso S, Sirvent JJ. Dural venous sinus thrombosis due to cranial trauma. Lancet. 1996;347:1564. [PubMed] |
| 11. | Stiefel D, Eich G, Sacher P. Posttraumatic dural sinus thrombosis in children. Eur J Pediatr Surg. 2000;10:41-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 40] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Bakar B, Tekkök IH. Venous sinus thrombosis after closed head injury: case report. Ulus Travma Acil Cerrahi Derg. 2010;16:98-102. [PubMed] |
| 13. | Brors D, Schäfers M, Schick B, Dazert S, Draf W, Kahle G. Sigmoid and transverse sinus thrombosis after closed head injury presenting with unilateral hearing loss. Neuroradiology. 2001;43:144-146. [PubMed] |
| 14. | Caplan JM, Khalpey Z, Gates J. Closed traumatic head injury: dural sinus and internal jugular vein thrombosis. Emerg Med J. 2008;25:777-778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Dalgiç A, Seçer M, Ergüngör F, Okay O, Akdağ R, Ciliz D. Dural sinus thrombosis following head injury: report of two cases and review of the literature. Turk Neurosurg. 2008;18:70-77. [PubMed] |
| 16. | Erdogan B, Caner H, Aydin MV, Yildirim T, Kahveci S, Sen O. Hemispheric cerebrovascular venous thrombosis due to closed head injury. Childs Nerv Syst. 2004;20:239-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 17. | Ferrera PC, Pauze DR, Chan L. Sagittal sinus thrombosis after closed head injury. Am J Emerg Med. 1998;16:382-385. [PubMed] |
| 18. | Lebowitz DC, Ko MW, Cameron EK, Ko PY. Cerebral sinus thrombosis in a 6-year-old boy after a minor head injury. Pediatr Emerg Care. 2014;30:177-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Sousa J, O’Brien D, Bartlett R, Vaz J. Sigmoid sinus thrombosis in a child after closed head injury. Br J Neurosurg. 2004;18:187-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Saad DF, Crawford GI, Wulkan ML. Cerebral venous thrombosis after closed head injury in a child. J Trauma. 2005;58:1066-1067. [PubMed] |
| 21. | Satoh H, Kumano K, Ogami R, Nishi T, Onda J, Nishimura S, Kurisu K. Sigmoid sinus thrombosis after mild closed head injury in an infant: diagnosis by magnetic resonance imaging in the acute phase--case report. Neurol Med Chir (Tokyo). 2000;40:361-365. [PubMed] |
| 22. | Taha JM, Crone KR, Berger TS, Becket WW, Prenger EC. Sigmoid sinus thrombosis after closed head injury in children. Neurosurgery. 1993;32:541-545; discussion 545-546. [PubMed] |
| 23. | Yuen HW, Gan BK, Seow WT, Tan HK. Dural sinus thrombosis after minor head injury in a child. Ann Acad Med Singapore. 2005;34:639-641. [PubMed] |
| 24. | Yun JH, Ko JH, Lee MJ. Early Spontaneous Recanalization of Sigmoid Sinus Thrombosis Following a Closed Head Injury in a Pediatric Patient: A Case Report and Review of Literature. J Korean Neurosurg Soc. 2015;58:150-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 25. | Muthukumar N. Cerebral venous sinus thrombosis and thrombophilia presenting as pseudo-tumour syndrome following mild head injury. J Clin Neurosci. 2004;11:924-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Beer-Furlan A, de Almeida CC, Noleto G, Paiva W, Ferreira AA, Teixeira MJ. Dural sinus and internal jugular vein thrombosis complicating a blunt head injury in a pediatric patient. Childs Nerv Syst. 2013;29:1231-1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 27. | Coutinho JM, Ferro JM, Canhão P, Barinagarrementeria F, Bousser MG, Stam J; ISCVT Investigators. Unfractionated or low-molecular weight heparin for the treatment of cerebral venous thrombosis. Stroke. 2010;41:2575-2580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 115] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 28. | Einhäupl K, Stam J, Bousser MG, De Bruijn SF, Ferro JM, Martinelli I, Masuhr F; European Federation of Neurological Societies. EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol. 2010;17:1229-1235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 316] [Article Influence: 22.6] [Reference Citation Analysis (0)] |