Published online Oct 16, 2016. doi: 10.12998/wjcc.v4.i10.344
Peer-review started: February 9, 2016
First decision: May 19, 2016
Revised: June 29, 2016
Accepted: July 29, 2016
Article in press: August 1, 2016
Published online: October 16, 2016
Processing time: 247 Days and 19.9 Hours
The indications of point-of-care ultrasound (POCUS) in the management of multiple trauma patients have been expanding. Although computed tomography (CT) scan of the orbit remains the gold standard for imaging orbital trauma, ultrasound is a quick, safe, and portable tool that can be performed bedside. Here we report two patients who had severe eye injuries with major visual impairment where surgeon-performed POCUS was very useful. One had a foreign body injury while the other had blunt trauma. POCUS was done using a linear probe under sterile conditions with minimum pressure on the eyes. Ultrasound showed a foreign body at the back of the left eye globe touching the eye globe in the first patient, and was normal in the second patient. Workup using CT scan, fundsocopy, optical coherence tomography, and magnetic resonance imaging of the orbits confirmed these findings. The first patient had vitreous and sub retinal haemorrhage and a full thickness macular hole of the left eye, while the second had traumatic optic neuropathy. POCUS gave accurate information concerning severe eye injuries. Trauma surgeons and emergency physicians should be trained in performing ocular ultrasound for eye injuries.
Core tip: The indications of point-of-care ultrasound in the management of multiple trauma patients have been expanding. Here we report two patients who had severe eye injuries with visual impairment in whom surgeon-performed point-of-care ultrasound was accurate. Trauma surgeons and emergency physicians should be trained in performing ocular ultrasound for eye injuries.
- Citation: Abu-Zidan FM, Balac K, Bhatia CA. Surgeon-performed point-of-care ultrasound in severe eye trauma: Report of two cases. World J Clin Cases 2016; 4(10): 344-350
- URL: https://www.wjgnet.com/2307-8960/full/v4/i10/344.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i10.344
The indications for point-of-care ultrasound (POCUS) in the management of patients with multiple trauma including the abdomen, chest and extremities have been evolving[1]. Eye injury constitutes about 3% of all Emergency Department visits[2]. Around 15% of major trauma patients have eye and orbital injuries[3]. Direct clinical examination of the eye in the emergency setting may be jeopardized by severe tissue injury around the eye[4]. Although computed tomography (CT) scan of the orbit remains the gold standard for imaging orbital trauma, ultrasound is a quick, safe, and portable tool that can be performed bedside and detect intra-ocular injuries[5,6]. Here we report two patients who had major eye injuries in whom surgeon-performed POCUS was very useful.
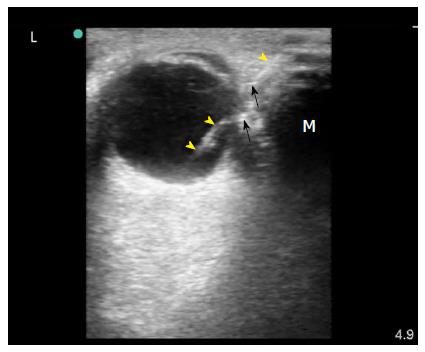
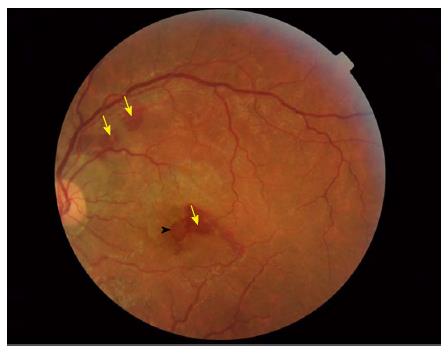
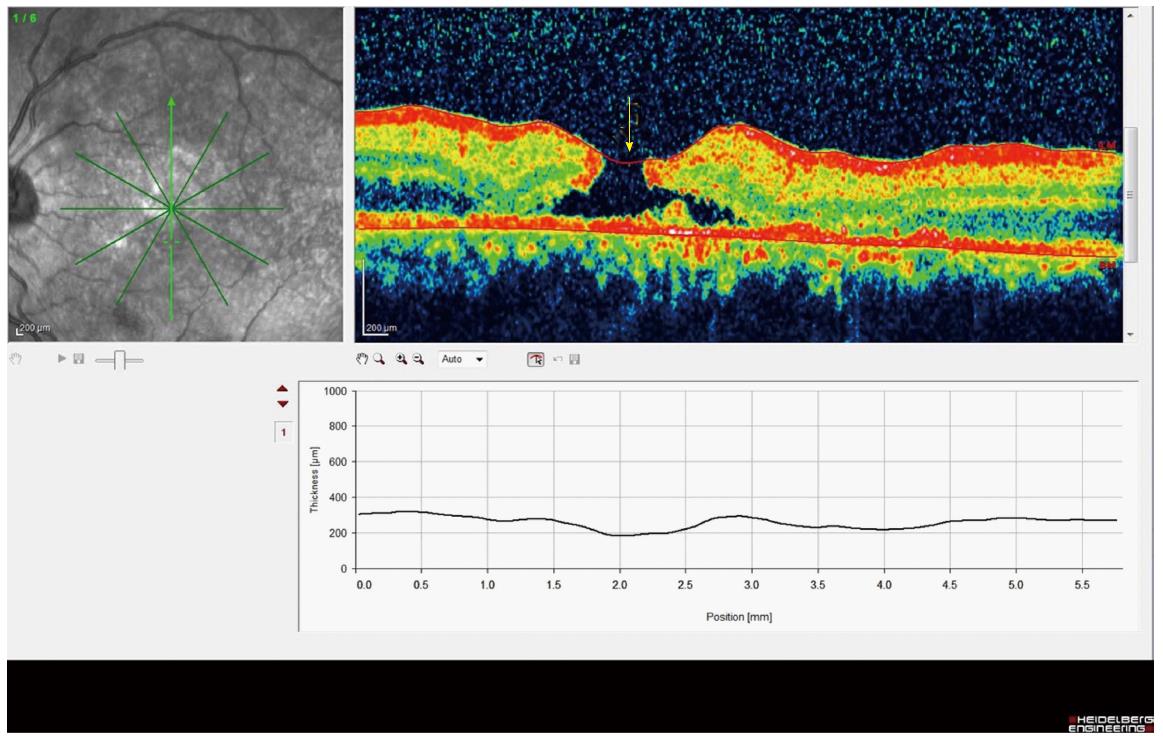
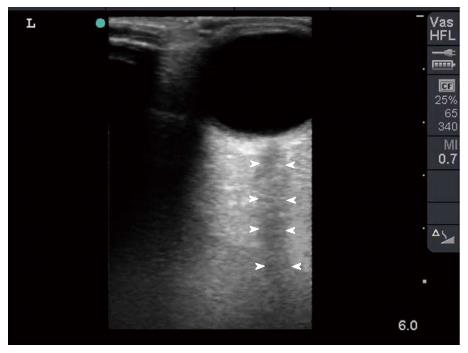
A 26-year-old labourer sustained a foreign body injury to the left eye. On examination, there was a 1 cm wide metallic foreign body embedded into his left orbit (Figure 1). Visual acuity of the right eye was 6/9 and of the left eye 6/120. The left eye was moving freely in all directions and the pupils were reactive to light. Surgeon-performed POCUS of the left eye was done using a linear probe under sterile conditions with minimum pressure on the eye. Ultrasound showed a foreign body in the retro-bulbar space which was most probably touching the eye globe (Figure 2). Plain CT scan of the orbits confirmed these findings (Figure 3). The foreign body was removed under GA. Follow up eye examination using slit lamp exam, fundoscopy (Figure 4) and optical coherence tomography (Figure 5) showed vitreous and sub-retinal haemorrhage and a full thickness macular hole in the left eye. The patient was referred to a vitreo-retinal surgeon for further management.
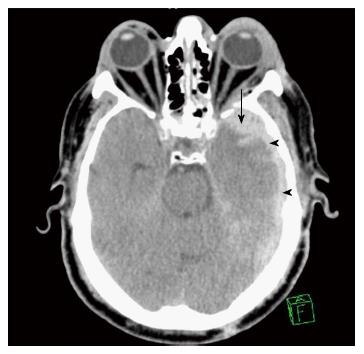
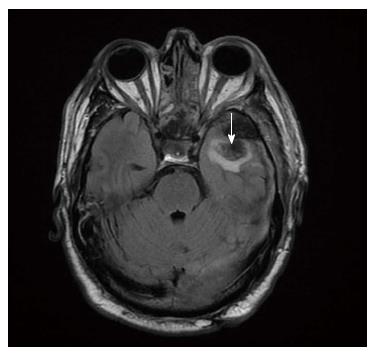
A 50-year-old diabetic man was riding a quad-bike without a helmet. One of the wheels of the quad-bike hit a pothole, and as a result the patient was thrown off and his head hit the ground. The patient lost consciousness for a short period. When brought to the Emergency Department, he was irritable with a Glasgow Coma Scale of 14/15. His blood pressure was 165/110 mmHg and his pulse was 110 bpm. On examination the patient had bilateral racoon eyes. Trauma CT scan showed a thin left subdural haematoma and parenchymal haemorrhagic contusion (Figure 6). The patient had multiple fractured ribs and a small pneumothorax to one side which was treated by chest tube drainage. He had grade III splenic injury which was treated conservatively. The patient was kept under observation in the Intensive Care Unit for one day. A follow up brain CT showed no significant brain oedema or mass effect, and he was shifted to the ward. Forty-eight hours after injury the patient was more alert. He complained of loss of vision of his left eye.
Examination of the left eye showed a raccoon eye, an oedematous eyelid, and severe ecchymosis of the conjunctiva. The left pupil was dilated and non-reactive to light (Figure 7). Visual acuity of the right eye was 20/20. There was no light perception by the left eye. Both eyes moved freely in all directions. Ophthalmoscopy of the fundi of both eyes was normal. A clinical diagnosis of left optic nerve injury was made. Optic nerve transection or retro-bulbar haematoma were suspected. The CT scan of both optic nerves was inconclusive because the trauma CT scan cuts were thick hence the optic nerves could not be properly evaluated. Bedside surgeon-performed POCUS of both eyes was normal. There was no intraocular bleeding or retro-bulbar haematoma, and the optic nerve was intact (Figure 8). We initially thought that this was possibly a false negative POCUS. We requested magnetic resonance imaging (MRI) of both orbits which confirmed the POCUS findings (Figure 9). A diagnosis of left traumatic optic neuropathy was reached. The patient was discharged home on day 16. He was contacted by phone 18 mo after injury to enquire about his left eye. He can now see only flashes in his left eye without vision. He has been thoroughly investigated in two private eye clinics and both reached the diagnosis of left traumatic optic neuropathy.
Clinical evaluation of severe eye injuries can be difficult due to the injury of surrounding soft tissues, presence of distracting injuries, or low level of consciousness[4]. The use of POCUS has dramatically increased over the last two decades, and this includes ocular ultrasound[7]. Bedside ocular ultrasound may give information that cannot be gained by clinical examination: for example, massive eyelid oedema may restrict the examination of pupil reaction in severe head injury. Pupil reaction can be examined by ultrasound even if the eye is closed[8]. Ultrasound may show lens dislocations, hyphaema, retinal detachment, or foreign bodies[4,6,9]. Furthermore, ultrasound may provide a reliable diagnosis of orbital fractures when studying the zygomatico-orbital complex[10].
The B (Brightness) ultrasound mode, which we have used, is commonly used by ophthalmologists. It depends on the strength by which tissue particles are attached (tissue impedance)[11]. The particles in fluid are less firmly attached to each other compared with those in muscles, and those in muscles are less firmly attached compared with those in fibrous tissue. Accordingly fluid reflects fewer ultrasound waves (that are later picked up by the ultrasound probe) compared with muscles, and muscles reflect fewer ultrasound waves compared with fibrous tissue. Therefore fluid will be black in ultrasound images (anechoic), muscles grey, and fibrous tissue white (hyperechoic). The resolution of the images (quality) will depend on the frequency of the ultrasound waves. The higher the frequency, the better the resolution[11]. Images using a 10 MHz ophthalmic probe[12] will be similar images to those discussed in the present studies. Ultrasound biomicroscopy, which uses B mode and high frequency ultrasound waves (35-50 MHz), gives excellent images of the eye[12]. At present POCUS examination of the eye is not commonly performed by non-ophthalmologists.
It is very difficult to master POCUS without understanding the basic physics of ultrasound. For example Figure 2 shows a mirror artefact which was produced because the ultrasound waves were reflected by the intra-orbital foreign body through a specific angle. This artefact mimicked an object on the opposite side to the foreign body, exactly as would be seen in a real mirror[11,13]. If the operator had not been aware of or familiar with the possibility of the production of artefacts in this way, they could possibly have interpreted such an artefact as a haematoma.
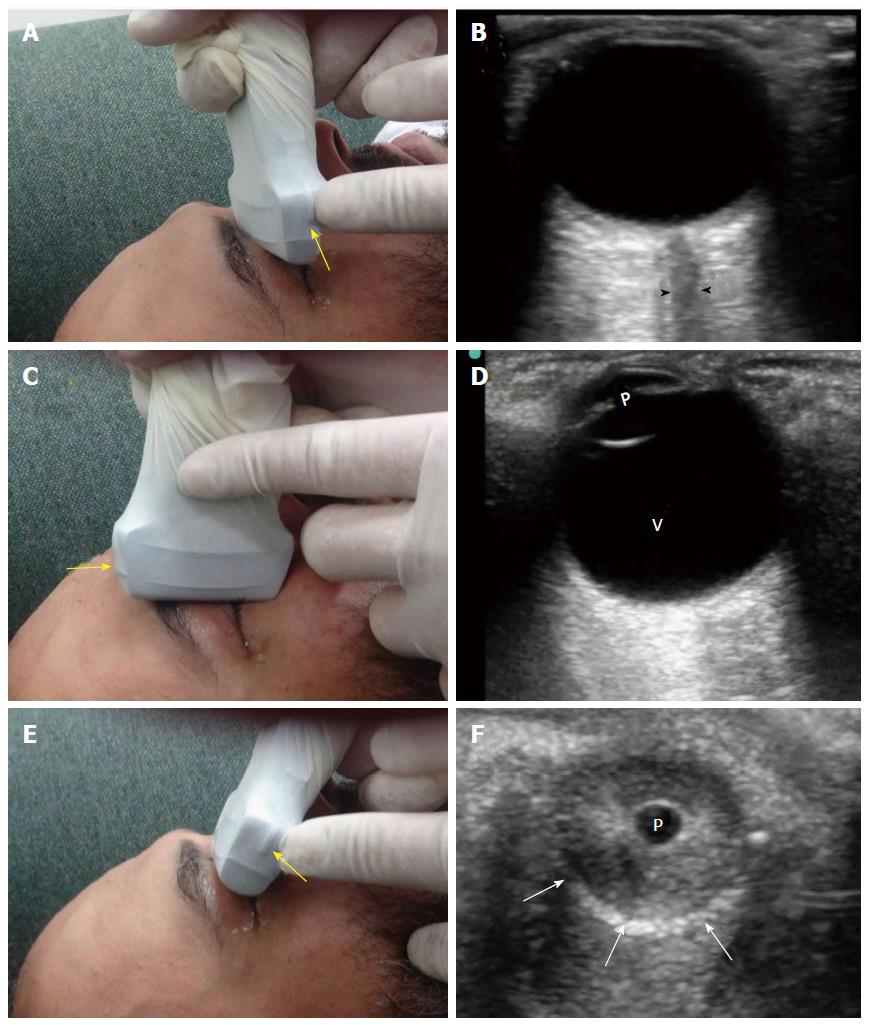
A portable ultrasound machine (MicorMaxx, SonoSite Inc., Borthel, WA, United States) with a high-frequency linear array probe is used (10-12 MHz). This enables the POCUS study to be performed bedside in the Emergency Department (as we did with the first patient) or in the ward (as we did with the second patient) without the need to transfer the patient. We usually perform the study while the patient is in supine position.
POCUS should be performed under sterile conditions in eye injuries because the ultrasound probe may transmit infection. We use a modified inexpensive sterile technique in which we tie the fingers of a sterile surgical glove (size 7.5-8.5). Sterile gel is put inside the glove which is used to cover the probe. The operator wears sterile surgical gloves and applies sterile gel over the closed eyelid. The probe has to be controlled by both hands so as to apply gentle pressure on the eye. Gentle pressure which does not change the convexity of the cornea is adequate[8]. The marker of the probe should point to the right side of the patient or upwards. Gentle examination using a high-frequency probe without pressure usually yields images which are clear enough to be evaluated[9]. This was clearly demonstrated in both of our patients. Both positive and negative findings proved to be accurate.
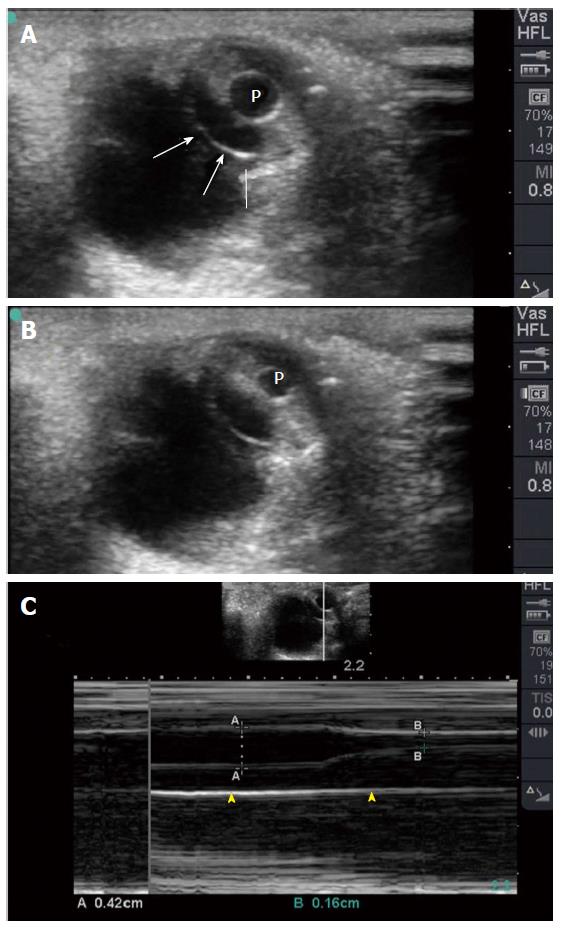
There are three common views which are used to examine the eye: The transverse antero-posterior view; the sagittal antero-posterior view; and the coronal view. These views are shown in Figure 10. The operator can fan or tilt the probe as needed. The coronal view, which is clinically useful, can be achieved through a transverse view directed cranially through the lower eyelid while the patient gazes upwards. This view can demonstrate pupil reaction to light; this is more obvious when the contralateral eye is closed[8]. M Mode can be used to accurately measure pupil size. This is important in patients who have severe head injury and whose eyelids cannot be opened (Figure 11).
CT scan is considered the gold standard for studying major eye injuries and diagnosing foreign bodies because it is available in many emergency departments[2,4]. It is also sensitive in diagnosing orbital fractures[14].
CT of the orbit is performed as part of whole–body trauma CT protocol in patients with multiple trauma, as occurred in the second patient[15]. Our trauma CT scan protocol yields slices 5 mm thick, with the possibility of producing images at slices 1 mm thick at different planes after finishing the study. Specific orbital CT scan is obtained through thin sections (0.625-1.25 mm) that can be later reconstructed in different planes[4,14]. Nevertheless, CT has risk of radiation, is not sensitive to optic nerve contusion as shown in our second case, and occasionally foreign bodies may cause streak artefacts[4].
MRI is very useful in studying the soft tissues and organic or wooden foreign bodies[2,4,6]. Nevertheless, it is contraindicated in cases of suspected metallic foreign bodies because of the risk of vision loss[2]. Furthermore, it is not available in all hospitals, particularly in emergency settings[2,14].
POCUS is available at the bedside, is safe, can be repeated without risk of radiation, produces real time images, and for studying intraocular soft tissue damage including vitreous and retina it is a superior tool to CT scan[2,4,6,16]. Ultrasound is of great value when ophthalmoscopy cannot be performed because of changes to light-conducting media resulting from bleeding or laceration[6]. Furthermore, ultrasound is very useful in pre-hospital or disaster situations where CT scan and MRI are not available[17]. The two cases that we have presented highlight the value of surgeon-performed POCUS in diagnosing eye injuries both in positive and negative studies.
If globe rupture is clinically evident, then ultrasound is contraindicated because it may worsen the clinical picture if high pressure is applied to the eye during the examination[2,4,14] Nevertheless, if globe rupture is only suspected, then the eye can be examined but with an extremely cautious gentle technique[6]. The closed eye should be examined using aseptic technique with gel applied over the eyelid. Furthermore, small foreign bodies may be missed by ultrasound if not imaged in the proper plane.
Four prospective observational studies have shown that POCUS has a high sensitivity and specificity in the evaluation of orbital trauma if performed by trained non radiologists[16]. Nevertheless, it is operator dependable. Proper training and experience are essential for accurate interpretation of images. The POCUS studies of our patients were performed by an operator (FAZ) who has more than 25 years’ experience of using POCUS. Both cases were managed in collaboration and consultation with ophthalmologists who were available at the same time of performing the POCUS exam.
It is important to stress that CT scan, ultrasound, and MRI are complementary and not competitive when studying eye injuries. For example, CT scan can be used to localize the location of a foreign body, while ultrasound can be used to diagnose the intra-ocular injuries[6].
In summary ocular POCUS gave very useful information in two cases of severe eye injuries. Trauma surgeons and emergency physicians should be properly trained on performing ocular ultrasound for eye injuries. Trauma surgeons and emergency physicians should take advantage of POCUS as an extension of their clinical examination techniques to enable them to take appropriate timely decisions.
We thank Ms. Geraldine Kershaw, Lecturer, Medical Communication and Study Skills, Department of Medical Education, College of Medicine and Health Sciences, UAE University for her assistance in grammar and linguistic corrections.
Two patients who had severe eye injuries, one caused by a foreign body and the other by blunt trauma.
Traumatic ophthalmic visual impairment.
Vitreous haemorrhage, retinal detachment, optic nerve injury, globe rupture.
Ultrasound showed a foreign body at the back of the left eye globe touching the eye globe in the first patient, and was normal in the second patient. Computed tomography (CT) scan, fundsocopy, optical coherence tomography, and magnetic resonance imaging of the orbits confirmed these findings.
Vitreous and sub retinal haemorrhage and a full thickness macular hole in the first case; and traumatic optic neuropathy in the second case.
Referral for retinal surgery in the first case, expectant treatment in the second case.
Point-of-care-ultrasound (POCUS) had a high sensitivity and specificity in the evaluation of orbital trauma if performed by trained non radiologists. It is especially useful when CT scan and magnetic resonance imaging (MRI) are not available.
POCUS is a good tool for studying intraocular soft tissue damage. It is of great value when ophthalmoscopy is difficult because of the pacification of light-conducting media. CT scan is considered the gold standard for studying major eye injuries and diagnosing foreign bodies, while MRI is very useful in studying the soft tissues of the eye and organic or wooden foreign bodies.
Trauma surgeons and emergency physicians should be properly trained in performing ocular ultrasound for eye injuries because they can take advantage of POCUS as an extension of their clinical examination techniques to enable them to take appropriate timely decisions.
The presented manuscript is interesting and shares experience with the POCUS of the eye in the emergency setting.
Manuscript source: Invited manuscript
Specialty Type: Medicine, research and experimental
Country of Origin: United Arab Emirates
Peer-Review Report Classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C,C,C,C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Hong YJ, Inan UU, Koleva-Georgieva DN, Nowak MS S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Mohammad A, Hefny AF, Abu-Zidan FM. Focused Assessment Sonography for Trauma (FAST) training: a systematic review. World J Surg. 2014;38:1009-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Dunkin JM, Crum AV, Swanger RS, Bokhari SA. Globe trauma. Semin Ultrasound CT MR. 2011;32:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Poon A, McCluskey PJ, Hill DA. Eye injuries in patients with major trauma. J Trauma. 1999;46:494-499. [PubMed] |
| 4. | Sung EK, Nadgir RN, Fujita A, Siegel C, Ghafouri RH, Traband A, Sakai O. Injuries of the globe: what can the radiologist offer? Radiographics. 2014;34:764-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Abu-Zidan FM. Point-of-care ultrasound in critically ill patients: Where do we stand? J Emerg Trauma Shock. 2012;5:70-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Fielding JA. The assessment of ocular injury by ultrasound. Clin Radiol. 2004;59:301-312. [PubMed] |
| 7. | Kilker BA, Holst JM, Hoffmann B. Bedside ocular ultrasound in the emergency department. Eur J Emerg Med. 2014;21:246-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 8. | Chiao L, Sharipov S, Sargsyan AE, Melton S, Hamilton DR, McFarlin K, Dulchavsky SA. Ocular examination for trauma; clinical ultrasound aboard the International Space Station. J Trauma. 2005;58:885-889. [PubMed] |
| 9. | Berkoff DJ, English J, Theodoro D. Sports medicine ultrasound (US) beyond the musculoskeletal system: use in the abdomen, solid organs, lung, heart and eye. Br J Sports Med. 2015;49:161-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Evirgen Ş, Kamburoğlu K. Review on the applications of ultrasonography in dentomaxillofacial region. World J Radiol. 2016;8:50-58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 37] [Cited by in RCA: 33] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Abu-Zidan FM, Hefny AF, Corr P. Clinical ultrasound physics. J Emerg Trauma Shock. 2011;4:501-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 12. | Silverman RH. High-resolution ultrasound imaging of the eye - a review. Clin Exp Ophthalmol. 2009;37:54-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 115] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 13. | Feldman MK, Katyal S, Blackwood MS. US artifacts. Radiographics. 2009;29:1179-1189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 146] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 14. | Kubal WS. Imaging of orbital trauma. Radiographics. 2008;28:1729-1739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 101] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Gunn ML, Kool DR, Lehnert BE. Improving Outcomes in the Patient with Polytrauma: A Review of the Role of Whole-Body Computed Tomography. Radiol Clin North Am. 2015;53:639-56, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Nunn KP, Thompson PK. Towards evidence based emergency medicine: PRIVATE Best BETs from the Manchester Royal Infirmary. BET 1: Can the nature and extent of orbital trauma be optimally assessed with ultrasound imaging in the emergency department? Emerg Med J. 2011;28:809-810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Dittrich K, Abu-Zidan FM. Role of Ultrasound in Mass-Casualty Situations. International Journal of Disaster Medicine. 2004;2:18-23. [RCA] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |