Published online Dec 16, 2016. doi: 10.12998/wjcc.v4.i12.419
Peer-review started: May 17, 2016
First decision: July 11, 2016
Revised: August 16, 2016
Accepted: September 21, 2016
Article in press: September 22, 2016
Published online: December 16, 2016
Processing time: 205 Days and 16 Hours
Primary central nervous system lymphoma (PCNSL) is a rare disease in pediatric age group. A thirteen-year-old male child presented with complaints of headache for six months, vomiting and diplopia for three days. Magnetic resonance imaging of the brain showed a single lesion of 1.7 cm × 1.6 cm × 1.6 cm in the mid brain and tectum. He underwent a gross total resection of the tumor. The histopathological evaluation revealed B cell high grade non Hodgkin lymphoma. The patient was treated with High dose methotrexate and cranio spinal radiation. The patient was alive without disease 12 mo after completion of treatment. This case highlights importance of keeping PCNSL as differential in brain stem lesions of pediatric patients also. Radiation and chemotherapy remains the most important treatment for such patients.
Core tip: Primary central nervous system lymphoma (PCNSL) in pediatric population is an uncommon disease. In addition location in the brainstem is far less common. We are reporting a rare case of PCNSL in the brain stem location in a 13-year-old patient. Brain stem lesions are not generally considered for lymphoma. This case highlights importance of keeping brainstem lymphoma as a differential.
- Citation: Benson R, Mallick S, Purkait S, Suri V, Haresh KP, Gupta S, Sharma D, Julka PK, Rath GK. Primary pediatric mid-brain lymphoma: Report of a rare pediatric tumor in a rare location. World J Clin Cases 2016; 4(12): 419-422
- URL: https://www.wjgnet.com/2307-8960/full/v4/i12/419.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i12.419
Primary central nervous system lymphoma (PCNSL) most commonly occurs in the age group of 50-70 years and is rare in pediatric age group[1,2]. Tectum (midbrain) is a very rare site of PCNSL. Here were report a case of primary midbrain lymphoma in a 13-year-old child.
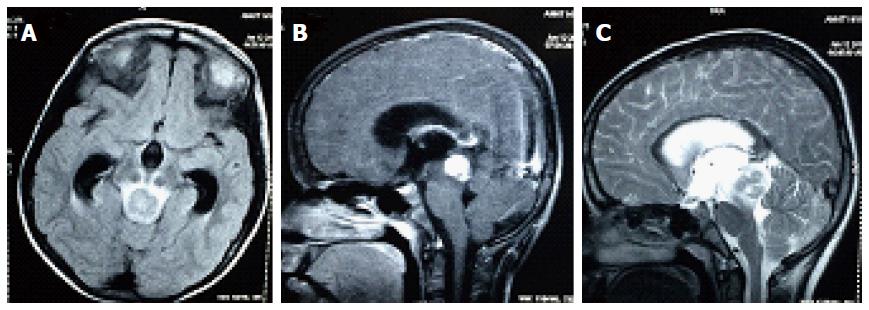
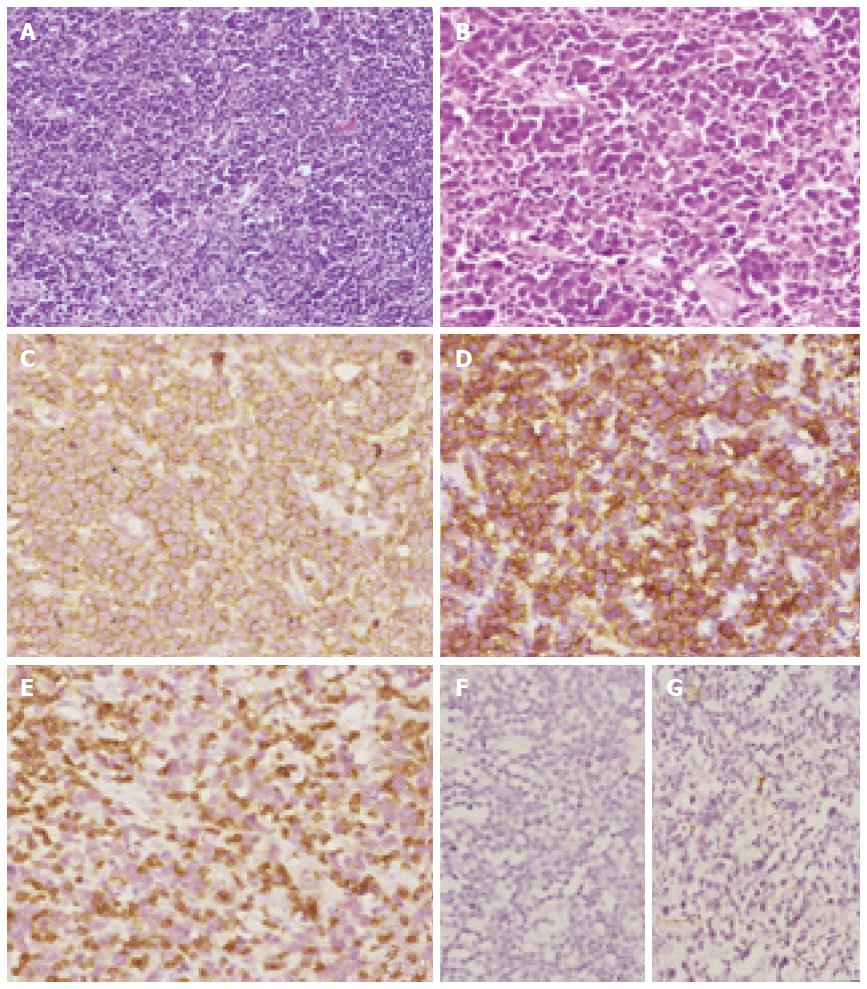
A 13-year-old male child was evaluated with complaints of headache for six months, vomiting and diplopia for three days. The child was evaluated with a contrast enhanced magnetic resonance imaging (MRI) of the brain which showed a single lesion 1.7 cm × 1.6 cm × 1.6 cm in the mid brain and tectum with intense contrast enhancement and hydrocephalus. The lesion was mildly hypo-intense in T1 and heterogeneously hyper-intense on T2W image with few hypo-intense areas. There was edema extending to mid part of pons (Figure 1). With a diagnosis of focal midbrain glioma, the patient underwent a ventriculo-peritoneal shunt and gross total excision of the tumor. Light microscopic examination of the lesion showed diffuse infiltration by atypical large lymphoid cells (immunopositive for leukocyte common antigen) having round nucleus with scanty cytoplasm. The cells are immunopositive for CD20 and CD79a (B-Cell markers) while negative for CD3 (T-Cell marker) and MPO (Myeloid marker). The histopathological evaluation revealed B cell high grade non Hodgkin lymphoma (Figure 2).
Postoperative MRI revealed no residual mass. MRI screening of the spine did not reveal any drop metastasis or lesion. Cerebro spinal fluid (CSF) cytology was done and showed lymphoma deposits. The bone marrow biopsy showed normal hematopoesis cell. Ophthalmic evaluation did not reveal any vitreous lesions and serology for HIV 1 and 2 was negative. Whole body positron emission tomography (PET-CT) showed no abnormal fluro-deoxy glucose avid areas except inflammatory lymph node in mesentery.
Patient was planned for adjuvant chemotherapy with high dose methotrexate. Methotrexate was given at a dose of 3.5 g/m2 with adequate hydration and Leucovorin rescue. The patient received 6 cycles of chemotherapy with high dose methotrexate and craniospinal irradiation. The dose of craniospinal irradiation planned was 36 Gray in 18 fractions over 3.5 wk followed by boost to the whole cranium for 9 Gray in 5 fractions over 1 wk. The patient is surviving without disease 1 year after treatment.
PCNSL is a very rare tumor in children. Pediatric cases account for about 1.5% of cases of primary CNS lymphoma reported to the brain tumor registry of Japan (1969-1990)[2]. Patients with human immune deficiency virus infection are at a higher risk for development of primary CNS lymphoma[3].
Pediatric PCNSL are different from adult group in that they are more frequently occurring in the posterior fossa (33.5% vs 9%) and have higher incidence of meningeal metastasis[4].
The majority of the patients of PCNSL have histology of diffuse large B-cell lymphoma (DLBCL). About 10% of the patients may have other histologies like Burkitts Lymphoma, indolent B-cell lymphomas and T cell lymphoma[1]. EBV may be seen associated with DLBCL of the CNS and may be more commonly associated in non-immune compromised patients[5]. Contrast enhanced MRI of the brain, spine screening MRI, CSF cytology, ophthalmic evaluation whole body CT/PET CT, viral markers are the important investigations in management of PCNSL.
It has been reported that adult PCNSL occurs in supra tentorial location in majority of patients with posterior fossa as a location of tumor only in 7% of the cases[6]. Only 3% cases have been reported to have a brainstem involvement and majority of such lesions are of T-cell lineage. Contrast enhanced MRI is the preferred imaging modality in these cases of PCNSL. Approximately 90% of these cases present with contrast enhancing lesions[6]. Ring like enhancement is rarely observed in immune competent patients, but commonly found in immune compromised patients[7]. The lesions may be multiple especially in immune compromised patients.
PCNSL is a highly radiosensitive and chemo sensitive infiltrative tumor. Steroids may be deferred till the diagnosis of PCNSL is confirmed. Surgery is helpful in confirming the diagnosis. A median survival of 4.6 mo has been reported for patients treated with surgical excision alone. Whole brain radiotherapy has conferred a median survival of 14.5-18 mo and a 5-year survival of 35%. However, patients treated with radiation alone experience early local failure. This finding paved for the combined modality therapy of chemotherapy and radiation therapy in sequential manner. Presently, high dose methotrexate forms the back bone of therapy in PCNSL with low dose whole brain radiation having important role in long term disease control[8]. Cytosine arabinoside has been added to high dose methotrexate to improve survival in this group of patients[9]. In another series 5-year event free survival was reported to be 70% in patients treated with combination chemotherapy of high dose methotrexate and Cytosine arabinoside without radiotherapy[10]. A radiation dose of 40-45 Gray to the whole cranium is recommended. Cranio spinal irradiation and intra thecal methotrexate is useful in patients with spinal drop metastasis or CSF dissemination. But this aggressive treatment approach is associated with significant toxicity. Neuro cognitive effects, hormonal imbalances, growth abnormalities and secondary malignancies are very important when we treat a pediatric case with such aggressive approach[2].
In conclusion, lymphoma in mid brain in pediatric age group is extremely rare. Chemotherapy forms the most important part of therapy for such cases. Low dose whole brain radiotherapy may be considered for improving long term disease control.
Focal midbrain glioma.
Tectal glioma, primitive neuro ectodermal tumor.
B cell lymphoma (DLBCL).
Focal midbrain glioma.
DLBCL.
Gross total excision, high dose methotrexate based 6 cycles of chemotherapy, cranio spinal irradiation.
This is a very rare location of a lymphoma in a teenager. The case presentation is interesting.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: India
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Alshehabi Z, Delwail V, Kupeli S, Mihaila RG S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Korfel A, Schlegel U. Diagnosis and treatment of primary CNS lymphoma. Nat Rev Neurol. 2013;9:317-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 136] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 2. | Abla O, Weitzman S, Blay JY, O’Neill BP, Abrey LE, Neuwelt E, Doolittle ND, Baehring J, Pradhan K, Martin SE. Primary CNS lymphoma in children and adolescents: a descriptive analysis from the International Primary CNS Lymphoma Collaborative Group (IPCG). Clin Cancer Res. 2011;17:346-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Rodriguez MM, Delgado PI, Petito CK. Epstein-Barr virus-associated primary central nervous system lymphoma in a child with the acquired immunodeficiency syndrome. A case report and review of the literature. Arch Pathol Lab Med. 1997;121:1287-1291. [PubMed] |
| 4. | Kai Y, Kuratsu J, Ushio Y. Primary malignant lymphoma of the brain in childhood. Neurol Med Chir (Tokyo). 1998;38:232-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Preusser M, Woehrer A, Koperek O, Rottenfusser A, Dieckmann K, Gatterbauer B, Roessler K, Slavc I, Jaeger U, Streubel B. Primary central nervous system lymphoma: a clinicopathological study of 75 cases. Pathology. 2010;42:547-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Sutherland T, Yap K, Liew E, Tartaglia C, Pang M, Trost N. Primary central nervous system lymphoma in immunocompetent patients: a retrospective review of MRI features. J Med Imaging Radiat Oncol. 2012;56:295-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Johnson BA, Fram EK, Johnson PC, Jacobowitz R. The variable MR appearance of primary lymphoma of the central nervous system: comparison with histopathologic features. AJNR Am J Neuroradiol. 1997;18:563-572. [PubMed] |
| 8. | Milgrom SA, Yahalom J. The role of radiation therapy in the management of primary central nervous system lymphoma. Leuk Lymphoma. 2015;56:1197-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | DeAngelis LM, Yahalom J, Heinemann MH, Cirrincione C, Thaler HT, Krol G. Primary CNS lymphoma: combined treatment with chemotherapy and radiotherapy. Neurology. 1990;40:80-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 179] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 10. | Abla O, Sandlund JT, Sung L, Brock P, Corbett R, Kirov I, Griffin TC, Blaser S, Weitzman S. A case series of pediatric primary central nervous system lymphoma: favorable outcome without cranial irradiation. Pediatr Blood Cancer. 2006;47:880-885. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |