Published online May 16, 2017. doi: 10.12998/wjcc.v5.i5.183
Peer-review started: December 7, 2016
First decision: January 16, 2017
Revised: March 7, 2017
Accepted: March 23, 2017
Article in press: March 24, 2017
Published online: May 16, 2017
Processing time: 159 Days and 16 Hours
Nasopharyngeal carcinoma (NPC) is a rare tumour that mainly metastasizes in lymph nodes, bones, lungs and liver. Colorectal metastases of NPC are extremely rare phenomenon and associated with a poor prognosis. We reported here a case of NPC with rectal metastasis, we discussed the treatment modalities and the prognosis after reviewing the similar cases described in the literature.
Core tip: This is a rare case of nasopharyngeal carcinoma with rectal metastasis. After reporting the similar cases in the literature, we discussed the prognosis and the treatment of this rare phenomenon.
- Citation: Vogel M, Kourie HR, Piccart M, Lalami Y. Unusual presentation of nasopharyngeal carcinoma with rectal metastasis. World J Clin Cases 2017; 5(5): 183-186
- URL: https://www.wjgnet.com/2307-8960/full/v5/i5/183.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v5.i5.183
Nasopharyngeal carcinoma (NPC) is a head and neck cancer starting in the upper part of the throat, behind the nose (nasopharynx). This tumor has different distribution and incidence worldwide with endemic regions: The incidence of NPC is lower than 1/100000 in most countries; however, in the southern part of China (including Hong Kong), its incidence is higher and can reach 15 to 20/100000. Otherwise, the incidence of NPC is higher in males, the sex ratio being 2-3:1[1,2].
Genetic susceptibility, Epstein-Barr chronic virus infection, and environmental factors (e.g., carcinogens and dietary factors) are risk factors associated to NPC[3,4]. NPC is divided into 3 subtypes by the World Health Organisation (WHO): Keratinizing squamous cell carcinoma, non-keratinizing carcinoma and undifferentiated carcinoma[5].
NPC has a tendency to metastasize to cervical lymph nodes, due to the abundant lymphatic network under the nasopharyngeal mucosa. At the time of diagnosis, 60%-85% of patients already have cervical metastasis[6]. The common distant metastasis are bones (65.9%), lungs (26.9%), liver (30.7%) and distant lymph nodes (28.5%). Other rare metastatic sites are described (2.4%) like spleen, kidney, pleura, breast gland, abdominal wall and thyroid gland[7]. The treatment of a non-metastatic patient is based on radiation therapy and/or chemotherapy. In metastatic NPC, the treatment is usually chemotherapy.
We report in this paper a rare presentation of NPC metastasizing to the rectum. We review the rare similar cases described in the literature about this association and discuss prognosis and treatment modalities of this unusual clinical presentation.
A 65-year-old smoker Caucasian patient presented to our department in July 2015 with stage IVc (T3N3bM1) non keratinizing undifferentiated NPC (WHO type III). The diagnosis was established by computed tomography (CT) requested for the investigation of chronic nasal obstruction and multiple cervical nodes. The tumour measured 7.2 cm in diameter. Multiple lymph nodes were palpable in the supra clavicular fossa. Further investigations with a positron emission tomography-computed tomography (PET-CT) showed metastatic lesions in bones and lungs. The patient was treated with radiotherapy therapy, because he refused the Cisplatin-5FU chemotherapy regimen and bisphosphonates for his bone metastasis. A post radiotherapy PET-CT showed a moderate metabolic response of the nasopharyngeal tumour and cervical lymph nodes, but also a metabolic progression in the distant metastatic lesions. A close follow-up was advised. A new progression in the adrenal glands, Th10-Th11 epiduritis and peritoneal carcinomatosis were reported after 7 mo. Epiduritis was treated with radiation therapy.
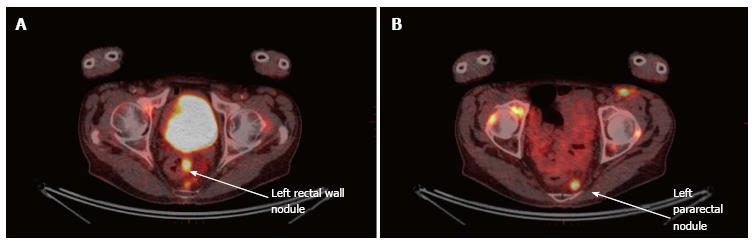
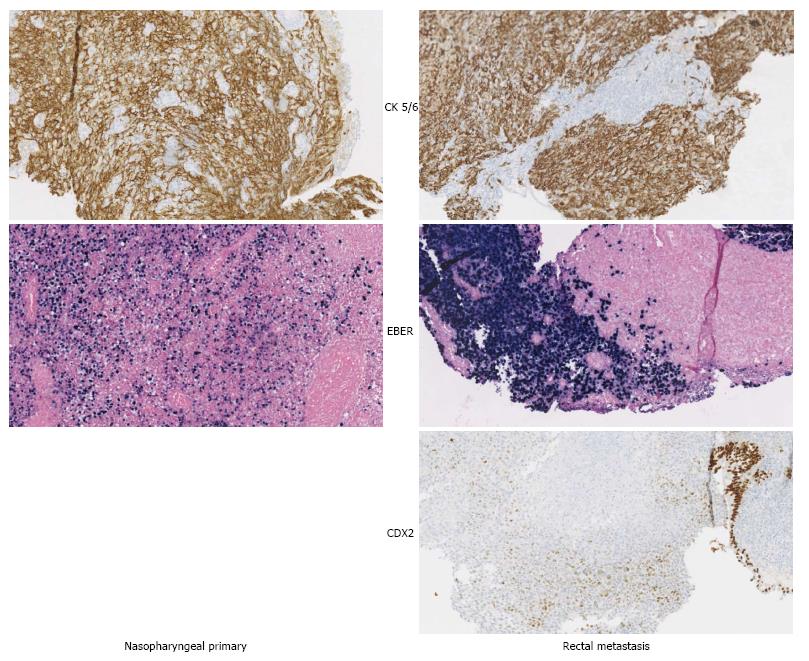
A follow-up PET-CT, after one year of the diagnosis, showed a suspicious lesion in the rectum (Figure 1). Before including the patient into a phase I protocol, it was necessary to document this lesion. The work-up included a colonoscopy revealing a rectal mass, and a biopsy documenting a metastatic lesion from the well-known nasopharyngeal non-keratinizing undifferentiated carcinoma (Figure 2). It was decided to start a palliative chemotherapy but the patient died one month without receiving any treatment.
Rectum and colon metastases of NPC are extremely rare entities. To our knowledge, there are only two similar cases described in the literature: One with rectal metastasis[8] and another with colon metastases[9]. These lesions are usually asymptomatic and diagnosed on complementary imaging tests.
Thus, Two out of three patients were asymptomatic; the only symptomatic patient was reported by Suppiah et al[8] and presented with rectal bleeding and abdominal pain. In the reported cases the patients had multiple other metastases before the diagnosis of the colorectal metastases. In the 3 cases, the patient shortly died after the diagnosis. In the case reported by Lahuri et al[9], the metastasis was interpreted first as rectal adenocarcinoma, leading to a right hemicolectomy. Chemotherapy was planned but the patient died rapidly (Table 1).
| Ref. | Age (yr) | Sites of metastasis | Other metastasis | Colorectal metastases treatment | Follow-up |
| Lahuri et al[9] (2015) | 61 | Ascending colon | Right adrenal gland, supraclavicular lymph nodes, liver, lungs | Right hemicolectomy | Patient died 2 mo later |
| Suppiah et al[8] (2006) | 64 | Rectum | Abdominal lymph nodes | None | Patient died 15 d later |
| The present case | 65 | Rectum | Lung, adrenal glands, bones, lymph nodes, epiduritis, peritoneal carcinomatosis | None | Patient died 1 mo later |
Differentiating between a secondary lesion and another primary in front of a rectal lesion in the context of NPC is essential to guide therapy. The diagnosis cannot be confirmed without a pathological exam including immune-histochemical staining to further characterize the lesion. In case of a confirmed secondary lesion, systemic chemotherapy is indicated, while in case of a rectal primary, a loco-regional treatment is prioritized.
Usually, the treatment for non metastatic NPC at early stages is radiotherapy, including both sides of the neck and retropharyngeal nodes. For locally advanced stages, the treatment guidelines advocate the combination of chemotherapy and radiotherapy. According to the response, surgery or brachytherapy can be considered as consolidation treatments[10]. In case of a metastatic NPC, the recommended first-line treatment is a platinum-based regimen and, more specifically, 5FU-cisplatin chemotherapy. In second line treatment, another chemotherapy can be proposed; the selection of which depends usually on the first-line treatment[11]. In the new era of checkpoint inhibitors, pembrolizumab, an anti-PD1 agent, showed remarkable results in advanced multitreated NPC with response rates of 26% and disease control rate of 77%[12].
To conclude, the diagnosis of rectal metastases originated of NPC is necessary to orient the treatment modality and to determine the prognosis of the disease.
The patient did not present particular symptoms at the diagnosis of rectal metastasis of nasopharngeal carcinoma.
The clinical examination of the patient was normal.
A rectal primary adenocarcinoma was a possible differential diagnosis.
A moderate anemia was the only laboratory test abnormality.
A follow-up positron emission tomography-computed tomography, after one year of the diagnosis of pharyngeal adenocarcinoma, showed a suspicious lesion in the rectum.
The work-up included a colonoscopy revealing a rectal mass, and a biopsy documenting a metastatic lesion from the well-known nasopharyngeal non-keratinizing undifferentiated carcinoma.
Palliative care was initiated because of the alteration of the performance status of the patient.
It is very important to confirm the pathology of unusual localization of a suspicious lesion in a patient developing cancer to differentiate between a metastasis and a second primary. The prognosis and the treatment of a rectal metastasis of nasopharyngeal carcinoma and rectal primary is very different.
The manuscript is of interest and well written.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Belgium
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Lai V, Li JJ, Tornesello ML S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Muir C, Waterhouse J, Mack T, Powell J, Whelan S. Cancer incidence in five continents, vol. V. Lyon, IARC: IARC scientific publications 1987; . |
| 2. | Parkin DM, Whelan SL, Ferlay J. Cancer incidence in five continents, vol. VIII. Lyon, IARC: IARC scientific publications 2002; . |
| 3. | Lee AW, Foo W, Mang O, Sze WM, Chappell R, Lau WH, Ko WM. Changing epidemiology of nasopharyngeal carcinoma in Hong Kong over a 20-year period (1980-99): an encouraging reduction in both incidence and mortality. Int J Cancer. 2003;103:680-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 126] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Jia WH, Luo XY, Feng BJ, Ruan HL, Bei JX, Liu WS, Qin HD, Feng QS, Chen LZ, Yao SY. Traditional Cantonese diet and nasopharyngeal carcinoma risk: a large-scale case-control study in Guangdong, China. BMC Cancer. 2010;10:446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 5. | Cheung F, Chan O, Ng WT, Chan L, Lee A, Pang SW. The prognostic value of histological typing in nasopharyngeal carcinoma. Oral Oncol. 2012;48:429-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Chong VF, Ong CK. Nasopharyngeal carcinoma. Eur J Radiol. 2008;66:437-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Shen LJ, Wang SY, Xie GF, Zeng Q, Chen C, Dong AN, Huang ZM, Pan CC, Xia YF, Wu PH. Subdivision of M category for nasopharyngeal carcinoma with synchronous metastasis: time to expand the M categorization system. Chin J Cancer. 2015;34:450-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Suppiah A, Karanikas I, MacDonald A, Monson JR, Hartley JE. Squamous cell carcinoma of the nasopharynx metastasising to rectum: first case report and literature review. Anticancer Res. 2006;26:4741-4744. [PubMed] |
| 9. | Lahuri YS, Mohamad I, Hashim H. Nasopharyngeal carcinoma with metastases to colon. Egyptian Journal of Ear, Nose, Throat and Allied Sciences. 2015;16:201-204. |
| 10. | Mesía R, Pastor M, Grau JJ, del Barco E. SEOM clinical guidelines for the treatment of nasopharyngeal carcinoma 2013. Clin Transl Oncol. 2013;15:1025-1029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Bensouda Y, Kaikani W, Ahbeddou N, Rahhali R, Jabri M, Mrabti H, Boussen H, Errihani H. Treatment for metastatic nasopharyngeal carcinoma. Eur Ann Otorhinolaryngol Head Neck Dis. 2011;128:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 125] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 12. | Hsu C, Lee S, Ejadi S, Even C, Cohen R, Le Tourneau C, Mehnert J, Algazi A, Van Brummelen E, Yuan SS. Antitumor activity and safety of pembrolizumab in patients with PD-L1-positive nasopharyngeal carcinoma: Interim results from a phase 1b study. EJC. 2015;51:S558-S558. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |