Published online Nov 16, 2016. doi: 10.12998/wjcc.v4.i11.364
Peer-review started: March 14, 2016
First decision: March 25, 2016
Revised: July 20, 2016
Accepted: August 30, 2016
Article in press: August 31, 2016
Published online: November 16, 2016
Processing time: 247 Days and 12.5 Hours
An idiopathic renal arteriovenous (AV) fistula is a rare malformation of the kidney that may present insidiously with heart failure or hematuria. The treatment may be challenging due to large fistula size that may limit endovascular management. The authors report a case of an 85-year-old Caucasian woman who presented with acute heart failure and was found to have a right renal AV fistula. Since she had no prior history of renal intervention or trauma, a diagnosis of idiopathic renal AV fistula was made. She was managed by endoluminal occlusion using multiple stainless steel coils and Amplatzer vascular plug II device. The follow-up computed tomography showed complete occlusion of the fistula. This report highlights the late presentation of this rare disease and presents the utility of the combination of coils and Amplatzer device for management of a large fistula. It also reiterates that even if large, these fistulas can be managed by endovascular occlusion.
Core tip: Idiopathic renal arteriovenous fistula is rare but may present in middle-aged to elderly population with heart failure or hematuria. It is more common in right kidney and typically there is a single communication with the renal vein. Since these can have a very high-flow, the management can be challenging, but is typically done by nephrectomy or endovascular occlusion. With advances in endovascular techniques, it has become the preferred management option. If conventional embolizing materials do not obtain appropriate closure, Amplatzer vascular plug II may be used to reinforce the occlusion of the feeding artery.
- Citation: Nagpal P, Bathla G, Saboo SS, Khandelwal A, Goyal A, Rybicki FJ, Steigner ML. Giant idiopathic renal arteriovenous fistula managed by coils and amplatzer device: Case report and literature review. World J Clin Cases 2016; 4(11): 364-368
- URL: https://www.wjgnet.com/2307-8960/full/v4/i11/364.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i11.364
The arteriovenous (AV) fistula is defined as a direct connection between an artery and a vein bypassing the usual capillary network; although in the case of coronary circulation, there may be communication between the coronary artery and a cardiac chamber[1]. With an increase in percutaneous interventions, the incidence of acquired renal AV fistulas is increasing, but the idiopathic/congenital type of AV fistula continues to be rare. The idiopathic AV fistula is usually large and has high flow; features that may limit the endovascular management due to the possibility of incomplete occlusion and migration of embolizing material[2]. Some reports in the literature have favored nephrectomy due to the large size of shunt and multiplicity of the shunt vessels[3,4]. We report a case of an elderly female presenting with heart failure due to idiopathic renal AV fistula that was successfully treated by embolization of renal artery aneurysm by multiple coils and occlusion of the distal limb of renal artery by Amplatzer vascular plug (AVP) II device. She showed significant improvement in symptoms along with improvement in imaging signs of heart failure at 6-mo follow-up.
An 85-year-old woman presented to the emergency room with progressive dyspnea for 4 wk with abdominal distension and lower extremity swelling for 2 wk. Past medical history was significant for hypertension and atrial fibrillation, which were being managed with low dose metoprolol succinate. Physical examination revealed moderate respiratory distress and irregularly irregular rhythm with the heart rate ranging 70 to 90 beats/min. Rales were noted over the both lower lung fields, with raised jugular venous pressure, tender hepatomegaly, abdominal distension and bilateral lower extremity edema. The cardiac exam was notable for harsh grade III/IV holosystolic murmur that was loudest at the apex. A bruit was heard in the posterior abdomen loudest at the right costovertebral angle. However no palpable thrill was felt. The electrocardiogram showed atrial fibrillation with the ventricular rate of 80 however without ST/T wave changes. Laboratory analysis revealed elevated b-type Natriuretic Peptide (BNP) of 4497 pg/mL (reference range < 100 pg/mL).
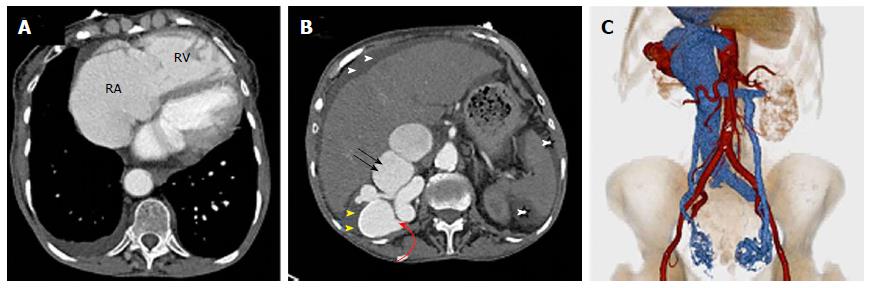
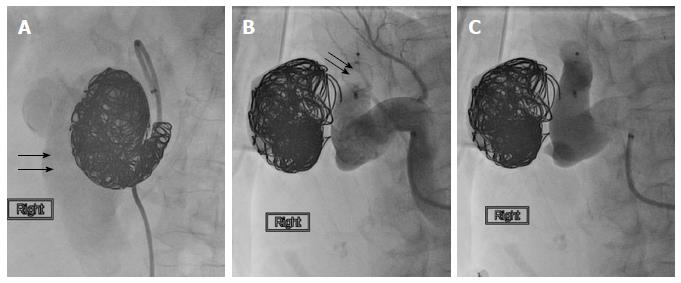
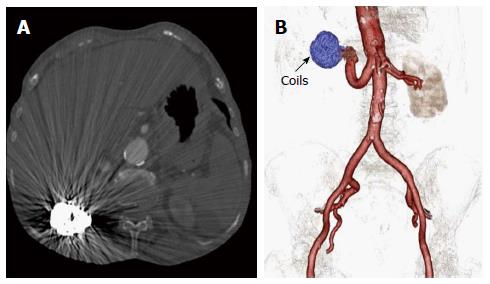
Transthoracic echocardiogram, performed as part of workup for heart failure, showed moderate concentric left ventricular hypertrophy with preserved left ventricular ejection fraction of 55%-60%. However, the patient was noted to have right heart failure with dilated right atrium and ventricle. The presence of bruit in the posterior abdomen prompted an ultrasound (USG) that revealed a peripherally calcified large anechoic structure within in the right kidney with the color flow on color Doppler imaging concerning for a large renal artery aneurysm and/or a vascular malformation. Computed tomography (CT) angiogram done for further evaluation showed aneurysmally dilated renal artery and vein (Figure 1B and C). The distal renal artery had a peripherally calcified focal aneurysm (Figure 1B) with early enhancement of renal vein suggesting an AV fistula. Besides severe dilatation of IVC, hepatic veins, and gonadal veins were seen due to compensatory volume overload while right side cardiac chambers were enlarged (Video 1 and Figure 1A). The patient was deemed to be a poor surgical candidate, and the decision was made to manage by endovascular occlusion. The interpolar branch of renal artery was catheterized that showed a large aneurysm with immediate opacification of the renal vein. It was decided to completely obliterate the aneurysm using large stainless steel coils. After using 22 stainless steel coils, the angiogram image showed a faint visualization of the IVC (Figure 2A). It was then decided to reinforce the obliteration of fistula by occluding the feeding distal renal artery by 12 mm Amplatzer vascular plug II (AGA Medical Corporation, Plymouth, MN). Following the deployment of the AVP II, there was no opacification of the venous system (Figure 2B and C). Her symptoms were improved and and the clinical exam showed resolution of jugular venous distention, decreased abdominal distension and lower extremity edema. The ascites resolved on follow-up CT (Figure 3) and the BNP decreased to 296 pg/mL at 6 mo.
Renal AV fistula can be acquired (approximately 70% of cases), congenital (approximately 25% of cases) or idiopathic (approximately 3%-5% of cases) in nature[5]. Acquired renal arteriovenous fistula (AVF) may be secondary to renal interventions (biopsy, surgery or nephrostomy placement), renal injury, inflammation or tumor[6]. Idiopathic fistulas occur in the absence of predisposing factors, are usually seen in middle aged patients and often present with cardiovascular symptoms like hypertension or congestive heart failure. They are hypothesized to be caused by erosion of an intraparenchymal renal arterial branch aneurysm into a vein[3,5]. Our case also shows a large renal artery aneurysm supporting this hypothesis. Idiopathic renal AV fistula is more common in the right kidney and females are affected twice as compared to males, similar to present case[6]. Given the absence of predisposing factor, congenital and idiopathic fistulas have been classified together as spontaneous AV fistula[7,8]. The congenital AV fistulas however usually present with hematuria and often shows multiple tortuous varix-like vessels on angiogram. The spontaneous fistulas on the other hand often present with cardiovascular symptoms and show a single enlarged feeding vessel just like in our case[6].
Like AVFs of any other anatomical site, imaging plays a vital role in diagnosis and treatment of the renal AVF[9]. Ultrasound with color Doppler is usually the initial investigation. On grey-scale ultrasound, the renal artery aneurysm may be anechoic and mimic a renal cyst. The Color and spectral Doppler are therefore vital to not only reveal the vascular nature of the lesion, but also to demonstrate arterialized venous return. Multidetector CT may reveal an enlarged feeding artery, early venous filling and venous engorgement secondary to hyperdynamic flow. Additionally, it may even show the site of fistulous communication, useful to optimize management.
The idiopathic renal AV fistula is often large and if symptomatic can be treated by either endoluminal occlusion or surgical excision. To the best of our knowledge, there is only one case of idiopathic renal AV fistula undergoing spontaneous closure[10]. Endoluminal occlusion is usually the management of choice in renal AV fistulae since it occludes the shunt while preserving the renal function[11]. Large shunt size and possibility of migration of embolizing material may limit endovascular management, warranting surgical management[3,4,12]. Traditionally stainless steel coils, gel foam and covered wall stents have been used as endovascular agents for the management of these cases[13]. In 2007, Idowu et al[13] described the use of Amplatzer device for management of high flow renal AV fistula. They described the dual use of this device, initially as an upstream filter to prevent migration of the coils (that were used for fistula embolization) and then it was used as the final embolizing device for the renal artery. In 2009, Campbell et al[14] described successful embolization of idiopathic renal AV fistula using Amplatzer device without using the coils. In 2013, Perkov et al[15] described the first case in which 2nd generation Amplatzer vascular plug (AVP II) was used for high flow renal AV fistula after initially attempted coil embolization failed due to migration. In our case, due to gigantic size and high flow, it was decided to first use multiple coils, but when the angiogram showed persistent IVC opacification, the occlusion was reinforced using AVP II. Our case highlights that despite the large size, combination of coils and AVP II device is an effective endovascular management option. Only a few cases with the similar management of idiopathic renal AV fistula have been described[13-15]. This case is also unique regarding the presentation of idiopathic AV fistula at this advanced age although previously one case is described in an 81-year-old woman[16]; but it is unclear in that case whether the etiology was acquired or idiopathic.
An 85-year-old woman presented with right heart failure and was found to have a giant idiopathic renal arteriovenous (AV) fistula on imaging. Decision was made to treat her by endoluminal occlusion. Initially multiple coils were used but complete occlusion could not be obtain. Hence, Amplatzer vascular plug was used to reinforce the obliteration of draining artery and adequate occlusion was achieved.
Idiopathic renal arteriovenous fistula with right heart failure.
Renal aneurysm, ischemic cardiomyopathy, high output heart failure, massive pulmonary embolism.
Elevated β-type Natriuretic Peptide of 4497 pg/mL (reference range < 100 pg/mL) that decreased to 296 pg/mL at 6 mo after treatment.
Echocardiogram showed LV hypertrophy with normal ejection fraction and right heart failure. Ultrasound showed a calcified anechoic renal lesion with color filling and dilated renal vein suggesting an aneurysm with possible malformation. Computed tomography confirmed the presence of a large calcified intraparenchymal renal aneurysm that was in communication with dilated renal vein suggesting renal fistula.
Endovascular occlusion using coils and 2nd generation Amplatzer vascular plug.
Idiopathic renal AV fistula can be large in size with high flow. If complete obliteration of fistula cannot be obtained using coils, then an Amplatzer vascular plug can be used to occlude the draining artery.
This report described an interesting and rare case of an idiopathic renal AV fistula in that update therapeutic strategy is well described. The paper is well written and the results are potentially useful when considering the diagnosis and treatment of a patient with renal AV fistula.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Corbacioglu SK, Durandy YD S- Editor: Kong JX L- Editor: A E- Editor: Wu HL
| 1. | Nagpal P, Khandelwal A, Saboo SS, Garg G, Steigner ML. Symptomatic Coronary Cameral Fistula. Heart Views. 2015;16:65-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Giavroglou CE, Farmakis TM, Kiskinis D. Idiopathic renal arteriovenous fistula treated by transcatheter embolization. Acta Radiol. 2005;46:368-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Nawa S, Ikeda E, Naito M, Kondo K, Yuasa I, Watanabe K, Fujita Y, Kunitomo T, Otsuka K. Idiopathic renal arteriovenous fistula demonstrating a huge aneurysm with a high risk of rupture: report of a case. Surg Today. 1998;28:1300-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Nagahara A, Nishimura K, Okuyama A. A giant idiopathic renal arteriovenous fistula associated with high-output heart failure. Int J Urol. 2009;16:648-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Mansueto G, D’Onofrio M, Minniti S, Ferrara RM, Procacci C. Therapeutic embolization of idiopathic renal arteriovenous fistula using the “stop-flow” technique. J Endovasc Ther. 2001;8:210-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Dönmez FY, Coşkun M, Uyuşur A, Hunca C, Tutar NU, Başaran C, Cakir B. Noninvasive imaging findings of idiopathic renal arteriovenous fistula. Diagn Interv Radiol. 2008;14:103-105. [PubMed] |
| 7. | Fogazzi GB, Moriggi M, Fontanella U. Spontaneous renal arteriovenous fistula as a cause of haematuria. Nephrol Dial Transplant. 1997;12:350-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Alscher DM, Hupp T, Mettang T, Kuhlmann U. A patient with hypertension was cured after resection of a renal AV fistula. Nephrol Dial Transplant. 2000;15:249-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Saboo SS, Juan YH, Belkin M, Sacks A, Khandelwal A, Steigner ML, Rybicki FJ. Multi-detector CT angiography in case of concomitant pseudoaneurysm and arteriovenous fistula of the lateral superior geniculate artery. Postgrad Med J. 2014;90:118-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Iko BO, Jones GW. Idiopathic renal arteriovenous fistula. Spontaneous closure. Urology. 1987;29:86-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Paschalis-Purtak K, Januszewicz M, Rokicki A, Puciłowska B, Imiela J, Cybulska I, Cieśla W, Prejbisz A, Szostek M, Januszewicz A. Arteriovenous fistula of the kidney: a case report of 47-year-old female patient treated by embolisation. J Hum Hypertens. 2003;17:293-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Val-Bernal JF, Caballero CI, Lastra P, Azueta A, Gutierrez-Baños JL. Aneurysm of the right renal vein arising from an idiopathic arteriovenous fistula. Cardiovasc Pathol. 2014;23:310-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Idowu O, Barodawala F, Nemeth A, Trerotola SO. Dual use of an amplatzer device in the transcatheter embolization of a large high-flow renal arteriovenous fistula. J Vasc Interv Radiol. 2007;18:671-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 34] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Campbell JE, Davis C, Defade BP, Tierney JP, Stone PA. Use of an amplatzer vascular plug for transcatheter embolization of a renal arteriovenous fistula. Vascular. 2009;17:40-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Perkov D, Novačić K, Novosel L, Knežević N. Percutaneous embolization of idiopathic renal arteriovenous fistula using Amplatzer vascular plug II. Int Urol Nephrol. 2013;45:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Khawaja AT, McLean GK, Srinivasan V. Successful intervention for high-output cardiac failure caused by massive renal arteriovenous fistula-a case report. Angiology. 2004;55:205-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |