Published online Jul 16, 2016. doi: 10.12998/wjcc.v4.i7.177
Peer-review started: February 23, 2016
First decision: March 25, 2016
Revised: March 30, 2016
Accepted: May 10, 2016
Article in press: May 11, 2016
Published online: July 16, 2016
Processing time: 139 Days and 12.6 Hours
Colitis cystic profunda is a rare entity benign condition of the colon and rectum that can mimic suspicious polyps or malignancy. The commonest sites of affectation are the rectum and the sigmoid colon but it can be unusually widely distributed in the colon. The aetiology of this condition is not fully elucidated and confident diagnosis can only be made on histological features. We hereby describe a patient who presented with significant rectal symptoms and an unexpected finding of a submucosal mucous cyst mimicking a suspicious rectal polyp and highlighted its significance and the review of the literature.
Core tip: Colitis cystic profunda is although rare but it is important that it is not mistaken for a mucinous adenocarcinoma, carcinoid tumour, pancreatic heterotopia, inverted or pseudo-invasion of adenomatous polyp of the anorectum for the purposes of treatment and prognostication.
- Citation: Ayantunde AA, Strauss C, Sivakkolunthu M, Malhotra A. Colitis cystica profunda of the rectum: An unexpected operative finding. World J Clin Cases 2016; 4(7): 177-180
- URL: https://www.wjgnet.com/2307-8960/full/v4/i7/177.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i7.177
Colitis cystic profunda (CCP) is a rare and uncommon benign lesion of the colon and rectum characterised by the presence of intramural or submucosal mucous containing cysts. Although it may diffusely involve the entire large bowel, the classical sites are usually in the rectum and sigmoid colon. Knowledge of this pathological entity is necessary and important as it can clinically and histological mimic a malignant lesion[1-3]. The aetiology of this rare condition is unclear and the diagnosis is usually by histology[1-3]. The first description of the lesions was by Stark[4] who found mucous cysts in the colon of two patients at autopsy who died of dysentery. Virchow later introduced the term “CCP” following a report of multiple polypoid cystic submucosal lesions[5]. We describe a case of a lady with rectal symptoms and a submucosal mucous cyst mimicking a suspicious rectal polyp and highlighted its significance and the review of the literature.
A 34-year-old lady presented with a history of recurrent fresh rectal bleeding for the past few years and associated more recently with mucus discharge and tenesmus. Apart from diarrhea-predominant irritable bowel syndrome she had no significant past medical problem and no family history of bowel pathology. Anorectal examination and rigid sigmoidoscopy revealed multiple rectal polyps with a particularly predominant one measuring about 3 cm on the right lateral wall of the rectum.
Flexible sigmoidoscopy confirmed a polypoid lesion in the rectum which turned out to be the previously noted 3 cm polyp on the lateral wall of the rectum (Figures 1 and 2). Histology of the multiple biopsies from this lesion and other multiple rectal polyps were reported as a “benign hyperplastic polyp with no dysplasia or malignancy”. She subsequently underwent an examination under anesthesia showing a 3-cm submucosal lesion in the right lateral rectal wall with a central pit. There were findings of a small rectocele and rectal mucosal prolapse in addition to the submucosal lesion. A careful excision was achieved by raising the submucosal layer with 0.5% lignocaine and 1 in 200000 adrenaline. Two/zero vicryl stay sutures at the superior and inferior margins were used for retraction to aid excision. A complete excision was achieved through a vertical mucosal incision dissecting the lesion wholemeal from the submucosal layer (Figure 2). The excised lesion was found to be a cystic lesion containing mucus (Figure 3).
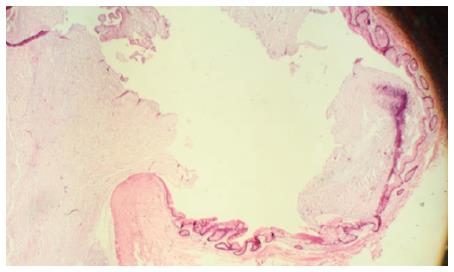
The H and E stain of the lesion confirmed cyst lined by atrophic colonic mucosa and colonic mucinous epithelium with surrounding fibrosis. The overlying mucosa shows some degree of benign hyperplasia. The cyst contains inspissated mucin with dystrophic calcification. The cyst extends into the submucosal tissue and up to the muscular layer but no evidence of dysplasia or malignancy is seen (Figure 4).
CCP is a rare benign condition involving the rectum and colon often presenting as a polypoid lesion[1-3]. This entity is of clinical significance in that it can often mimics malignant lesions of the colorectum to which it must be distinguished[1]. The aetiology of this entity is unknown but there is a proposed theory of congenital origin. It has been found to be associated with several acquired conditions such as rectal prolapse, solitary rectal ulcer (SRU), inflammatory bowel disease, diverticulitis, local rectal trauma and adenocarcinoma[1-12].
Pathologically, CCP is a benign lesion characterized by mucin filled cysts beneath the muscularis mucosa. Its distribution can be in localized form with a polypoidal lesion or in a more diffuse pattern with variable length of the rectal mucosa or colon involved[9]. Both of these patterns of distributions have been well described in the setting of acquired conditions causing mucosal ulceration and inflammation[7]. The localized form has been reported in associated with solitary rectal ulcer syndrome, rectal prolapse[1,10,12] while the more diffuse types have been described in patients with Crohn’s disease, ulcerative colitis, radiation, and infectious colitis[7,11]. Mitsunaga et al[8] recently reported a case of a single polypoid CCP lesion in association with an adenocarcinoma. Therefore, a careful histopathological examination of all CCP specimens is advisable to exclude an associated malignancy.
The most common symptoms of this pathology include fresh rectal bleeding, mucus discharge, tenesmus, proctalgia fugax, altered bowel habits and a long existing history of obstructive defecation[2,8,12]. There are no peculiar characteristics of CCP on endoscopy. Endoscopic features are usually those of polypoid lesion covered by a normal, oedematous or ulcerated mucosa. Endoscopic anorectal ultrasound where available can be diagnostic as it shows a hypoechoic signal usually in the submucosal layer with no surrounding deeper layer infiltration. These important features distinguish it from malignancy of the anorectum[12]. Computerized tomography scan and/or magnetic resonance imaging typically reveal non-infiltrating submucosal cystic lesion with some loss of perirectal fatty tissue and thickening of levator ani muscles[1,13]. These imaging may show features of SRU and pelvic floor dysfunction. Anorectal physiology studies including evacuatory proctography have been reported to document rectal intussusceptions in up to 45%-80% of patients with localised CCP[14]. Features of localised CCP of the rectum are in most cases not distinguishable from those of SRU as they tend to have similar underlying factors including evacuatory dysfunction and rectal mucosal prolapse. However, this relationship between CCP and SRU is not always demonstrable in all patients. Association of rectal prolapse has been reported in up to 54% of localised CCP[1,15].
Treatment of CCP is mostly conservative and surgery is only indicated in patients with severe symptoms with associated significant rectal prolapse. First-line management option should commence with dietary and lifestyle changes. This is aim at avoiding constipation and straining during defecation. This treatment regime can be aided by the use of bulking laxatives, stool softeners and lubricants, hydrocortisone enemas and sucralfate[7,14]. Bowel retraining with biofeedback therapy may be successful in some group of patients[16]. Patients who fail to respond to conservative measures, with persistent, relapsing symptoms, obstructive defecation and full thickness rectal prolapse or where the initial diagnosis is not definite should be considered for surgery. Operative options include transanal excision of CCP as in this reported case, rectal mucosal excision (Delorme’s operation), perineal rectosigmoidectomy (Altemeier’s operation) with coloanal anastomosis, stapled transanal resection of rectum (STARR procedure) or abdominal approach laparoscopic ventral rectopexy[2,13,17].
Although CCP is rare, it is important to be aware of this clinical and pathologic entity so that it is not mistaken for a mucinous adenocarcinoma, carcinoid tumour, pancreatic heterotopia, inverted or pseudo-invasion of the adenomatous polyp of the anorectum for the reasons of therapy and prognosis.
A 34-year-old lady presented with significant rectal symptoms and an unexpected finding of a subucosal mucous cyst mimicking a suspicious rectal polyp.
A suspected 3 cm rectal mucosal polypoid lesion on the right lateral wall on sigmoidoscopy and at examination under anaesthesia.
Mucinous adenocarcinoma, carcinoid tumour, pancreatic heterotopia, inverted or pseudo-invasion of the adenomatous polyp of the anorectum.
Histopathology with H and E of the lesion confirmed cyst lined by atrophic colonic mucosa and colonic mucinous epithelium with surrounding fibrosis. The overlying mucosa shows some degree of benign hyperplasia. The cyst contains inspissated mucin with dystrophic calcification. The cyst extends into the submucosal tissue and up to the muscular layer but no evidence of dysplasia or malignancy is seen. These features are in keeping with colitis cystica profunda.
Complete surgical excision of lesion.
Colitis cystic profunda (CCP) is a rare and uncommon benign lesion of the colon and rectum characterised by the presence of intramural or submucosal mucous containing cysts. Knowledge of this pathological entity is necessary and important as it can clinically and histological mimic a malignant lesion.
CCP was first described as mucous cyst lesion by Stark. Virchow later introduced the term CCP.
This pathological entity can be confused with mucinous adenocarcinoma, carcinoid tumour, pancreatic heterotopia, inverted or pseudo-invasion of the adenomatous polyp of the anorectum. Knowledge of this entity is therefore important to the clinician in guiding therapeutic intervention.
This is a well written case report, with adequate review of the literature. It is important to consider CCP in the differential of rectal submucosal lesions.
Manuscript source: Invited manuscript
P- Reviewer: Delladetsima IK, Naito Y, Qayed E S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Kayaçetin E, Kayaçetin S. Colitis cystica profunda simulating rectal carcinoma. Acta Chir Belg. 2005;105:306-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Guest CB, Reznick RK. Colitis cystica profunda. Review of the literature. Dis Colon Rectum. 1989;32:983-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Kornprat P, Langner C, Pfeifer J, Mischinger HJ. Colitis cystica profunda associated with rectal prolapse: report of a case. Int J Colorectal Dis. 2007;22:1555-1556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Stark W. Specimen septemhistoriaset dissections dysentoricumexhibens (thesis). The Netherelands: Leiden 1966; . |
| 5. | Virchow R. Die KrankhaftenGeschwulste. Berlin: Hirschwald 1963; . |
| 6. | de Toro C G, Villaseca H M, Roa S JC. Colitis cystica profunda: report of one case. Rev Med Chil. 2007;135:759-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Madan A, Minocha A. First reported case of colitis cystica profunda in association with Crohn’s disease. Am J Gastroenterol. 2002;97:2472-2473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Mitsunaga M, Izumi M, Uchiyama T, Sawabe A, Tanida E, Hosono K, Abe T, Shirahama K, Kanesaki A, Abe M. Colonic adenocarcinoma associated with colitis cystica profunda. Gastrointest Endosc. 2009;69:759-760; discussion 760-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Qayed E, Srinivasan S, Wehbi M. A case of colitis cystica profunda in association with diverticulitis. Am J Gastroenterol. 2011;106:172-173. [PubMed] |
| 10. | Wang F, Frisbie JH, Klein MA. Solitary rectal ulcer syndrome (colitis cystica profunda) in spinal cord injury patients: 3 case reports. Arch Phys Med Rehabil. 2001;82:260-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Toll AD, Palazzo JP. Diffuse colitis cystica profunda in a patient with ulcerative colitis. Inflamm Bowel Dis. 2009;15:1454-1455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Higuera Alvarez R, García Jde L, San Miguel G, Castro B. [Colitis cystica profunda]. Rev Esp Enferm Dig. 2008;100:240-242. [PubMed] |
| 13. | Valenzuela M, Martín-Ruiz JL, Alvarez-Cienfuegos E, Caballero AM, Gallego F, Carmona I, Rodríguez-Téllez M. Colitis cystica profunda: imaging diagnosis and conservative treatment: report of two cases. Dis Colon Rectum. 1996;39:587-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Dolar E, Kiyici M, Yilmazlar T, Gürel S, Nak SG, Gülten M. Colitis cystica profunda. Turk J Gastroenterol. 2007;18:206-207. [PubMed] |
| 15. | Abid S, Khawaja A, Bhimani SA, Ahmad Z, Hamid S, Jafri W. The clinical, endoscopic and histological spectrum of the solitary rectal ulcer syndrome: a single-center experience of 116 cases. BMC Gastroenterol. 2012;12:72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | Vaizey CJ, Roy AJ, Kamm MA. Prospective evaluation of the treatment of solitary rectal ulcer syndrome with biofeedback. Gut. 1997;41:817-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 17. | Beck DE. Surgical Therapy for Colitis Cystica Profunda and Solitary Rectal Ulcer Syndrome. Curr Treat Options Gastroenterol. 2002;5:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |