Published online Jun 16, 2017. doi: 10.12998/wjcc.v5.i6.254
Peer-review started: September 23, 2016
First decision: November 21, 2016
Revised: March 9, 2017
Accepted: March 21, 2017
Article in press: March 22, 2017
Published online: June 16, 2017
Processing time: 265 Days and 1.9 Hours
Intussusception is rarely observed in adults. Adult cases account for only 5% of all cases of intussusceptions and almost 1%-5% of bowel obstruction cases. The etiology, presentation and management of intussusception in adults are different from those in children. The clinical presentation in adults often includes nonspecific signs and symptoms, thereby complicating differential diagnosis from other causes of abdominal pain. We report a 29-year-old Asian woman who visited our emergency department with complaints of fever associated with epigastric pain since one day. Abdominal computed tomography demonstrated ileocolic intussusception, and laparoscopic small bowel luminal mass resection was performed. Histopathology report confirmed a 3.5 cm × 2.7 cm submucosal lipoma in the terminal ileum. Sufficient vigilance and appropriate investigations are important for prompt diagnosis and surgical referral of patients to enable favorable outcomes. A computed tomography scan can be a helpful modality in establishing a diagnosis.
Core tip: Intussusception is rarely observed in adult patients. Adult clinical presentation is non-specific. A 29-year-old Asian female patient presented with a fever and abdominal pain. Abdominal computed tomography demonstrated ileocolic intussusception. A computed tomography scan can help diagnose ileocolic intussusception. Ileocolic intussusception should be considered as an infrequent cause of acute abdominal pain in adults.
- Citation: Lee DE, Choe JY. Ileocolic intussusception caused by a lipoma in an adult. World J Clin Cases 2017; 5(6): 254-257
- URL: https://www.wjgnet.com/2307-8960/full/v5/i6/254.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i6.254
Intussusception of the bowel is defined as a condition in which a proximal bowel segment (intussusceptum) invaginates into an adjacent distal segment (intussuscipiens), thereby causing bowel obstruction[1]. Intussusception is a rare cause of abdominal pain in the adult population, accounting for only 1%-5% of all cases of intestinal obstructions and 5% of all cases of intussusception[2-4]. The clinical presentation in adults often includes nonspecific signs and symptoms, thereby complicating the differential diagnosis from other causes of abdominal pain. With early diagnosis, appropriate treatment including surgery can be performed. This has resulted in the mortality rate from intussusception being less than 1%[5]. We present a case of a 29-year-old Asian woman with ileocolic intussusception caused by a lipoma and resected by laparoscopy-assisted surgery.
A 29-year-old Asian woman was admitted to our emergency department (ED) with complaints of epigastric pain, nausea, fever and a chill that persisted for one day. One day previously, she presented to a regional emergency center with nausea, fever and a chill. She was diagnosed with viral enterocolitis and treated by intravenous hydration and antipyretics. Her symptoms progressively worsened despite consuming analgesics and she was admitted to our ED. She denied any history of diarrhea, melena, hematochezia, weight gain or loss and bowel habit change.
Her past medical history included gastric polypectomy in the previous year and a 3-cm lipoma in the colon, which was incidentally detected using colonoscopy. She was a non-smoker and denied alcohol use. In the ED, her blood pressure was 115/76 mmHg, her heart rate was 109 beats/min and her axillary temperature was 36.9 °C. A physical examination revealed diffuse tenderness upon palpation, particularly in the epigastric area and right lower quadrant and normoactive bowel sounds. The other examination results were normal.
Initial laboratory data were significant for a white cell count of 11.34 × 109/L, with 93.7% neutrophils. The C-reactive protein (CRP) level was elevated at 8.21 mg/L (ref. < 0.5 mg/dL). The results of other blood tests and urine analysis were within normal ranges.
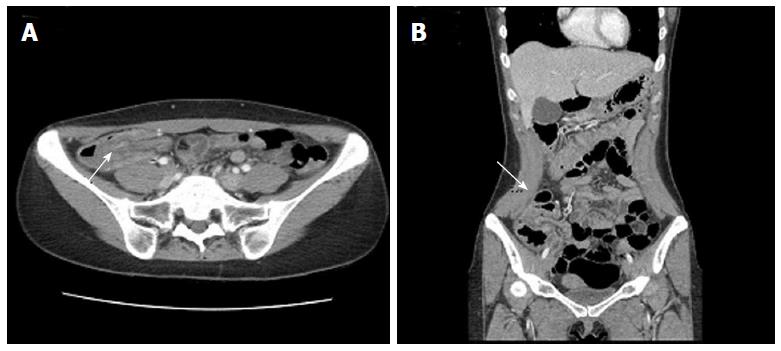
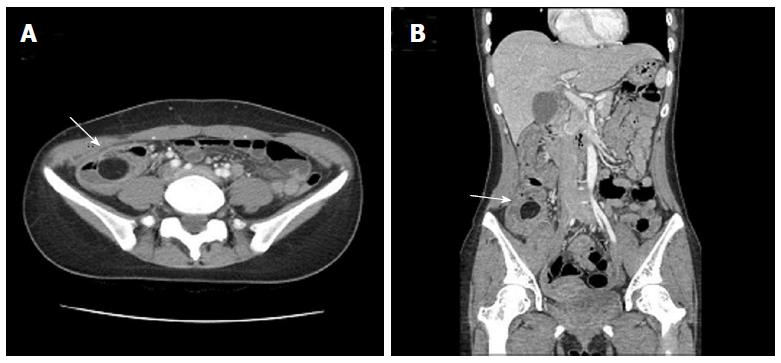
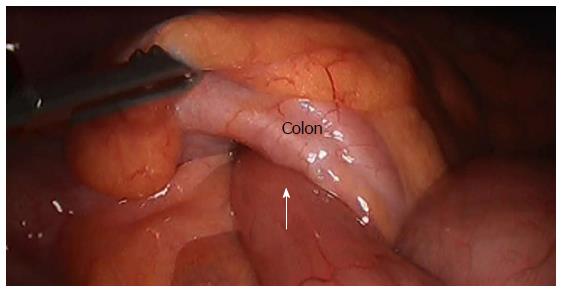
Plain abdominal radiography was performed and did not show signs of obstruction or perforation. A contrast-enhanced abdomen and pelvis computed tomography (CT) scan was performed, which revealed diffuse edematous wall thickening of the ascending and transverse colon, and the entrance of the ileal segment of the small intestines into the colon, thereby indicating ileocolic intussusception (Figure 1). The leading structure was a 27-mm fatty dense structure within the bowel lumen that was separate from the mesentery (Figure 2). The general surgery team was consulted and the patient underwent laparoscopic small bowel luminal mass resection on the third day following admission, which revealed intussusception for the ileum to the colon (Figure 3). The mass was located in the proximal 5 cm of the ileocecal valve and the surgeon found it on palpation during surgery. The histopathology report confirmed a 3.5 cm × 2.7 cm submucosal lipoma in the terminal ileum. The patient was discharged on the fifth postoperative day without complications. One week later, she visited the outpatient department and didn’t complain any symptoms.
Intussusception is common in children and mainly in those under the age of three. Overall, the male-to-female ratio is approximately 3:1. With advancing age, the sexual difference becomes marked. In patients older than four years, the male-to-female ratio is 8:1[6,7]. The etiology, presentation and management of intussusception in adults are different from those of children. In children, intussusception is usually idiopathic or secondary to a viral illness. Furthermore, the ileocecal valve may be functioning as the lead point in ileocecal intussusception[8]. In the adult population, primary or idiopathic intussusception accounts for about 8%-20% of cases[9,10]. Secondary intussusception, which is more common in the adult population, is associated with a pathological lesion involving a lead point, which can be a benign polyp, enlarged mesenteric lymph node, lipoma, appendix, Meckel’s diverticulum, or malignant tumors, such as lymphoma, gastrointestinal stromal tumor, primary or metastatic adenocarcinoma[4,10,11]. Lipomas may occur throughout the intestinal tract, but occur most frequently in the colon. Intussusception can be classified into four types depending on its location: (1) entero-enteric, or involving the small intestine; (2) colo-colic, or involving the large intestine; (3) ileo-colic, or involving the terminal ileum and ascending colon; and (4) ileo-cecal, or involving the ileo-cecal valve as the lead point[4,12].
Early diagnosis of adult intussusception is difficult because most cases present with non-specific signs and symptoms as well as have a chronic, sub-acute or acute course. The classic triad of intermittent abdominal pain, currant jelly stools, and a palpable tender mass seen in children is rarely present in adults. However, in adults, nausea, vomiting, gastrointestinal bleeding, changes in bowel habits and abdominal distension are more common[9,11]. Adult intussusceptions are detected using plain abdominal film, barium studies, colonoscopy, abdominal sonography, abdominal CT, angiography and magnetic resonance imaging[11,13,14]. Although there are several diagnostic imaging techniques, as mentioned above, an abdominal CT scan is the most commonly used and accurate diagnostic modality[9,13-15]. CT shows “target” or “sausage”-shaped lesions, while also defining the location, nature and relationship of the lesion to surrounding tissues with an accuracy that ranges from 60% to 100%[3,9,13,15]. Abdominal ultrasonography has also been successful in diagnosing intussusception, especially if a palpable mass is found[16].
Adult intussusception is associated with a pathological lesion involving a lead point. Therefore, surgical intervention is mandatory. Most surgeons accept that adult intussusception requires surgical intervention because of the large proportion of structural anomalies and the high incidence of occurring malignancy[4].
Endoscopic resection has been reported, but it can result in unfavorable complications, including perforation or hemorrhage. Surgical resection is commonly recommended to remove the lead point, such as lipomas that are larger than 2-cm in diameter[17].
Emergency physicians and clinicians frequently face a patient complaining of abdominal pain. Ileocolic intussusception is a rare cause of abdominal pain in adults that can often be elusive due to the frequent lack of peritoneal irritation signs and specific symptoms. Complications associated with intussusception, which rarely occur when the diagnosis is prompt, include perforation during non-operative reduction, wound infection, sepsis from undetected peritonitis (which is a major complication that occurs following a missed diagnosis), necrosis and bowel perforation and recurrence. While intussusception itself has good prognosis, the main prognostic factor affecting the course of the disease is the nature of the causative lesion. Mortality for adult intussusception increases from 8.7% of cases with benign lesions to 52.4% of cases with malignant lesions[9].
A sufficient level of vigilance and appropriate investigations are important for a prompt diagnosis and surgical referral of patients for a favorable outcome. In this case, we illustrate the importance of a thorough evaluation in patients with acute abdominal pain. In doing so, we highlight the diagnostic values of CT scanning and performing a complete ileocolonoscopy.
A 29-year-old Asian female presented to the authors’ emergency department with complaints of epigastric pain, nausea, fever and a chill that persisted for one day.
Ileocolic intussusception.
Acute enteritis, colitis, diverticulitis.
Laboratory data were significant for a white cell count of 11.34 × 109/L, with 93.7% neutrophils and the C-reactive protein of 8.21 mg/L, respectively.
Computed tomography demonstrated ileocolic intussusception and a 27-mm fatty dense mass.
The histopathology report confirmed a 3.5 cm × 2.7 cm submucosal lipoma in the terminal ileum.
Laparoscopic small bowel luminal mass resection was performed.
There have been various case reports of intussusception in adult on this rare disease entity.
Sufficient vigilance and appropriate investigations are important for prompt diagnosis and surgical referral of patients to enable favorable outcomes.
The case the authors reported was interesting.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: India
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lasithiotakis K, Lee HC S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Ghaderi H, Jafarian A, Aminian A, Mirjafari Daryasari SA. Clinical presentations, diagnosis and treatment of adult intussusception, a 20 years survey. Int J Surg. 2010;8:318-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 2. | Haas EM, Etter EL, Ellis S, Taylor TV. Adult intussusception. Am J Surg. 2003;186:75-76. [PubMed] |
| 3. | Barussaud M, Regenet N, Briennon X, de Kerviler B, Pessaux P, Kohneh-Sharhi N, Lehur PA, Hamy A, Leborgne J, le Neel JC. Clinical spectrum and surgical approach of adult intussusceptions: a multicentric study. Int J Colorectal Dis. 2006;21:834-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 164] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 4. | Marinis A, Yiallourou A, Samanides L, Dafnios N, Anastasopoulos G, Vassiliou I, Theodosopoulos T. Intussusception of the bowel in adults: a review. World J Gastroenterol. 2009;15:407-411. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 428] [Cited by in RCA: 505] [Article Influence: 31.6] [Reference Citation Analysis (2)] |
| 5. | Stringer MD, Pablot SM, Brereton RJ. Paediatric intussusception. Br J Surg. 1992;79:867-876. [PubMed] |
| 6. | Shapkina AN, Shapkin VV, Nelubov IV, Pryanishena LT. Intussusception in children: 11-year experience in Vladivostok. Pediatr Surg Int. 2006;22:901-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Parashar UD, Holman RC, Cummings KC, Staggs NW, Curns AT, Zimmerman CM, Kaufman SF, Lewis JE, Vugia DJ, Powell KE. Trends in intussusception-associated hospitalizations and deaths among US infants. Pediatrics. 2000;106:1413-1421. [PubMed] |
| 8. | Rogers SO, Lee MC, Ashley SW. Giant colonic lipoma as lead point for intermittent colo-colonic intussusception. Surgery. 2002;131:687-688. [PubMed] |
| 10. | Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg. 1997;173:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 382] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 11. | Eisen LK, Cunningham JD, Aufses AH. Intussusception in adults: institutional review. J Am Coll Surg. 1999;188:390-395. [PubMed] |
| 12. | Weilbaecher D, Bolin JA, Hearn D, Ogden W. Intussusception in adults. Review of 160 cases. Am J Surg. 1971;121:531-535. [PubMed] |
| 13. | Yakan S, Caliskan C, Makay O, Denecli AG, Korkut MA. Intussusception in adults: clinical characteristics, diagnosis and operative strategies. World J Gastroenterol. 2009;15:1985-1989. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 134] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Chang CC, Chen YY, Chen YF, Lin CN, Yen HH, Lou HY. Adult intussusception in Asians: clinical presentations, diagnosis, and treatment. J Gastroenterol Hepatol. 2007;22:1767-1771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Smith DS, Bonadio WA, Losek JD, Walsh-Kelly CM, Hennes HM, Glaeser PW, Melzer-Lange M, Rimm AA. The role of abdominal x-rays in the diagnosis and management of intussusception. Pediatr Emerg Care. 1992;8:325-327. [PubMed] |
| 16. | Reijnen HA, Joosten HJ, de Boer HH. Diagnosis and treatment of adult intussusception. Am J Surg. 1989;158:25-28. [PubMed] |
| 17. | Yu JP, Luo HS, Wang XZ. Endoscopic treatment of submucosal lesions of the gastrointestinal tract. Endoscopy. 1992;24:190-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |