Published online Aug 16, 2016. doi: 10.12998/wjcc.v4.i8.202
Peer-review started: February 18, 2016
First decision: March 24, 2016
Revised: April 7, 2016
Accepted: June 14, 2016
Article in press: June 16, 2016
Published online: August 16, 2016
Processing time: 176 Days and 13 Hours
AIM: To study patient outcomes after surgical correction for iatrogenic patellar instability.
METHODS: This retrospective study looked at 17 patients (19 knees) suffering from disabling medial patellar instability following lateral release surgery. All patients underwent lateral patellofemoral ligament (LPFL) reconstruction by a single surgeon. Assessments in all 19 cases included functional outcome scores, range of motion, and assessment for the presence of apprehension sign of the patella to determine if LPFL reconstruction surgery was successful at restoring patellofemoral stability.
RESULTS: No patients reported any residual postoperative symptoms of patellar instability. Also no patients demonstrated medial patellar apprehension or examiner induced subluxation with the medial instability test described earlier following LPFL reconstruction. Furthermore, all patients recovered normal range of motion compared to the contralateral limb. For patients with pre and postoperative outcome scores, the mean overall knee injury and osteoarthritis outcome score increased significantly, from 34.39 preoperatively (range: 7.7-70.12) to 69.54 postoperatively (range: 26.82-91.46) at final follow-up (P < 0.0001).
CONCLUSION: This novel technique for LPFL reconstruction is effective at restoring lateral restraint of the patellofemoral joint and improving joint functionality.
Core tip: This is a case series of patients presenting with an initial history of anterior knee pain who underwent lateral capsular surgical release procedure at an outside institution. They were referred to us after a dramatic increase in their knee problems following this procedure, including recurrent medial patellar instability and pain. There are two techniques in the current literature that describe lateral patellofemoral ligament reconstruction. Here we present a third technique, as well as the specific physical examination that indicated each patient for surgery. This is an important topic because of the debilitating nature of these iatrogenic symptoms, and the 100% relief of medial patellar subluxation we were able to accomplish in the postoperative period.
- Citation: Beckert M, Crebs D, Nieto M, Gao Y, Albright J. Lateral patellofemoral ligament reconstruction to restore functional capacity in patients previously undergoing lateral retinacular release. World J Clin Cases 2016; 4(8): 202-206
- URL: https://www.wjgnet.com/2307-8960/full/v4/i8/202.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i8.202
Lateral retinacular release (LR) is an arthroscopic or open procedure of the lateral patellofemoral ligament (LPFL) and capsule designed to relieve pressure in the joint for some patients presenting clinically with anterior knee pain. Indications leading surgeons to pursue LR include anterior knee pain secondary to a “tight lateral band”, chondromalacia patella, and “patellofemoral syndrome”. Once a common procedure, LR can leads to unfavorable outcomes namely medial apprehension of the patella, which was first reported in the literature by Hughston and Deese[1]. While it is unclear how many LR procedures are performed today, the purpose of this case series is illustrate several patients referred to our tertiary care center with a dramatically worsened clinical presentation immediately following LR due to recurrent medial subluxations.
Medial subluxation is a debilitating condition characterized by the patella translating horizontally out of the trochlear groove in the medial direction, in this case due to the compromised lateral restraints during LR surgery. Hughston et al[2] reported 85% of patients suffering from medial patellar subluxation could not perform “light recreational activities”, and 69% of patients had “severe” or “disabling” knee pain. It is for these reasons why patients seek treatment to decrease pain and increase function. Previous studies have shown LPFL reconstruction in patients with iatrogenic medial patellar instability significantly improved pain and functionality[3,4].
Two techniques currently describe LPFL reconstruction in the literature. Teitge et al[5] describes a technique using a patellar tendon graft, while Saper and Shneider[6] describe a technique using a quadriceps tendon graft. Using a third technique described below, it is hypothesized that restoration of the lateral capsule and LPFL will solve the sudden deteriorated state that followed the excessive lateral release in the immediate postoperative period. We also look to explore specific preoperative clinical exam findings that indicate the patient will significantly benefit from LPFL reconstruction.
This was a retrospective case series done at the University of Iowa, with all data obtained by a single investigator (Beckert MW) following Institutional Board Review (IRB) approval between July 2013 and August 2014. Data was collected during standard follow-up care in an outpatient clinic setting, however three patients had no record of post-operative functional outcome scores and these were administered by telephone. All patients were seen clinically for follow-up after LPFL reconstruction, with an average final follow-up of 2.05 years. The senior author (Albright JP) identified the study population during the patient’s clinical evaluation for symptoms following LR. Clinical evaluations were conducted by Albright JP in all cases. Twenty-three consecutive LPFL reconstructions following LR conducted between 2009 and 2014 were eligible for the study. All patients demonstrated medial apprehension of the patella preoperatively, and a majority experienced frank medial subluxation. The study excluded patients with concurrent lateral patellar apprehension to focus on the iatrogenic medial instability caused by prior lateral release.
Chief complaints during preoperative evaluation were pain, instability, and frank medial patellar subluxations or dislocations, frequently while walking on flat ground. The diagnosis of medial subluxation is made by beginning with the leg relaxed in full extension. The examiner then pushes and holds the patella in a medial position as the free hand is placed in the popliteal space and passively flexes the patient’s knee with relaxed quadriceps. Within the first 20-30 degrees the examiner observes a biomechanical acceleration (“jerk”) as the patella slides back into the trochlear groove as the knee is flexed further. This “jerk” is recognized by the patient as what happens to them frequently; often with every step as they are walking. This is opposed to the smooth re-entry gliding of a non-subluxating patella that can be observed in the patient’s opposite leg. The process is then repeated with the leg again starting relaxed in full extension, pushing the patella medially and then ask the patient to actively create an active quadriceps contraction prior to the passive flexion of the knee. Here it is observed that muscle contraction aligns the extensor mechanism to the point that there is smooth patellar movement back into the trochlear groove when the knee is subsequently flexed by the examiner. A similar examination and technique was previously described by Fulkerson[7].
In addition to medial patellar subluxation and/or apprehension, two clinical indications were used by the senior author to pursue LPFL reconstruction. In all instances, patients experienced at least some noticeable improvement in joint functionality from using a patellar-stabilizing sleeve with a medial buttress and walking across the exam room. Additionally, in some patients the examiner could restore patellar stability and decrease pain by placing a finger medially on their patella during gait. Both scenarios provided objective evidence that LPFL reconstruction would prove beneficial for the patient.
An initial incision was made lateral to the patella, dissecting down to the lateral retinaculum, allowing the exposure of both the patellar surface and posterior surface of the lateral femoral condyle. In all cases a loose encapsulated layer of scar tissue was filling the gap between the edges of the capsule. A lateral parapatellar arthrotomy was performed by incising this scar tissue. At that point the soft tissues of the joint were inspected. It was determined whether or not the re-approximation of the edges of the lateral retinaculum might cause too much tension on the patellofemoral articulation. Therefore, the reconstruction procedure was performed with an allograft hamstring tendon.
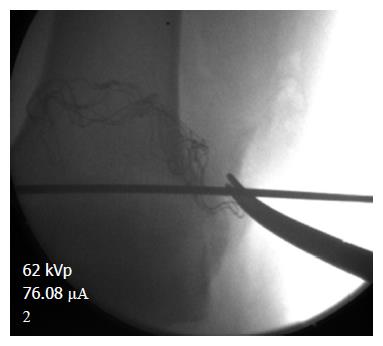
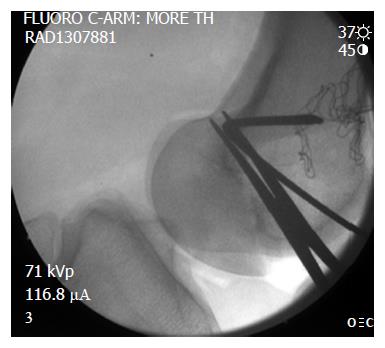
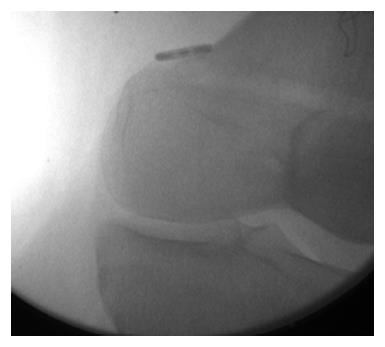
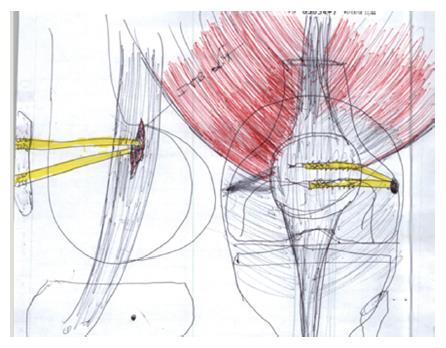
LPFL reconstruction was conducted using fluoroscopy to check the start position of the guide pin, placed in the lateral femoral epicondyle in an isometric point that mimics the ideal location of an medial patellofemoral ligament (MPFL) reconstruction (Figure 1). This location is confirmed by: (1) position of the entrance tunnel from lateral X-ray compared to the Blumensaat line and the posterior cortex in that area (Figure 2); (2) checking the isometry of the potential graft from 100 degrees of flexion out to full extension; and (3) stimulation of the femoral nerve to achieve quadriceps contraction as described by McDermott et al[8]. The length between the guide pin entry point and the patella was checked from extension to flexion using a free suture and allograft, proceeding once satisfied. The extensor muscle was stimulated via femoral nerve catheter with the leg in full extension to access the effect of the quadriceps activity on the length of the graft itself. The semitendinosus allograft was secured to the lateral femoral condyle using an EndoButton type device fixed on the medial femoral condyle (Figure 3). The allograft was then sutured to the patella in isometric position with the knee in flexion, using a FiberWire and Krachow suture. The graft was passed through the EndoButton loop to allow a two-tailed graft suturing as described by Csintalan et al[9] for MPFLs. A decompression window was created in the iliotibial band at the femoral origin of the LPFL reconstruction as it exited the femoral condyle on its way to the patella (Figure 4). This prevents the anterior and posterior motion that occurs naturally with the iliotibial band from interfering with the reconstruction. Once the graft was in place the isometry was then checked as well as the quadriceps activity on the length of the graft. The FiberWire attached to the allograft was securely fixed to the anterior aspect of the patella with no bone suture anchors. After observing neutral patella tracking through a full range of motion with an absence of medial apprehension, wounds were thoroughly irrigated and closed with a 2-0 Vicryl suture.
There have been reports of simply reattaching the capsule, however in this series we chose to reconstruct the LPFL allograft, because reattachment of the atrophied sides of the release was thought to create too much patellofemoral tension in these cases.
Patients began passive and active motion on the first postoperative day with the goal of reaching 90 degrees by 14 d postoperative. Patients were locked in extension in a hinged brace during ambulation and sleeping for the first 2 wk postoperatively. Active straight leg raising and eccentric quadriceps contraction allowing knee flexion to occur as far as tolerated were also encouraged starting early after surgery.
All patients returned to clinic for postoperative physical examination. During physical examination, testing for both medial apprehension and subluxation was conducted, as described previously. Other outcomes included range of motion assessed by the senior author and knee injury and osteoarthritis outcome scores (KOOS) survey questionnaire[8]. Physical examination data used in the study was taken during patient’s most recent follow-up appointment.
Between August 2009 and August 2014, the senior author (Albright JP) performed LPFL reconstruction with or without partial synovectomy and plicectomy on 20 patients (23 knees) who previously had LR surgery done at an outside institution. Two patients were excluded from the study due to both medial and lateral patellar instability, while a third patient declined to participate in the study when contacted. This brought the total study population to 17 patients (19 knees). The average patient age at the time of LPFL reconstruction was 29.46 years (15.4-54.35). There were 18 females and one male. All patients completed postoperative physical examination. Postoperative KOOS were obtained for 89.5% of patients. Twelve of the 19 knees (63.2%) had both pre and postoperative KOOS scores available for statistical comparison using one-way T scores. The threshold for statistical significance was P < 0.05[10].
No patients reported any residual postoperative symptoms of patellar instability. Also no patients demonstrated medial patellar apprehension or examiner induced subluxation with the medial instability test described earlier following LPFL reconstruction. Furthermore, all patients recovered normal range of motion compared to the contralateral limb. For patients with pre and postoperative outcome scores, the mean overall KOOS score increased significantly, from 34.39 preoperatively (range: 7.7-70.12) to 69.54 postoperatively (range: 26.82-91.46) at final follow-up (P < 0.0001).
LR surgeries extensive enough to compromise the lateral restraints of the patella can indeed lead to medial patellar subluxation. Although the quadriceps muscles can provide stability by contracting to keep the patella within the trochlear groove in some circumstances such as getting up out of chairs or walking stairs, on flat surfaces these muscles are normally silent during the swing phase of gait, allowing the patella to drift medially into a subluxed position. As the knee passively flexes in subsequent stages, the patella violently re-enters the groove as seen clinically during the novel subluxation exam in our patients as described above. These patients had great difficulty with the mere act of walking on flat ground because their patella subluxes with nearly every step.
The restoration of the lateral capsule and LPFL was 100% effective in treating the sudden deteriorated state that followed the excessive lateral release in the immediate postoperative period by eliminating the patient’s medial apprehension. Reconstruction of the LPFL also significantly improved knee pain and function in these patients, as determined by: (1) the postoperative physical exam in all patients; (2) postoperative functional outcome scores; and (3) pre- vs postoperative outcome scores when available.
This study had a number of limitations. Although 17 of 19 knees completed postoperative outcome scores, only 12 knees completed both pre and postoperative outcome scores and were made available for data analysis. This only eliminated the quantification of how poorly patients were doing preoperatively, but from a clinical standpoint it was impressive beyond quantification. Their major complaint was that they had an operation for anterior knee pain but made dramatically worse following the procedure. Post LPFL reconstruction however, 89.5% patients completed functional outcome scores, and our findings agree with that of other literature analyzing the outcomes of restoring lateral restraint following LR surgery[3,4]. This, along with the fact that all 19 knees completed the physical exam portion of postoperative evaluation, leads us to believe the limitations of the data analysis did not have a major effect on our conclusions. Other outcome measures were also used to strengthen our findings, including range of motion, and the presence of medial apprehension and subluxation to objectively determine the success of LPFL reconstruction.
This is a case series of patients presenting with an initial history of anterior knee pain who had undergone a lateral capsular surgical release procedure. They were referred because of a dramatic increase in their knee problems due to an additional appearance of postoperative patellar instability. Our preoperative clinical exam assessment found that patellar instability existed, and the restoration of patellar stability with LPFL reconstruction led to a significant improvement in patient outcomes.
Patellar instability is a severely debilitating pathology of the patellofemoral joint that is relatively common, especially in adolescence. Lateral release is an arthroscopic or open procedure though to reduce tension on some of the lateral restraints of the knee that are believed to cause pain in some patients, but often causes unintended patellar instability. In these cases, it is imperative that lateral structures of the knee joint be repaired to correct for this recurrent medial instability.
The literature only supports two prior methods of lateral patellofemoral ligament (LPFL) reconstruction for iatrogenic patellar instability. The authors present a third technique along with outcome measures in a series of patients.
The authors’ results show favorable outcomes with the technique described for LPFL reconstruction and justifies its future use in this specific patient population.
This is an important topic with excellent results of the described technique.
Manuscript source: Invited manuscript
Specialty type: Medicine
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Andrish J, Shneider DA S- Editor: Qiu S L- Editor: A E- Editor: Zhang FF
| 1. | Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16:383-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 153] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Hughston JC, Flandry F, Brinker MR, Terry GC, Mills JC. Surgical correction of medial subluxation of the patella. Am J Sports Med. 1996;24:486-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Sanchis-Alfonso V, Montesinos-Berry E, Monllau JC, Merchant AC. Results of isolated lateral retinacular reconstruction for iatrogenic medial patellar instability. Arthroscopy. 2015;31:422-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Heyworth BE, Carroll KM, Dawson CK, Gill TJ. Open lateral retinacular closure surgery for treatment of anterolateral knee pain and disability after arthroscopic lateral retinacular release. Am J Sports Med. 2012;40:376-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Teitge RA, Torga Spak R. Lateral patellofemoral ligament reconstruction. Arthroscopy. 2004;20:998-1002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Saper MG, Shneider DA. Lateral Patellofemoral Ligament Reconstruction Using a Quadriceps Tendon Graft. Arthrosc Tech. 2014;3:e445-e448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447-456. [PubMed] |
| 8. | McDermott SE, Anthony CA, McCunniff P, Duchman K, Albright JP. A clinical and radiographic approach for establishing proper tibial tubercle transfer when using quad active femoral nerve stimulation. Iowa Orthop J. 2013;33:84-89. [PubMed] |
| 9. | Csintalan RP, Latt LD, Fornalski S, Raiszadeh K, Inacio MC, Fithian DC. Medial patellofemoral ligament (MPFL) reconstruction for the treatment of patellofemoral instability. J Knee Surg. 2014;27:139-146. [PubMed] |
| 10. | Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S208-S228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 672] [Cited by in RCA: 873] [Article Influence: 67.2] [Reference Citation Analysis (0)] |