Published online Apr 16, 2016. doi: 10.12998/wjcc.v4.i4.108
Peer-review started: October 14, 2015
First decision: November 11, 2015
Revised: December 6, 2015
Accepted: January 8, 2016
Article in press: January 11, 2016
Published online: April 16, 2016
Processing time: 184 Days and 12.2 Hours
An unusual case of long standing sclerosing mesenteritis; initially presented with recurrent abdominal pain and a mesenteric mass with surrounding fat oedema and stranding with a pseudocapsule and fat ring sign were clearly visualised on the initial computed tomography scan. Laparotomy showed diffuse thickening at the root of the mesentery and histology from this specimen revealed fat necrosis and reactive lymphoid tissue consistent with sclerosing mesenteritis. Initial treatment with steroids and tamoxifen relieved the symptoms and the mass. He was maintained on tamoxifen. Three years later he developed a recurrence of his symptoms and abdominal mass that responded to a course of steroids. Two years following this, he developed a follicular Hodgkin’s lymphoma.
Core tip: Sclerosing mesenteritis is a rare disease but clinicians should be mindful of this condition that can present with various clinical symptoms including recurrent abdominal pain. The case we describe showed typical features of sclerosing mesenteritis and demonstrated good clinical and radiological response to steroids and tamoxifen. Five years later he developed a recurrence of the abdominal mass that showed transformation into a lymphoma.
- Citation: Shah S, Mahy G, Roche E. Rare case of sclerosing mesenteritis and low grade follicular lymphoma. World J Clin Cases 2016; 4(4): 108-111
- URL: https://www.wjgnet.com/2307-8960/full/v4/i4/108.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i4.108
Sclerosing mesenteritis also known as mesenteric lipodystrophy and mesenteric panniculitis is the part of the spectrum of idiopathic primary inflammatory and fibrotic process that affects mesentery[1]. This is a relatively rare condition with clinical data limited only to case reports. It has a male preponderance and generally occurs in the sixth and seventh decades of life. Pathophysiology remains unknown and various mechanisms like trauma (including surgery), autoimmune, malignant and paraneoplastic causes have been postulated. There is an association with lymphoma, breast cancer, lung cancer, melanoma and colon cancer[1-4]. In one study, prior abdominal surgery was present in about 35% of patients. There have been no reports of sclerosing mesenteritis transforming into a lymphoma, although in one case both of these lesions coexisted. We report an unusual case of long standing sclerosing mesenteritis that subsequently progressed to a follicular Hodgkin’s lymphoma.
We report a case of a 63-year-old man who presented to our department five years ago, with a five-year history of recurrent abdominal pain that had recently worsened. It was constant and increased in intensity on lying down and radiated into his back. He denied vomiting, weight loss or anorexia.
He was known to have Metabolic syndrome and his past surgical history included: (1) a laparotomy done over 10 years ago for probable cyst on pancreas; the details were not available; and (2) cholecystectomy, 5 years ago for calculus cholecystitis. On examination of his abdomen there was a long mid-line scar, mild abdominal tenderness and an impression of an ill-defined mass in his mid abdomen.
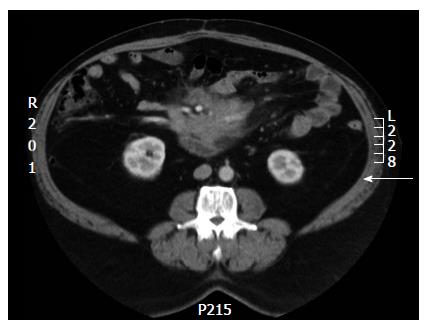
No abnormalities were noted on routine blood work up. IgG 4 and platelet serotonin were within normal limits. Computerized tomography (CT) scan of the abdomen showed a mesenteric mass with surrounding fat oedema and stranding. It was encasing superior mesenteric vessels and extending superiorly to the uncinate process. A pseudocapsule and fat ring sign were clearly visualised (Figure 1).
He had a laparotomy that showed diffuse thickening at the root of the mesentery that did not feel hard. On incising the peritoneum there was no discrete mass evident, though some discolouration and sclerosis of fat was present. There was no intra-abdominal lymphadenopathy. The histology from this specimen revealed fat necrosis and reactive lymphoid tissue. The features were consistent with sclerosing mesenteritis.
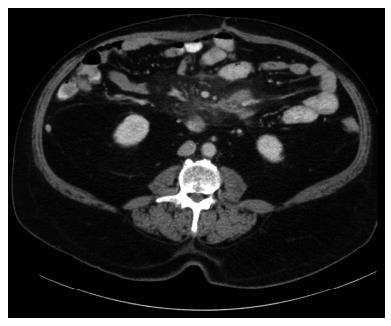
He was commenced on prednisolone 50 mg daily and Tamoxifen 10 mg twice a day and noticed significant improvement in his clinical symptoms. His steroids were tapered and discontinued and he continued on Tamoxifen 10 mg daily. He remained well and a repeat CT scan had shown a significant improvement (Figure 2).
Three years later he developed an exacerbation of his symptoms and imaging demonstrated a recurrence of the mass. He was retreated with oral steroids and Tamoxifen was increased to 10 mg twice a day. He responded clinically and radiologically.
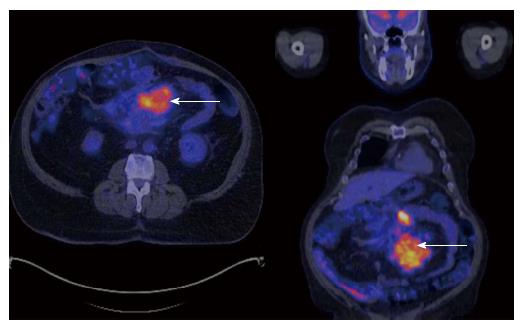
Two years later, he had a further recurrence in his symptoms. CT scans showed an increase in size and a change in characteristics of the mass. Positron emission tomography (PET) scan showed an intensely fluorodeoxyglucose avid heterogeneous nodal masses in the mesentery and adjacent para-aortic and aorto-caval nodes that were suspicious for a malignant process (Figure 3). He underwent a mini laprotomy for mesenteric mass biopsy. Histology revealed a follicular lymphoma/nodular sclerosing Hodgkin’s disease and he has been commenced on treatment.
The clinical presentation of Sclerosing mesenteritis varies from asymptomatic incidental diagnosis to various clinical features including abdominal pain, vomiting, diarrhoea, constipation, anorexia, weight loss, fatigue, fever of unknown origin, ascites, pneumoperitonium, pleural and pericardial effusion[1-6].
The diagnosis of sclerosing mesenteritis requires appropriate clinical and radiological analysis with multidetector CT and MRI being the modality of choice. Biopsy is necessary for definitive diagnosis. The two main CT features are the “fat ring” sign consisting of area of fat around the mesenteric vessels and presence of a pseudocapsule around the tumour. Other CT findings consist of increased attenuation in mesentery, foci of fat necrosis and fibrosis appearing as low-attenuation areas and a solid mass encasing the mesenteric vessels[7,8]. Magnetic resonance imaging and PET scans are upcoming modalities used to diagnose this condition. A negative PET has a high diagnostic accuracy in excluding tumoural mesenteric involvement while increased uptake suggests the co-existing mesenteric deposits, particularly in patients with lymphoma[9,10].
Management of sclerosing mesenteritis is based on expert opinion with no recognised standard therapy. Treatment is generally guided by symptoms. Various treatments have been mentioned in case reports including immunosuppressive therapy with glucocorticoid and tamoxifen as first line therapy while colchicine, azathioprine or cyclophosphamide may be used as adjunct therapy. For refractory cases thalidomide can be considered. Surgery and radiation therapy both have a limited role. Surgery is best reserved for obstructive cases. The largest series was published from the Mayo Clinic in 2007 and based on their advice it is recommended that tamoxifen be continued indefinitely as the rate of recurrence and complications is significant[5]. A combination of steroids (40-60 mg) and Tamoxifen 10 mg BD tapered over three months has been the regimen most widely used. Tamoxifen apparently decreases inflammation and down regulates fibroblast proliferation[1-5,10].
The case we describe showed typical features of sclerosing mesenteritis and demonstrated good clinical and radiological response to steroids and tamoxifen. Over the years he had follow up by imaging techniques to check the progress of mesenteric mass after treatment with Tamoxifen and steroids to which he responded well initially. Three years later he developed an exacerbation of his symptoms and a recurrence of the abdominal mass on imaging that was treated again with steroids and tamoxifen. After 5 years he presented with recurrent symptoms and increase in size and a change in characteristics of the mass that was proved to be follicular Hodgkin’s Lymphoma on histology.
A 63-year-old man with metabolic syndrome and previous abdominal surgery presented with a five-year history of recurrent abdominal pain that had recently worsened.
There was a long mid-line scar, mild abdominal tenderness and an impression of an ill-defined mass in his mid-abdomen.
Differential diagnosis is quiet broad and includes multiple causes of recurrent abdominal pain and abdominal masses including any intra-abdominal malignancy, carcinomatosis, lymphoma, pancreatitis, retroperitoneal fibrosis, vasculitis and granulomatous diseases.
All laboratory investigations were within normal limits.
Initial computerised tomography scan of the abdomen showed a mesenteric mass with surrounding fat oedema, stranding and pseudocapsule with fat ring sign. Subsequent positron emission tomography scan on an intensely fluorodeoxyglucose avid heterogeneous nodal masses in the mesentery and adjacent para-aortic and aorto-caval nodes that were suspicious for a malignant process.
Histology revealed a follicular lymphoma/nodular sclerosing Hodgkin’s disease.
He was commenced on prednisolone 50 mg daily and tamoxifen 10 mg twice a day for treatment of symptomatic sclerosing mesenteritis. Later on after the diagnosis of lymphoma he underwent chemotherapy.
In this study, the authors report a case of a man with a metabolic syndrome story. The patient got a dual treatment with glucocorticoid and tamoxifen which evolved through a lymphoma. This case study is interesting.
P- Reviewer: Langdon S, Poirot M S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Friedman LS. Sclerosing mesenteritis. UptoDate Topic 2602 Version 8.0. [updated 2013 Nov 25]. Available from: http//www.uptodate.com. |
| 2. | Taylor CR. An 83-Year-Old Man with Abdominal Pain, Nausea, and Weight Loss. Medscape, Mar 11, 2005. Available from: http://www.medscape.com/viewarticle/495063. |
| 3. | Ginsburg PM, Ehrenpreis ED. A pilot study of thalidomide for patients with symptomatic mesenteric panniculitis. Aliment Pharmacol Ther. 2002;16:2115-2122. [PubMed] [DOI] [Full Text] |
| 4. | Chawla S, Yalamarthi S, Shaikh IA, Tagore V, Skaife P. An unusual presentation of sclerosing mesenteritis as pneumoperitoneum: case report with a review of the literature. World J Gastroenterol. 2009;15:117-120. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Akram S, Pardi DS, Schaffner JA, Smyrk TC. Sclerosing mesenteritis: clinical features, treatment, and outcome in ninety-two patients. Clin Gastroenterol Hepatol. 2007;5:589-596; quiz 523-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 202] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 6. | Arora M, Dubin E. A clinical case study: sclerosing mesenteritis presenting as chylous ascites. Medscape J Med. 2008;10:30. [PubMed] |
| 7. | Daskalogiannaki M, Voloudaki A, Prassopoulos P, Magkanas E, Stefanaki K, Apostolaki E, Gourtsoyiannis N. CT evaluation of mesenteric panniculitis: prevalence and associated diseases. AJR Am J Roentgenol. 2000;174:427-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 206] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 8. | Horton KM, Lawler LP, Fishman EK. CT findings in sclerosing mesenteritis (panniculitis): spectrum of disease. Radiographics. 2003;23:1561-1567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 155] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 9. | Zissin R, Metser U, Hain D, Even-Sapir E. Mesenteric panniculitis in oncologic patients: PET-CT findings. Br J Radiol. 2006;79:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Iwanicki-Caron I, Savoye G, Legros JR, Savoye-Collet C, Herve S, Lerebours E. Successful management of symptoms of steroid-dependent mesenteric panniculitis with colchicine. Dig Dis Sci. 2006;51:1245-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |