Published online Nov 16, 2016. doi: 10.12998/wjcc.v4.i11.375
Peer-review started: April 22, 2016
First decision: July 5, 2016
Revised: August 1, 2016
Accepted: August 27, 2016
Article in press: August 29, 2016
Published online: November 16, 2016
Processing time: 206 Days and 20.1 Hours
Foreign body (FB) ingestion is very common in Malaysian population. The most commonly ingested FB is fish bone. Common presenting symptoms include FB sensation, odynophagia and or sharp pricking pain during swallowing. A careful history and physical examination is very important. Despite negative laryngoscopy and rigid esophagoscopy, persistent symptoms warrants further radiographic imaging studies. The FB can migrate extraluminally and involve other important adjacent structures of the neck and along the digestive tract. We report 3 cases of extraluminal migration of fish bone and their complications, which were successfully managed. One case with vascular complication which involve common carotid artery and the other two cases with neck abscess formation involving thyroid gland, retropharyngeal and parapharyngeal abscess.
Core tip: Accidental fish bone ingestion is very common but the complication of migrating fish bone into the neck spaces causing abscess and adjacent important structures of the neck alarm us the need for earlier detection and intervention. This case report represents 3 cases of foreign body ingestion which has a life threatening complications but successfully treated and factors that lead to these complications identified.
- Citation: Johari HH, Khaw BL, Yusof Z, Mohamad I. Migrating fish bone piercing the common carotid artery, thyroid gland and causing deep neck abscess. World J Clin Cases 2016; 4(11): 375-379
- URL: https://www.wjgnet.com/2307-8960/full/v4/i11/375.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i11.375
The commonest accidental foreign body (FB) ingestion encountered in our daily practice in Malaysia is fish bone as fish is a household favourite as a protein source. Common presenting symptoms are including FB sensation or sharp pain during swallowing. Some of the patients seek medical treatment immediately and recovered well without any unwanted sequelae. Unfortunately, few of them presented with complications of the FB ingestion because they preferred the traditional treatment causing the delay to get proper treatment. Delay detection of fish bone impaction or missing fish bone was usually due to negative findings of visual inspection and laryngoscopy, in addition with low sensitivity detection rate of radiolucent fish bone from the lateral neck radiograph[1]. Patient was rarely asymptomatic during the intervening period and after over a few days patient presented with symptoms and signs of complication such as neck abscess[2].
A 20-year-old man presented with odynophagia and pricking sensation at the right anterior neck four days after he ingested FB while eating. He had no fever, no neck swelling and no obstructive symptoms. On examination, the neck was not tender and showed no swelling palpable. The intraoral findings were normal. Laryngoscopy showed no evidence of FB in the oropharynx, hypopharynx as well as larynx. Soft tissue neck radiograph demonstrated a radiopaque FB shadow at C5 vertebral body level (Figure 1). Direct laryngoscopy and rigid esophagoscopy under general anaesthesia revealed an edematous posterior pharyngeal wall but no FB seen. Then, contrasted computed tomography (CT) of the neck showed presence of thin sharp-ended FB opacity embedded within the soft tissue of the right neck just below the vocal cord region (level C5/C6) (Figure 2).
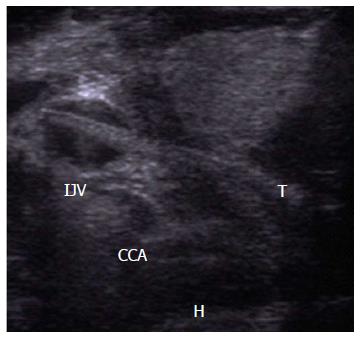
A neck ultrasonography study showed a linear FB seen coursing from the right thyroid lobe and runned obliquely piercing the right common carotid artery with the tip of FB abutting the internal jugular vein. Small hematoma was seen in between the right thyroid lobe and the right common carotid artery (Figure 3). Patient underwent right neck exploration and it was later found that the removed fish bone measuring 2.5 cm, with through-and-through piercing the right common carotid artery.
An 80-year-old lady with underlying diabetes mellitus and hypertension, presented with persistent pricking neck pain associated with odynophagia and dysphagia. The patient had accidentally ingested a fish bone six days prior to the presentation. She only tolerated small amount of soft diet but had no obstructive symptoms such as dyspnea or noisy breathing. Intraoral examination did not reveal any FB. There was a right level II neck swelling, firm and tender. Plain soft tissue neck radiograph demonstrated a radiopaque FB in a vertical position at C5-C6 level of vertebral body (Figure 4). Flexible fiberoptic nasopharyngolaryngoscopy showed pooling of saliva at both pyriform fossa, no medialization of lateral pharyngeal wall and no bulging at the posterior wall. Transnasal esophagoscopy also revealed normal finding. A direct laryngoscopy with rigid esophagoscopy and needle aspiration of right neck swelling were conducted under general anaesthesia and revealed edematous arytenoids and posterior pharyngeal wall, an abrasion area at 17 cm from upper incisors but no slough or pus at the abrasion site. No FB was seen in the esophagus. Upon milking the right neck swelling externally, we noticed minimal pus drained out from above the cricopharyngeal area, but were unsure of the origin. Then, needle aspiration of the right neck swelling was done, but no pus aspirated. We proceeded with contrasted CT and revealed a FB migration into the strap muscles and right thyroid lobe complicated with intramuscular and right submandibular abscess (Figure 5). No neck ultrasound was done prior to surgery.
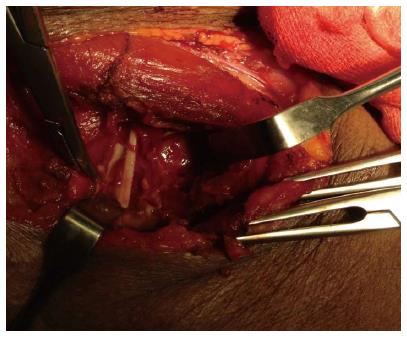
A surgical exploration under general anaesthesia the next day revealed a 4 cm fish bone with a pointed sharp end located at the edge of the right thyroid lobe, piercing through the medial aspect the right sternocleidomastoid muscle (Figure 6). Ten milliliter of pus was drained out from the neck region around the fish bone and the abscess cavity extend superiorly to the submandibular region. The pus cultured group C beta-hemolytic Streptococcus and patient completed intravenous (IV) tazocin (piperacillin + tazobactam) for 1 wk. The patient was observed 11 d post operation because the wound is sloughy with poor diabetic control and there was a need to complete the IV tazocin for one week.
A 70-year-old gentleman with poorly controlled diabetes mellitus accidentally ingested a fish bone. He experienced a FB sensation associated with pain in the throat. He had visited a district hospital after 5 d of ingestion in view of the persistent symptoms. A thorough clinical examination with soft tissue neck radiograph and a flexible fiber optic endoscopy was performed and revealed no significant findings. He was given one course of oral antibiotics.
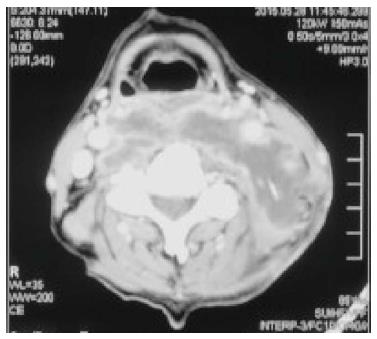
One week later, he presented again to the hospital with increasing left neck swelling, vomited pus, but had no fever. There was a diffused swelling at the left side of the neck, firm and tender. Intraorally, there was no FB noted, no medialization of lateral pharyngeal wall and no obvious opening with pus seen. Flexible fiber optic laryngoscopy of the upper aerodigestive tract was negative. A contrasted CT of the neck revealed a fish bone at the level C3, measures 2.5 cm in length with hypodense collection at the retropharyngeal area extend from C1-C5 level, and left parapharyngeal area extending laterally and posteriorly to the left carotid space (Figure 7).
Patient underwent transcervical neck exploration and direct laryngoscopy with intraoral pus drainage under general anesthesia. There was an abscess collection medial to posterior end of left sternocleidomastoid muscle with medial end of the muscle was unhealthy with slough. Fish bone measure 2.5 cm embedded in the slough tissue medial to the posterior end of the sternocleidomastoid muscle (Figure 8). Intraoperatively, pus was coming out from the ruptured retropharyngeal wall at the level of epiglottis, and drainage was done via direct laryngoscopy. Pus culture revealed group C beta-hemolytic Streptococcus. Intravenous cefuroxime and metronidazole were administered. A repeated flexible fiber optic laryngoscopy on day 11 post operatively showed no more pus coming out in the aerodigestive tract with a negative fistula test by drinking a water dyed with methylene blue without any leakage seen at the external neck wound. Patient was kept in ward for 11 d post operatively because of the poor diabetic control and the need for dressing of the neck wound.
Fish bone ingestion is the commonest FB ingestion in otorhinolaryngology practice especially in Asian population[3]. Most patients with foreign bodies ingestion were presented within 24 h[4]. Late presentation may be due to self treatment at home where patients tried to swallow bolus of food to dislodge the FB or they prefer to seek traditional treatment first. Late presentations and delay in treatment lead to unwanted and serious complications[4]. In our cases, patients came late between day 4 and 10 post-ingestion. Fish bone ingestion can be as simple as impaction at the base of tongue, palatine tonsil or vallecula which can be easily removed in clinic settings without any complications[3]. Other sites of impaction include the pyriform fossa, the epiglottis, the cricopharyngeus and the esophagus. The incidence of FB getting lodged at the cricopharynx or at any one of the other constrictions of the esophagus is 5%[5].
A detailed history taking, physical examination and simple radiography of the neck as well as endoscope findings are useful for diagnosis. Lue et al[6] had reported a sensitivity and specificity of plain radiography as 39% and 72% respectively to detect presence of fish bones.
Very rarely, an ingested FB can also penetrate through the gastrointestinal tract and can become lodged in the soft tissues of the neck. In the presence of positive neck radiography, negative direct laryngoscopy and rigid esophagoscopy findings, with persistent clinical symptoms, high index of suspicion of migrating FB should alarm the clinicians. Fish bone can migrate extraluminally and cause deep neck abscess (retropharyngeal, parapharyngeal abscess), vascular complications including vascular esophageal fistula (aorta-esophageal, innominate artery-esophageal fistula) and puncture of carotid artery, thromboembolism, brachial plexus injury, thyroid gland retention[7] and very rarely inflammatory pseudotumour of liver when the fishbone tracked down to the gastrointestinal tract[8].
Suspected complication or other negative investigative modalities, CT scan can be used as it is considered the best diagnostic tool for better detection of FB type, size, orientation, location and its relationship to other vital structures in the neck such as carotid artery, internal jugular vein, thyroid gland, thyroid cartilage and hyoid bone. It may also indicate the location and extension of the neck abscess. Therefore, CT scan is very important for diagnosis as it also acts as a guiding tool for surgeon when a surgical neck exploration is warranted. However, ultrasonography still has a role in evaluating the embedded or migrating FB. When dealing with FB retention in the thyroid gland, cervical ultrasonography is superior to CT scan in terms of differentiating the calcification from the FB and microcalcification from nodular goiters. Besides, ultrasonography was able to show the shape and orientation of the fish bone after several directional changes of the probe[7]. In our first case, neck ultrasonography presented a better and more detailed image than the neck CT scan.
The FB migration to extraluminal area is attributed by several factors. These include the orientation and pointed shape of the fish bone[4], contraction of the cricopharyngeus muscle during swallowing[9] or neck muscles during neck movement, and local inflammation of the esophageal or pharyngeal wall and direct pressure necrosis[10]. In a Singaporean series, there were 24 cases of migrating FBs, and they concluded that all of the migrated FBs were linear, sharp fish bones with horizontal orientation were more likely to migrate extraluminally to the path of least resistance[4].
The initial CT scan findings in case 1 demonstrated the FB embedded within the soft tissue of the right neck just below the vocal cord region, but after 24 h, intraoperatively, we found that the fish bone already migrated and piercing the right common carotid artery. Jamal et al[11] reported a patient with rapid movement of fish bone from the onset of patient’s complaint until the time of spontaneous extrusion in the neck was estimated about 72 h.
A fish bone piercing the inferior pole of right thyroid lobe in case 2 was removed successfully via the transcervical neck exploration, preserving the thyroid gland. Other literature had reported cases of thyroid abscess caused by ingested fish bone needed thyrotomy through the transcervical approach and a fish bone deeply buried in the left thyroid gland removed with thyroidectomy[12]. The background history of uncontrolled diabetes mellitus can worsen the abscess formation with retained FB as we can see in our third case.
In conclusion, extraluminal migrating foreign bodies should be suspected early when patient having persistent symptoms, despite negative laryngoscopy and rigid esophagoscopy. Plain radiography can be either negative or positive as the fish bone may be radiolucent or radiopaque. It should be confirmed with CT scan or may be aided with neck ultrasonography and removed surgically as soon as possible to prevent life-threatening consequences.
Patients with a few days history of fish bone ingestion presented with persistent odynophagia, dysphagia and neck swelling.
Migrating fish bone complicated with abscess formation.
Flexible nasopharyngoscopy was done for the 3 patients but unable to locate the fish bone.
Fish bone was seen in the soft tissue neck X-ray of 2 patients. Computed tomography (CT) scan and neck ultrasound were done and managed to locate the fish bone (one piercing the common carotid artery, one near the thyroid gland and one in the posterolateral part of the neck) and to look for the extension of the abscess.
All three patients had underwent neck exploration to remove the fish bone and they were given one course of intravenous antibiotic because of the inflammation and abscess formation.
When a patient is symptomatic for fish bone ingestion but direct laryngoscopy and esophagoscopy revealed normal finding, a CT scan should be done to look for embedded foreign body.
Fish bone migration is a very rare case. This paper introduced three cases of fish bone migration. The material is true, and the picture is real. There are some clinical significances in clinical field.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Malaysia
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Abulezz TA, Xu Z S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Jha SK, Kumar SP, Somu L, Ravikumar A. Missing fish bone: case report and literature review. Am J Otolaryngol. 2012;33:623-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 2. | Thomas AM, Nadeem B, Badaridatta HC. Migrated foreign body neck. J Case Rep Med. 2012;1:1-3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Yang SW, Chen TM, Chen TA. Migrating fish bone complicating a deep neck abscess. Chang Gung Med J. 2005;28:872-875. [PubMed] |
| 4. | Chee LW, Sethi DS. Diagnostic and therapeutic approach to migrating foreign bodies. Ann Otol Rhinol Laryngol. 1999;108:177-180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Shanmugam R, Shanmugam VU, Mariappan R, Swaminathan B, Nandipati S, Ghosh P, Ramya CV. Migrating foreign body in the neck penetrating the neck muscle. Sch J Med Case Rep. 2015;3:393-395. |
| 6. | Lue AJ, Fang WD, Manolidis S. Use of plain radiography and computed tomography to identify fish bone foreign bodies. Otolaryngol Head Neck Surg. 2000;123:435-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 68] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 7. | Lin YH, Ho HC, Hsiao SH. An ingested fishbone migrating to the thyroid gland - a case report. Tzu Chi Med J. 2006;18:438-441. |
| 8. | Srinivasan UP, Duraisamy AB, Ilango S, Rathinasamy A, Chandramohan SM. Inflammatory pseudotumor of liver secondary to migrated fishbone - a rare cause with an unusual presentation. Ann Gastroenterol. 2013;26:84-86. [PubMed] |
| 9. | Coret A, Heyman Z, Bendet E, Amitai M, Itzchak I, Kronberg J. Thyroid abscess resulting from transesophageal migration of a fish bone: ultrasound appearance. J Clin Ultrasound. 1993;21:152-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Goh YH, Tan NG. Penetrating oesophageal foreign bodies in the thyroid gland. J Laryngol Otol. 1999;113:769-771. [PubMed] |
| 11. | Jamal S, Irfan M, Nazim N. Spontaneous extrusion of migrated fishbone in the neck after 48 hours of ingestion. Bangladesh J Med Sci. 2011;10:129-132. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Park JH, Kim BH, Jung SC, Do NY. Deep neck infection caused by fish bone migration and huge fish bone migration observed by chance: Two unusual cases of fish bone migration. Am J Case Rep. 2011;12:186-188. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |