Published online Aug 16, 2016. doi: 10.12998/wjcc.v4.i8.213
Peer-review started: February 27, 2016
First decision: April 15, 2016
Revised: May 2, 2016
Accepted: May 31, 2016
Article in press: June 2, 2016
Published online: August 16, 2016
Processing time: 169 Days and 4.1 Hours
AIM: To examine whether it is possible to prevent the occurrence of post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis in patients experiencing difficulties with selective biliary duct cannulation by pancreatic duct stenting using a loop-tipped guidewire.
METHODS: Procedure success rate, frequency of unintended insertion of the guidewire into side branches of the pancreatic duct, and incidence of procedural accidents were examined using a loop-tipped guidewire (Group A, 20 patients), and a conventional straight-type guidewire (Group B, 20 patients).
RESULTS: The success rate of the procedure was 100% in both groups. Unintended insertion of the guidewire into a side branch of the pancreatic duct occurred 0.056 ± 0.23 (0-1) times in Group A and 2.3 ± 1.84 (0-5) times in Group B; thus, unintended insertion of the guidewire into a side branch of the pancreatic duct was seen significantly less frequently in Group A. There were no procedural accidents in Group A, whereas pancreatitis occurred in one Group B patient; however, the difference between the two groups was not statistically significant. The serum amylase level after ERCP was 257.15 ± 136.4 (88-628) IU/L in Group A, and 552.05 ± 534.57 (101-2389) IU/L in Group B, showing a significantly lower value in Group A. Hyperamylasemia was found in two patients (10%) in Group A, and nine (45%) in Group B, showing a significantly lower value in Group A.
CONCLUSION: The results suggest that in patients who experience difficulties with biliary cannulation, the use of a loop-tipped guidewire for pancreatic duct stenting may assist with the prevention of post-ERCP pancreatitis, and thereby to a reduction of the risk of post-ERCP pancreatitis or hyperamylasemia.
Core tip: The results suggest that a loop-tipped guidewire inserted in the pancreatic duct during stenting in patients who experience difficulties with selective biliary duct cannulation has the potential to assist with prevention of unintended insertion of the guidewire into side branches of the pancreatic duct, and thereby contribute to a reduced risk of post-endoscopic retrograde cholangiopancreatography pancreatitis or hyperamylasemia.
- Citation: Sakai Y, Tsuyuguchi T, Sugiyama H, Hayashi M, Senoo JI, Sasaki R, Kusakabe Y, Nakamura M, Yasui S, Mikata R, Miyazaki M, Yokosuka O. Prevention of post-endoscopic retrograde cholangiopancreatography pancreatitis by pancreatic duct stenting using a loop-tipped guidewire. World J Clin Cases 2016; 4(8): 213-218
- URL: https://www.wjgnet.com/2307-8960/full/v4/i8/213.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i8.213
Endoscopic retrograde cholangiopancreatography (ERCP) is no longer a purely diagnostic technique. It has developed into an exclusively therapeutic procedure to treat pancreatic and biliary disease. Post-ERCP pancreatitis is the commonest early side effect of this procedure. Although its frequency varies according to the patient, technique employed, definition of pancreatitis, and method of investigation, it is generally reported to occur in about 4.5% of patients based on the results of large-scale prospective studies[1-7]. Although in many cases post-ERCP pancreatitis abates after admission and treatment for a few days, it may aggravate. It is reported that about 0.04% of patients need surgery, while about 0.03% of them die[1,2,4,5]. Elimination of post-ERCP pancreatitis is a goal that has not been achieved, despite various attempts, since the adoption of ERCP. Pancreatic duct stenting is one strategy for preventing the occurrence of pancreatitis caused by duodenal papilledema resulting from difficult selective biliary cannulation. Its usefulness is frequently reported[8-12].
However, in some patients who experience difficult selective biliary duct cannulation, pancreatic duct stenting fails to prevent pancreatitis. One past report describing the occurrence of pancreatitis in spite of pancreatic duct stenting suggests that pancreatitis might have occurred due to frequent unintended insertion of the guidewire into side branches of the pancreatic duct when placing the guidewire into the pancreatic duct[8]. In this study, we aimed to prevent post-ERCP pancreatitis by placing a loop-tipped guidewire into the pancreatic duct during pancreatic duct stenting in patients experiencing difficult selective biliary duct cannulation.
Of 1218 patients undergoing ERCP from and of 502 patients who had not undergone ERCP from experiencing difficulty with selective biliary cannulation were April 2013 to April 2015, 20 patients included in our test group (Group A). Of these 20 patients, 1 underwent diagnostic ERCP and 19 underwent therapeutic ERCP. We decided whether the patients had experienced difficulties with selective biliary cannulation 15 min after cannulation had been attempted employing a contrast method using a conventional imaging catheter and directly examining the duodenal papilla. ERCP was conducted by doctors who are accredited as specialists by the Japan Gastroenterological Endoscopy Society and have experience with ERCP in more than 3000 patients (Y.S., T.T.). Group A consisted of 10 male patients and 10 female patients, whose mean age was 71.68 ± 9.53 years old (43 to 85 years old), and included 12 with bile duct stones, three with cholangiocarcinoma, 3 with pancreatic cancer, 1 with intraductal papillary mucinous neoplasm (IPMN) and one with gallbladder cancer.
Before ERCP, all patients were given the standard premedication consisting of intravenous administration of midazolam (3-10 mg), with the dose adjusted for age and tolerance. Scopolamine butylbromide or glucagon was used to induce duodenal relaxation. During ERCP, arterial oxygen saturation was continuously monitored using a pulse oximeter. Patients were kept fasting for at least 24 h after the procedure and remained as inpatients for at least 72 h. They received an 8-h infusion of a protease inhibitor (nafamostat mesylate, 20 mg/d) and antibiotics (SBT/CPZ, 2 g/d) for 2 d. Serum amylase level was measured before and about 18 h after ERCP. The reference range for amylase was 42-135 IU/L. Patients were clinically evaluated for symptoms (abdominal pain, nausea, etc.) and physical findings (abdominal tenderness).
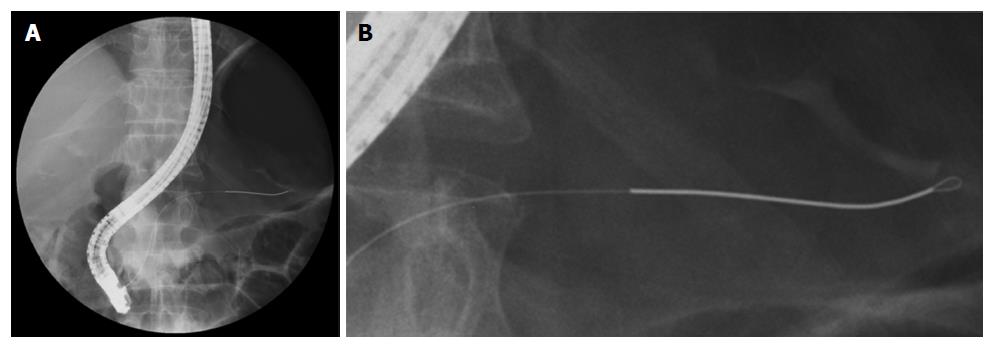
The procedures were carried out using side-viewing duodenoscopes (JF240, 260V, TJF260V: Olympus Corp., Tokyo, Japan). For cannulation, catheters PR-104Q, PR-110Q-1 and PR-233Q were used. A 0.035-inch guidewire (Loop tip: Cook Medical Corp., Winston-Salem, NC) was employed (Figure 1). In patients experiencing difficult selective biliary duct cannulation, cannulation of the biliary duct was attempted using the pancreatic duct guidewire-placing method (P-GW) or transpancreatic precut papillotomy (TPPP) by inserting the guidewire into the pancreatic duct. In such cases, the guidewire was first inserted up to the caudal segment of the main pancreatic duct to keep the guidewire stable during the procedure. Since the pancreatic duct was imaged by contrast imaging, close attention was paid to its morphology to prevent the guidewire from being inserted into any side branches. If any resistance was encountered during insertion, the guidewire was moved forward carefully so as to avoid labored insertion. Patients were excluded from this study if cannulation of both the biliary and pancreatic ducts failed. The loop tip guidewire was inserted into the pancreatic duct via the cannula to stabilize the papilla of Vater and straighten the bile duct terminal (Figure 2). In P-GW, biliary cannulation was tried with the guidewire placed in the pancreatic duct. After successful cannulation of the biliary duct, additional procedures such as endoscopic sphincterotomy (EST), biliary stent placement, intraductal ultrasonography (IDUS), biopsy of the biliary duct, etc., were performed as necessary. If selective biliary cannulation was not successful using the P-GW method, even when tried for 15 min, TPPP was selected instead. TPPP was conducted using a Clever-Cut3V (Olympus Corp.) at the discretion of the operator. A papillotome was inserted under induction with a guidewire. Dissection was conducted using an Olympus PSD-20 Electrosurgical Unit (Olympus Corp.) at a power of 25 W. Dissection was conducted by directing the dissection blade toward the 11 or 12 o’clock direction of the bile duct. After dissection, biliary cannulation was attempted using the bile discharged from the opening in the biliary duct and the biliary mucosa as marks. After successful biliary cannulation, the target procedure was conducted; thereafter, pancreatic duct stenting was carried out. A 5-Fr 3-cm straight unilateral-flapped stent (Geenen Pancreatic Stent: Cook Medical Corp.) was placed using a pushing tube under induction of the guidewire in a configuration that crossed the duodenal papilla. Cannulation was conducted employing a conventional imaging catheter. No wire-guided cannulation was performed. We did not use nonsteroidal anti-inflammatory drugs (NSAIDs) in all cases. All the patients had provided their written informed consent before these diagnostic and therapeutic procedures. Iatrogenic morbidity was assessed according to the criteria of Cotton et al[13]. Hyperamylasemia was defined as serum amylase ≥ 3 times the normal level (42-135 IU/L), independent of the presence or absence of abdominal pain. The results obtained using the loop-tipped guidewire were compared with those obtained in 20 patients (Group B) who had experienced difficult selective biliary duct cannulation and in whom the procedures had been successful after the placement of a guidewire (0.025-inch VisiGlide, straight type: Olympus Corp.) in the pancreatic duct. These 20 patients were selected from among 188 patients who had undergone ERCP for the first time between December 2010 and May 2012. All the procedures were recorded on video, and the success rate, incidence of procedural accidents, and frequency of unintended insertion of the guidewire into a side branch of the pancreatic duct were examined. This study was conducted after obtaining the approval of the Institutional Ethics Committee.
Data were analyzed using Statistical Package for Social Science (SPSS) software version 18 (SPSS, Chicago, IL). Fisher’s exact probability test, Student’s t test, and the Mann-Whitney U-test were used for statistical analyses to compare the blood test findings and patient background. A P value of < 0.05 was regarded as significant.
There were no significant differences in clinical background between patients who underwent ERCP using the loop-tipped guidewire (Group A) and those who underwent ERCP using the straight-type guidewire (Group B) (Table 1). In Group A, 5 patients underwent P-GW, and 15 patients underwent P-GW + TPPP. Selective biliary duct insertion was successful in all these patients. EST was then conducted in 19 patients, lithotomy in 12, biliary stent placement in 7, IDUS in 1, and biopsy of the biliary duct in 1. No significant differences were observed in the procedures conducted, cannulation time, or even procedure time when compared with Group B (Table 2). The target procedures were accomplished in both groups of patients. After completion of the procedure, pancreatic duct stenting was attempted and proved successful in all the patients in both groups. No procedural accidents, such as bleeding, perforation, or pancreatitis were observed in Group A. In Group B, there were no cases of bleeding or perforation, but mild pancreatitis was observed in one patient, who was treated conservatively. The serum amylase level at baseline was 72.84 ± 20.63 (41-112) IU/L in Group A, and 72.75 ± 20.40 (43-120) IU/L in Group B, showing no significant difference between the two groups. After ERCP, the level of serum amylase was 257.15 ± 136.44 (88-628) IU/L in Group A, and 552.05 ± 534.57 (101-2389) IU/L in Group B, showing a significantly lower value in Group A. The frequency of unintended insertions of the guidewire into a side branch of the pancreatic duct was 0.056 ± 0.23 (0-1) times in Group A, and 2.3 ± 1.84 (0-5) times in Group B, showing a significantly reduced frequency in Group A. Hyperamylasemia was observed in two patients (10%) in Group A, and in nine (45%) patients in Group B: A significantly lower value in Group A (Table 3).
| Loop-type guidewire (Group A) | Straight-type guidewire (Group B) | P-value | |
| n | 20 | 20 | |
| Age | 71.68 ± 9.53 (43-85) | 71.63 ± 10.36 (39-80) | NS |
| Sex | Males 10, females 10 | Males 10, females 10 | NS |
| Disease | |||
| Bile duct stone | 12 | 12 | NS |
| Cholangiocarcinoma | 3 | 3 | NS |
| Pancreatic cancer | 3 | 2 | NS |
| Gallbladder cancer | 1 | 2 | NS |
| Intraductal papillary mucinous neoplasm | 1 | 1 | NS |
| Diagnostic ERCP | 1 | 1 | NS |
| Therapeutic ERCP | 19 | 19 | NS |
| Loop-type guidewire (Group A) | Straight-type guidewire (Group B) | P-value | |
| P-GW | 5 | 6 | NS |
| P-GW + TPPP | 15 | 14 | NS |
| Endoscopic sphincterotomy | 19 | 19 | NS |
| Lithotomy | 12 | 12 | NS |
| Biliary stenting | 7 | 7 | NS |
| Intraductal ultrasonography | 1 | 1 | NS |
| Biopsy of the bile duct | 1 | 1 | NS |
| Pancreatic duct stenting | 20 | 20 | NS |
| Pancreatic duct injection | 1.263 ± 0.562 | 1.286 ± 0.588 | NS |
| (1-3) | (1-3) | ||
| Cannulation time (min) | 33.45 ± 9.72 | 34.9 ± 97.04 | NS |
| (16-50) | (16-50) | ||
| Procedure time (min) | 44.2 ± 13.22 | 46.8 ± 14.03 | NS |
| (23-70) | (20-63) |
| Loop-type guidewire (Group A) | Straight-type guidewire (Group B) | P-value | |
| Bleeding | 0 | 0 | - |
| Perforation | 0 | 0 | - |
| Pancreatitis | 0 | 1 | NS |
| Pre-ERCP amylase level | 72.84 ± 20.63 | 72.75 ± 20.40 | NS |
| (41-112) | (43-120) | ||
| Post-ERCP amylase level | 257.15 ± 136.44 | 552.05 ± 534.57 | < 0.05 |
| (88-628) | (101-2389) | ||
| Frequency of unintended insertion of the guidewire into a side branch of the pancreatic duct | 0.056 ± 0.23 | 2.3 ± 1.84 | < 0.05 |
| (0-1) | (0-5) | ||
| Hyperamylasemia | 2 | 9 | < 0.05 |
| Others | 0 | 0 | - |
According to past reports on the prevention of post-ERCP pancreatitis, it is currently impossible to completely suppress its occurrence. Post-ERCP pancreatitis is thought to occur due to various factors. It is suspected that one or more concomitant factors may cause pancreatitis. With regard to its prevention, pancreatic duct stenting has been reported to be useful in reducing the increased inner pressure associated with buildup of pancreatic juice caused by postoperative papilledema. However, pancreatitis cannot as yet be entirely eliminated. According to our experience, pancreatitis occurs in patients who experience difficulties with selective biliary duct cannulation: These patients are more likely to develop postoperative papilledema despite pancreatic duct stenting, probably because the reason for the development of post-ERCP pancreatitis is multifactorial. Examination of patients who experience difficult selective biliary duct cannulation and who developed pancreatitis even after pancreatic duct stenting showed that in some patients the guidewire was unintentionally inserted into a side branch of the pancreatic duct multiple times: This may have stimulated or damaged the pancreatic duct, leading to the onset of pancreatitis[8]. Since the pancreatic duct is S-shaped and has branches, it is difficult to insert a guidewire through the main pancreatic duct toward its caudal segment without any problems. Since the guidewire we employed in this study is the loop-tipped type, we anticipated a very low risk of inserting the guidewire into a branch of the duct. Video recording of the actual procedure revealed that unintended insertion of the guidewire into a branch did not occur unless the branched pancreatic duct was markedly dilated due to IPMN. Since the conventional straight-type guidewire is reported to be too frequently, although unintentionally, inserted into side branches of the pancreatic duct, it appears that amylase levels after ERCP tended to be significantly lower in the A group, although no significant difference was observed in the incidence of pancreatitis. These results suggest that pancreatic duct stenting after inserting the loop-tipped guidewire into the pancreatic duct can prevent stimulation or damage to the pancreatic duct by unintended insertion of the guidewire into branched ducts and thus reduce the risk of pancreatitis. Another type of guidewire, the J-type tip guidewire, is associated with a lower risk of insertion into branched ducts. However, its tip may be unintentionally inserted into the branched ducts while retracting the guidewire. Therefore, the loop-tipped guidewire is currently the design with the lowest risk of unintended insertion into side branches of the pancreatic duct[14,15]. This study was conducted in a small number of patients, but the results warrant future studies using larger samples that would include randomized controlled trials. Although this study was conducted using the contrast method and a catheter, inevitably examination by wire-guided cannulation will become necessary. With regard to the contrast method, since a contrast radiograph of the pancreatic duct is often taken when inserting the guidewire into the pancreatic duct, the openness of the pancreatic duct can be assessed to some degree. Contrast medium is not used for wire-guided cannulation, however: The guidewire is advanced blindly, without assessing the openness of the pancreatic duct[14-17], and if the loop-tipped guidewire is not inserted easily into the side branches of the pancreatic duct, this method can be considered even more useful. Various examinations may be necessary to further evaluate the usefulness of this type of guidewire.
Our results suggest that a loop-tipped guidewire inserted into the pancreatic duct during stenting in patients who experience difficulty with selective biliary duct cannulation could assist with the prevention of unintended insertion of the guidewire into side branches of the pancreatic duct, and thereby to a reduced risk of post-ERCP pancreatitis or hyperamylasemia.
Preventing post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis is a task that has not been resolved since the introduction of ERCP, despite numerous attempts. As one of such attempts, pancreatic duct stenting is used to prevent the occurrence of pancreatitis caused by duodenal papilledema resulting from difficult selective biliary cannulation, and its usefulness is frequently reported. In this study, the authors aimed to prevent post-ERCP pancreatitis by placing a loop-tipped guidewire into the pancreatic duct while pancreatic duct stenting is attempted in patients who experienced difficulty with selective biliary duct cannulation.
Procedure success rate, frequency of unintended insertion of the guidewire into side branches of the pancreatic duct, and incidence of procedural accidents were examined using a loop-tipped guidewire (Group A, 20 patients), and a conventional straight-type guidewire (Group B, 20 patients).
Unintended insertion of the guidewire into a side branch of the pancreatic duct occurred 0.056 ± 0.23 (0-1) times in Group A and 2.3 ± 1.84 (0-5) times in Group B: Thus, unintended insertion of the guidewire into a side branch of the pancreatic duct was seen significantly less frequently in Group A. Hyperamylasemia was found in two patients (10%) in Group A, and in nine patients (45%) in Group B, showing a significantly lower value in Group A. Pancreatic duct stenting using a loop-tipped guidewire may assist with the prevention of post-ERCP pancreatitis, and thereby to a reduction in the risk of post-ERCP pancreatitis or hyperamylasemia.
Pancreatitis caused by duodenal papilledema due to difficult selective biliary cannulation.
The results suggest that in patients experiencing difficulty with biliary cannulation, pancreatic duct stenting using a loop-tipped guidewire can assist with the prevention of post-ERCP pancreatitis, and thereby to a reduction in the risk of post-ERCP pancreatitis or hyperamylasemia.
This is very interesting manuscript from the clinical point of view.
Manuscript source: Invited manuscript
Specialty type: Medicine
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Malak M, Vujasinovic M S- Editor: Ji FF L- Editor: A E- Editor: Zhang FF
| 1. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1689] [Article Influence: 58.2] [Reference Citation Analysis (2)] |
| 2. | Loperfido S, Angelini G, Benedetti G, Chilovi F, Costan F, De Berardinis F, De Bernardin M, Ederle A, Fina P, Fratton A. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998;48:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 779] [Article Influence: 28.9] [Reference Citation Analysis (1)] |
| 3. | Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 4. | Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 801] [Cited by in RCA: 835] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 5. | Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M, Geenen J, Ryan M, Parker H, Frakes JT, Fogel EL. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 433] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 6. | Wang P, Li ZS, Liu F, Ren X, Lu NH, Fan ZN, Huang Q, Zhang X, He LP, Sun WS. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009;104:31-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 357] [Cited by in RCA: 329] [Article Influence: 20.6] [Reference Citation Analysis (1)] |
| 7. | Sakai Y, Tsuyuguchi T, Hirata N, Nakaji S, Shimura K, Fujimoto T, Tsuchiya S, Nishino T, Nishikawa T, Sugiyama H. Can endoscopic sphincterotomy be performed safely in elderly patients aged 80 years or older with pancreatic and biliary diseases? Hepatogastroenterology. 2013;60:1251-1256. [PubMed] |
| 8. | Sakai Y, Tsuyuguchi T, Mikata R, Tawada K, Tada M, Togo S, Tamura R, Saito M, Kurosawa J, Ishihara T. Utility of placement of pancreatic duct spontaneous dislodgement stent for prevention of post-ERCP pancreatitis in patients with difficulty in selective biliary cannulation. Hepatogastroenterology. 2011;58:687-693. [PubMed] |
| 9. | Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, Horaguchi J, Takasawa O, Koshita S, Kanno Y, Ogawa T. Can pancreatic duct stenting prevent post-ERCP pancreatitis in patients who undergo pancreatic duct guidewire placement for achieving selective biliary cannulation? A prospective randomized controlled trial. J Gastroenterol. 2010;45:1183-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Sakai Y, Tsuyuguchi T, Mikata R, Sugiyama H, Yasui S, Eto R, Fujimoto T, Tamura R, Togo S, Tada M. Pancreatic duct guidewire-indwelling method for patients resistant to selective biliary cannulation and usefulness of pre-cut papillotomy following unsuccessful biliary cannulation with pancreatic duct guidewire-indwelling method. Hepatogastroenterology. 2011;58:698-704. [PubMed] |
| 11. | Kawaguchi Y, Ogawa M, Omata F, Ito H, Shimosegawa T, Mine T. Randomized controlled trial of pancreatic stenting to prevent pancreatitis after endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2012;18:1635-1641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Ito K, Fujita N, Noda Y, Kobayashi G, Obana T, Horaguchi J, Takasawa O, Koshita S, Kanno Y. Pancreatic guidewire placement for achieving selective biliary cannulation during endoscopic retrograde cholangio-pancreatography. World J Gastroenterol. 2008;14:5595-5600; discussion 5599. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 13. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] |
| 14. | Tsuchiya T, Itoi T, Maetani I, Shigoka H, Ikeuchi N, Umeda J, Sofuni A, Itokawa F, Ishii K, Kurihara T. Effectiveness of the J-Tip Guidewire for Selective Biliary Cannulation Compared to Conventional Guidewires (The JANGLE Study). Dig Dis Sci. 2015;60:2502-2508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 15. | Omuta S, Maetani I, Shigoka H, Gon K, Saito M, Tokuhisa J, Naruki M. Newly designed J-shaped tip guidewire: a preliminary feasibility study in wire-guided cannulation. World J Gastroenterol. 2013;19:4531-4536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Kawakami H, Maguchi H, Mukai T, Hayashi T, Sasaki T, Isayama H, Nakai Y, Yasuda I, Irisawa A, Niido T. A multicenter, prospective, randomized study of selective bile duct cannulation performed by multiple endoscopists: the BIDMEN study. Gastrointest Endosc. 2012;75:362-372, 372.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 17. | Nambu T, Ukita T, Shigoka H, Omuta S, Maetani I. Wire-guided selective cannulation of the bile duct with a sphincterotome: a prospective randomized comparative study with the standard method. Scand J Gastroenterol. 2011;46:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |