Published online Aug 16, 2016. doi: 10.12998/wjcc.v4.i8.219
Peer-review started: February 23, 2016
First decision: March 25, 2016
Revised: March 31, 2016
Accepted: May 31, 2016
Article in press: June 2, 2016
Published online: August 16, 2016
Processing time: 174 Days and 17.9 Hours
A 15-year-old boy with transposition of the great arteries (TGA) and neonatal arterial switch operation (ASO) presented with complete occlusion of the left main coronary artery (LMCA). Intra-operatively, an intramural left coronary artery was identified. Therefore, since age 7 years he had a series of screening exercise stress tests. At 13 years old, he had 3 to 4 mm ST segment depression in the infero-lateral leads without symptoms. This progressed to 4.2 mm inferior ST segment depression at 15 years old with normal stress echocardiogram. Sestamibi myocardial perfusion scan and cardiac magnetic resonance imaging was inconclusive. Therefore, a coronary angiogram was obtained which showed complete occlusion of the LMCA with ample collateralization from the right coronary artery system. This was later confirmed on a computed tomogram (CT) angiogram, obtained in preparation of coronary artery bypass grafting. The case illustrates the difficulty of detecting coronary artery stenosis and occlusion in young patients with rich collateralization. Coronary CT angiogram and conventional angiography were the best imaging modalities to detect coronary anomalies in this adolescent with surgically corrected TGA. Screening CT angiography may be warranted for TGA patients, particularly for those with known coronary anomalies.
Core tip: In complete transposition of the great arteries (TGA), neonatal arterial switch operation offers excellent long term survival. Yet there can be late coronary artery complications. In this case, an asymptomatic teenager had an abnormal screening exercise-stress test leading to the identification of complete left coronary occlusion. This case illustrates how rich coronary collateralization can obscure even complete coronary occlusion. As such, young patients pose a unique diagnostic challenge. Coronary computed tomogram (CT) angiogram and conventional angiography were the best imaging modalities to detect the problem. Screening CT angiography may be warranted for TGA patients, particularly for those with known coronary anomalies.
- Citation: Saini AP, Cyran SE, Ettinger SM, Pauliks LB. Coronary artery occlusion after arterial switch operation in an asymptomatic 15-year-old boy. World J Clin Cases 2016; 4(8): 219-222
- URL: https://www.wjgnet.com/2307-8960/full/v4/i8/219.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i8.219
Complete transposition of the great arteries (TGA) is the most common cyanotic heart defect and lethal unless treated during infancy. Currently, most patients undergo an arterial switch operation (ASO) which involves transfer of the coronary arteries from the native to the neo-aorta. Successful coronary transfer during the ASO is crucial for long term morbidity and mortality of this operation[1]. There is increasing awareness of late coronary artery complications in long-term survivors following the ASO[1-4]. Patients with these late coronary lesions may be asymptomatic. Therefore, adult guidelines have recommended routine screening coronary angiography but this approach is not widely accepted in Pediatrics[5]. This case illustrates the limitations of the different other diagnostic techniques available to detect myocardial ischemia in this scenario.
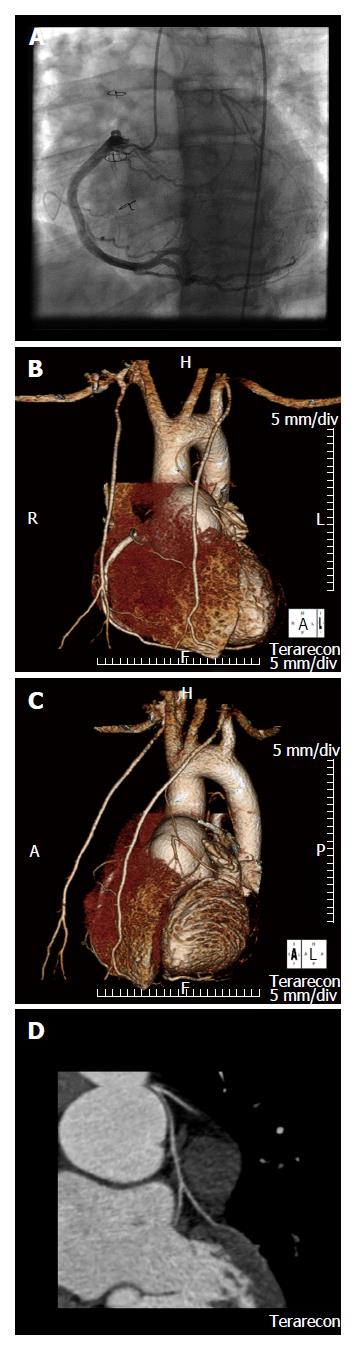
A 15-year-old boy presented with an abnormal screening exercise stress test. He had undergone ASO for complete TGA as a newborn. Intra-operatively, he was found to have an intramural course of the left main coronary artery (LMCA) and also required revision of the operation for bleeding a day later. During serial follow up, he was asymptomatic. Physical examination was unremarkable except for obesity and a grade 2/6 systolic ejection murmur at the left sternal border with radiation to the back. The murmur was consistent with mild branch pulmonary artery stenosis, documented on baseline echocardiogram. He underwent his first maximal exercise stress test (EST) using the Bruce protocol at 7 years of age. Initially, he showed non-specific infero-lateral ST segment depression of up to 2 mm. Repeat EST at age 13 showed 3 to 4 mm inferolateral ST segment depression. This was deemed incidental in the absence of clinical symptoms and with a normal stress echocardiogram. Serial screening Holter electrocardiograms were also reassuring with rare isolated unifocal premature contractions. At age 15, follow up EST revealed up to 4.2 mm inferior and lateral ST segment depression, again with a normal stress echocardiogram. The patient was restricted from competitive sports and started on beta blocker therapy. He subsequently reported resolution of the palpitations that he had felt but never mentioned before. On follow up, sestamibi stress test after one months of atenolol, the ST segment changes were reproducible and unchanged. Myocardial perfusion didn’t show ischemia or wall motion abnormalities. However, there was a fixed anterior and antero-septal defect with no evidence of ischemia. Cardiac magnetic resonance imaging (MRI) with late gadolinium enhancement was negative. The coronary arteries were not seen well on MRI. A coronary angiogram then revealed complete ostial occlusion of the LMCA (Figure 1). There was with ample collateralization from the right coronary artery system retrograde supplying the LMCA (Figure 1). A computer tomography angiogram (obtained in preparation for the surgical revascularization procedure) also showed diffuse hypoplasia of the left coronary artery system (Figure 1B-D). The patient underwent coronary artery bypass grafting with the left internal mammary artery to the left anterior descending (LAD). He is now a year out from his bypass surgery and is doing well clinically. However, there is persistent mild inferolateral ST segment depression on maximal EST with normal stress echocardiogram.
Occult coronary artery obstruction has been increasingly recognized in long-term survivors following the ASO[1-4]. Therefore, lifelong follow-up is recommended after ASO, and a one-time evaluation of the patency of the coronary arteries has to be considered according to the current American Heart Association/European Society of Cardiology (AHA/ESC) guidelines for adults with congenital heart disease[5,6]. This case illustrates the difficulties encountered in diagnosing late coronary events years after the ASO in young patients without atherosclerosis. Many patients with late coronary lesions are asymptomatic or are not aware of the significance of symptoms (like this patient who didn’t report his palpitations). If coronary stenosis developed slowly in young patients, collaterals can develop. Myocardial ischemia then may manifest itself late, well into teenage years. Occult coronary problems may be unmasked by growth spurts and increased oxygen demand as the adolescents challenge themselves more in sports and other activities. Although retrograde perfusion from collateral circulation may initially provide sufficient perfusion of the myocardium, coronary blood flow can become insufficient with growth and during periods of increased myocardial demand. This puts these patients at risk for sudden cardiac death as first sign of their coronary problem.
Adult congenital heart disease guidelines now comprise a recommendation for coronary angiography after ASO[2]. However, in Pediatric Cardiology, the practice of routine coronary angiography in ASO survivors has not been widely implemented as the risk benefit ratio for cardiac catheterization in asymptomatic ASO survivors is unclear[7]. Computed tomogram (CT) angiogram now offers a more acceptable screening method that is equally highly sensitive and specific. In children, non-invasive methods to assess coronaries are preferable. This case shows that a CT angiogram provided optimal visualization of the coronary anatomy. Based on this experience, CT angiograms could potentially become the screening test of choice to assess coronary anatomy following the ASO for TGA. It also allows excellent interrogation of the branch pulmonary arteries following the Lecompte maneuver.
Treatment of coronary artery problems following ASO for TGA can be challenging. Surgical and percutaneous coronary revascularization has been employed in patients with evidence of myocardial ischemia with mixed results[8]. Based upon the experience with surgical intervention for anomalous origin of the coronary artery from opposite sinus in the absence of structural heart disease, we know that nearly half of the children still had abnormal stress testing electrocardiogram (ECG) findings with normal stress echocardiograms post-operatively[9,10]. Therefore, further follow up of these patients is challenging.
This case calls attention to the potential of coronary CT angiogram in diagnosing late coronary obstruction in patients post arterial switch operation for transposition of the great arteries. Screening with exercise stress testing helped to raise suspicion of a problem but this standard method was ultimately non-diagnostic in this scenario. Therefore, CT angiogram or coronary angiogram should be considered in teenagers, as recommended by current guidelines for the management of adults with surgically corrected transposition of the great arteries.
The 15-year-old male patient was asymptomatic but had a severe coronary artery problem putting him at risk for sudden cardiac death following arterial switch operation for complete transposition of the great arteries as a newborn.
Complete occlusion of the left coronary artery.
Nonspecific ST segment changes.
Complete occlusion of left coronary artery.
Coronary artery bypass operation.
Late coronary artery complications are a recognized complication of the arterial switch operation for complete transposition of the great arteries. However, the optimal diagnostic work up is still unclear.
Computed tomogram computer tomography.
Treatment of coronary artery problems following arterial switch operation for transposition of the great arteries (TGA) can be challenging due to their atypical presentation compared to adults with ischemic heart disease.
The authors present a case report of complete left main coronary artery occlusion after arterial switch operation in an asymptomatic15-year-old boy. They have concluded that coronary computed tomography angiogram or coronary angiogram (CAG) should be considered in patients with TGA. This manuscript is nicely structured and well written.
Manuscript source: Invited manuscript
Specialty type: Medicine
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B, B, B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Firstenberg MS, Jiang B, Kettering K, Najafi M, Peteiro J, Ueda H S- Editor: Qiu S L- Editor: A E- Editor: Zhang FF
| 1. | Oda S, Nakano T, Sugiura J, Fusazaki N, Ishikawa S, Kado H. Twenty-eight years’ experience of arterial switch operation for transposition of the great arteries in a single institution. Eur J Cardiothorac Surg. 2012;42:674-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 2. | Legendre A, Losay J, Touchot-Koné A, Serraf A, Belli E, Piot JD, Lambert V, Capderou A, Planche C. Coronary events after arterial switch operation for transposition of the great arteries. Circulation. 2003;108 Suppl 1:II186-II190. [PubMed] |
| 3. | Lalezari S, Bruggemans EF, Blom NA, Hazekamp MG. Thirty-year experience with the arterial switch operation. Ann Thorac Surg. 2011;92:973-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Tobler D, Williams WG, Jegatheeswaran A, Van Arsdell GS, McCrindle BW, Greutmann M, Oechslin EN, Silversides CK. Cardiac outcomes in young adult survivors of the arterial switch operation for transposition of the great arteries. J Am Coll Cardiol. 2010;56:58-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 124] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 5. | Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasules JW, Graham TP, Hijazi ZM. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines on the management of adults with congenital heart disease). Circulation. 2008;118:e714-e833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 663] [Cited by in RCA: 636] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 6. | Baumgartner H, Bonhoeffer P, De Groot NM, de Haan F, Deanfield JE, Galie N, Gatzoulis MA, Gohlke-Baerwolf C, Kaemmerer H, Kilner P. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). Eur Heart J. 2010;31:2915-2957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1602] [Cited by in RCA: 1555] [Article Influence: 103.7] [Reference Citation Analysis (1)] |
| 7. | Oztunç F, Bariş S, Adaletli I, Onol NO, Olgun DC, Güzeltaş A, Ozyilmaz I, Ozdil M, Kurugoğlu S, Eroğlu AG. Coronary events and anatomy after arterial switch operation for transposition of the great arteries: detection by 16-row multislice computed tomography angiography in pediatric patients. Cardiovasc Intervent Radiol. 2009;32:206-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Legendre A, Chantepie A, Belli E, Vouhé PR, Neville P, Dulac Y, Vaksmann G, Bonnet D, Serraf A. Outcome of coronary artery bypass grafting performed in young children. J Thorac Cardiovasc Surg. 2010;139:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Brothers JA, McBride MG, Seliem MA, Marino BS, Tomlinson RS, Pampaloni MH, Gaynor JW, Spray TL, Paridon SM. Evaluation of myocardial ischemia after surgical repair of anomalous aortic origin of a coronary artery in a series of pediatric patients. J Am Coll Cardiol. 2007;50:2078-2082. [PubMed] |
| 10. | Brothers JA, Gaynor JW, Jacobs JP, Poynter JA, Jacobs ML. The Congenital Heart Surgeons’ Society Registry of Anomalous Aortic Origin of a Coronary Artery: an update. Cardiol Young. 2015;25:1567-1571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |