Published online Jan 16, 2016. doi: 10.12998/wjcc.v4.i1.25
Peer-review started: May 6, 2015
First decision: September 8, 2015
Revised: October 14, 2015
Accepted: November 10, 2015
Article in press: November 11, 2015
Published online: January 16, 2016
Processing time: 261 Days and 5.7 Hours
Peristomal variceal bleeding due to portal hypertension is an entity that has rarely been reported with 3%-4% risk of death. A 68-year-old woman who had undergone a palliative colostomy (colorectal carcinoma) presented with a massive hemorrhage from the colostomy conduit. Considering her oncological status with medial and right hepatic veins thrombosis due to liver metastasis invasion, an emergency transhepatic coil embolization was successfully performed. Standard treatment modality for these cases has not been established. Percutaneous transhepatic coil embolization of varices is a safe and effective choice in patients who present with life threatening bleeding and exhibit contraindications to transjugular intrahepatic portosystemic shunt.
Core tip: Peristomal variceal bleeding in patients with portal hypertension is a rare entity with increased risk of death. In situations when life-saving procedures are required in such patients, standard treatment modality has not been established. We illustrate a successfully performed emergency transhepatic coil embolization of bleeding varices in an oncological patient with contraindications to transjugular intrahepatic portosystemic shunt. Additionally, we discuss other different treatment options described in the literature and its technical challenges.
- Citation: Maciel MJS, Pereira OI, Motta Leal Filho JM, Ziemiecki Junior E, Cosme SL, Souza MA, Carnevale FC. Peristomal variceal bleeding treated by coil embolization using a percutaneous transhepatic approach. World J Clin Cases 2016; 4(1): 25-29
- URL: https://www.wjgnet.com/2307-8960/full/v4/i1/25.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v4.i1.25
Patients with portal hypertension commonly develop varices that typically arise in the gastro-esophageal region. On the other hand, ectopic varices - a rare condition - may occur along the entire gastrointestinal tract. Sites other than the gastroesophageal junction account for only 5% of all variceal bleeding[1]. Peristomal variceal initial bleeding mortality rate is as high as 40% due to the challenges related to the diagnosis, management and treatment of this condition. Variceal bleeding from a stoma is a well-known entity that has rarely been reported[2]. A bleeding episode has an estimated risk of death of 3% to 4%[3].
The standard of practice for the handling of stomal variceal hemorrhage has not yet been established. Treatment options range from conservative therapies (medication and/or sclerotherapy), to surgical procedures - such as stomal reconstruction or portosystemic shunting[3]. Minimally invasive therapies such as transjugular intrahepatic portosystemic shunt (TIPS) creation have been immensely useful for portal pressure decompression and have been demonstrated to be an effective treatment for individual with stomal bleeding. Albeit, some patients are not suitable candidates for TIPS procedure because they have subjacent hepatic encephalopathy or poor liver function[4].
Transhepatic coil embolization of bleeding stomal varices could be an option for treatment in cases in which TIPS is contraindicated; however, it demands a transhepatic approach with the related risk of hepatic damage or bleeding[5,6]. Another minimally invasive treatment option is embolization of the offending varix via transjugular transhepatic approaches[2].
The purpose of this paper is to describe a rare case of variceal hemorrhage from a colostomy that was successfully treated with coil embolization using a percutaneous transhepatic approach. This study was approved by the Clinical Hospital of the University of Sao Paolo Medical School institutional review board.
A 68-year-old woman who had undergone palliative loop colostomy due to locally advanced colorectal carcinoma two years prior presented to our service with chronic bleeding from the colostomy conduit. The primary disease was stage T4 Nx M1 with ovary, uterus and ureter invasion, as well as liver and lung metastases; the patient has been treated with four cycles of palliative chemotherapy with leucovorin, 5-fluorouracil (5FU) and oxaliplatin. The patient also had right portal vein compression, medial and right hepatic vein thrombosis caused by the liver metastasis invasion, and no previous history of liver dysfunction (child-pugh A5).
At the end of the fourth cycle of chemotherapy, she developed recurrent episodes of stomal bleeding that required transfusion and hospitalization. The bleeding was first thought to originate from the colon and was treated with tranexemic acid (500 mg, three times daily for 7 d), fresh frozen plasma and red blood cell transfusion. The clinical exam demonstrated stomal mucosal erithema and edema. Because the hemorrhaging persisted, an enhanced multislice computed tomography (CT) scan was performed, along with 3D reconstructions; it showed ectopic varices at the colostomy site that were fed by the inferior mesenteric vein (Figure 1), which was suggestive of portal hypertension.
Massive hemorrhage occurred during the hospitalization, and the patient developed hemorrhagic shock. Considering her oncological status (T4 M1 clinical stage IV) in palliative chemotherapy and hepatic metastasis, an emergency transhepatic embolization was planned as a less invasive procedure than TIPS.
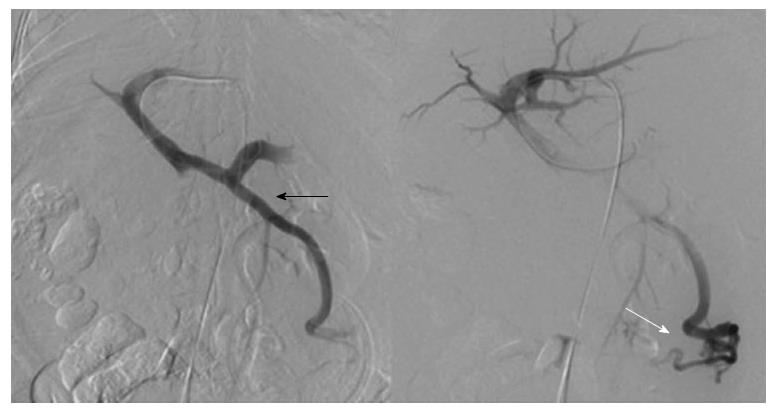
Percutaneous transhepatic access was obtained through a left portal vein branch ultrasound guided puncture with a 22-gauge Chiba needle and catheterization using the NPAS kit (Cook, Bloominton, IN, United States). Portal and mesenteric venography were performed using a Cobra II 5 French catheter that showed varices appearing from the hepatofugal flow onto the colostomy conduit by inferior mesenteric tributaries (Figure 2). The portal-pressure gradient (between the portal vein and the right atrium measured by central venous catheter placement) was 16 mmHg. Ectopic varices were accessed by catheterization using a Cobra II 5 French catheter and a 0.035’ hydrophilic guidewire (Merit Medical, Jordan, UT, United States), and coil embolization was then performed. A total of 11 platinum coils, 14 to 20 cm long (Nester, Cook, Bloominton, IN, United States and Interlock, Boston Scientific, Natick, MA, United States), were used. After embolization, venography demonstrated complete obliteration of the variceal branches (Figure 3). The portal-pressure gradient measured after embolization was 24 mmHg. Gelfoam was used to occlude the hepatic parenchyma catheter path after sheath removal.
The patient developed no complications from the procedure, no hemorrhages developed during the first month post embolization. Improvement of stomal mucosal erythema and edema were observed and no colostomy disfunction was noted. Over the most recent six-month follow-up period, the patient was maintained on palliative treatment with chemotherapy and radiotherapy despite minor stomal and rectal bleeding that was managed conservatively with compression and tranexemic acid.
Hemorrhaging of ectopic varices is a rarely reported subject in the literature and is mostly related to digestive tract or umbilical bleeding. Hemorrhage arising from peristomal varices has been related in case reports, and most occur from an ileostomy conduit[2,4-7]. This sort of bleeding is commonly chronic and recurrent rather than massive. Doppler ultrasound, CT and magnetic resonance angiography may identify varices in the region of the stoma and facilitate the diagnosis of cirrhosis, portal hypertension and the assessment of portal patency[8]. This patient had a precise diagnosis of peristomal variceal bleeding with portal hypertension based on enhanced multislice CT and venography.
The combination of extensive liver metastasis and chemotherapy was assumed to be the etiology of this patient’s portal hypertension. Several authors have reported portal hypertension due to perisinusoidal fibrosis, severe sinusoidal obstruction, and fibrotic venular occlusion in patients receiving oxaliplatin. The use of oxaliplatin and 5FU has been related to obliterative portal venopathy as a consequence of nodular regenerative hyperplasia that causes portal congestion and sinusoidal dilation[9].
Recent reviews have not yet defined the standard of care in these cases of ectopic variceal bleeding. Recommended care includes conservative medical therapy, endoscopic therapy, interventional radiology therapy, surgical shunt placement and even liver transplantation. Band ligation and sclerotherapy are feasible options in the management of these cases, but the high risk of necrosis, perforation, massive hemorrhage, and sustained portal hypertension result in disappointing outcomes[8]. When the bleeding is life threatening or unresponsive to conservative treatments, surgical shunts have been performed. Surgical decompression of the portal vein is effective for controlling and preventing variceal bleeding, but may cause liver failure or hepatic encephalopathy, with mortality ranging from 1% to 50%[5,7].
Direct percutaneous ultrasound-guided endoluminal embolization with cyanoacrylate glue or coils has been described as a potential alternative treatment[10,11]. Although this approach has been described as a safe and effective technique for controlling stomal bleeding, it is particularly useful when a single dominant feeding varix is identified[12]. Other limitations are that additional varices or venous collateral may still develop as well as the increased risk of embolization material migration to the main portal vein and mucosal damage at the stomal site.
TIPS alone or in combination with varix embolization is effective for stop bleeding of ectopic variceal in patients suffering with portal hypertension because it treats the underlying pathological process by reducing portal hypertension[8,13]. Even though TIPS appears to be a safe and effective treatment modality, 25% and 30% of patients develop rebleeding with a patent TIPS and are at risk of developing encephalopathy, respectively[3,10].
Transhepatic variceal coil embolization is a feasible and safe option reported in the literature[10,12]. Our patient was in poor clinical condition in the emergency setting of an acute life threatening peristomal variceal bleed; therefore, an approach based on coil embolization of the varices using a percutaneous transhepatic approach was selected, with TIPS being reserved for recurrent bleeding. After the bleeding was successfully treated, it seemed appropriate for this patient to be treated with TIPS, whereas there was an increase in the portal-pressure gradient after coil embolization. Nevertheless, the present common understanding of TIPS creation for hemostasis is that it raises the incidence of hepatic encephalopathy and spoils liver function[7]. It was decided that the TIPS procedure was contraindicated in this case after a multidisciplinary discussion, considering that this was an oncological patient who was receiving palliative treatment for worsening clinical status due to disease progression with vertebral metastasis and medullar compression. Other conditions that would make the procedure technically challenging was the hepatic tumor burden with medial and right hepatic vein thrombosis.
The transhepatic approach was the best option for this case considering the patient had no ascites and there were no contraindications to this access despite the liver metastases. This route allowed access to numerous vessels in the same setting. The procedure was successfully performed with occlusion of the peristomal varices, and no complications such as mesenteric or stomal ischemia occurred. Kishimoto et al[6] reported a similar case of stomal varices treated with percutaneous transhepatic coil embolization with the use of a total of 28 coils including fibered platinum microcoils, platinum coils and stainless steel coils to stop the bleeding. In our case, a total of 11 fibered platinum coils with lengths varying from 14 to 20 cm were used. The long lengths of the coils contributed to the use of a smaller number of coils in the present case.
Recurrent bleeding may occur in patients who have undergone transhepatic embolization as a result of variceal recanalization or the development of new ones because it did not decrease the portal pressure. Sclerotherapy with absolute ethanol followed by coil occlusion has been reported to prevent recurrent bleeding, but the procedure was not shown to prevent it[5]. Toumeh et al[5] described a patient who developed recurrent bleeding from recanalized ileostomy varices one year after the first coil embolization treatment, which was controlled by transhepatic embolization. The embolic agents used were alcohol, Gelfoam and Gianturco coils[5]. Although the method of coil embolization has a high incidence of recurrent hemorrhage, it is effective for the treatment of life threatening acute variceal bleeding. Our patient stabilized with a major reduction in bleeding and no need of blood transfusion, and the oncologic palliative treatment was continued.
Complications of transhepatic embolization are related to liver trauma with bleeding, bile leakage and portal vein thrombosis[5-7]. Transhepatic tract bleeding after percutaneous portal vein access has been reported to be up to 30% of cases when access site closure was not performed. When surgeons routinely embolize or close transhepatic tracts in percutaneous portal puncture, this bleeding risk decreases to 0%-6.5%[14]. Gelfoam or small coil use to occlude the parenchymal track is effective at preventing bleeding from the puncture site. Although rare, liver trauma can be avoided by ultrasound guided transhepatic puncture. The progress of the embolization should be closely monitored to prevent reflux of the embolic agent into the portal vein. Similar to transhepatic portal puncture, the reported rate of fatal complications due to TIPS procedure access is between 0.6% and 4.3%, including intraperitoneal hemorrhage as a result of extrahepatic rupture of the portal vein, laceration of the hepatic artery, and transcapsular puncture with the transjugular needle[15].
In conclusion, percutaneous transhepatic embolization could be considered for patients with stomal variceal bleeding, in whom TIPS is contraindicated.
A 68-year-old woman who had undergone palliative loop colostomy due to locally advanced colorectal carcinoma presented to our service with recurrent episodes of stomal bleeding that required transfusion and hospitalization.
At the end of the fourth cycle of chemotherapy, she developed recurrent episodes of stomal bleeding that required transfusion and hospitalization.
Coagulation disturb; colorectal neoplasm; gastro-esophageal varices.
Laboratory exams are compatible with massive hemorrhage (hemorrhagic shock).
Computed tomography showed ectopic varices at the colostomy site that were fed by the inferior mesenteric vein.
Coil embolization using a percutaneous transhepatic approach was performed to stop the variceal bleeding.
Patients with portal hypertension commonly develop varices that typically arise in the gastro-esophageal region. Ectopic varices are rare and may occur along the entire gastrointestinal tract. Sites other than the gastroesophageal junction account for only 5% of all variceal bleeding. Variceal bleeding from a stoma is a well-known entity that has rarely been reported. The risk of death from an episode of bleeding is estimated to be 3% to 4%.
Ectopic varices are rare (5% of all variceal bleeding) and may occur along the entire gastrointestinal tract. The risk of death from an episode of bleeding is estimated to be 3% to 4%, so the bleeding should be treated. Percutaneous transhepatic embolization should be considered for patients with stomal variceal bleeding, in whom transjugular intrahepatic portosystemic shunt is contraindicated.
This article describes about a successful case of percutaneous transhepatic coil embolization for peristomal variceal bleeding. This case report is meaningful and informative.
P- Reviewer: Shibasaki S
S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Norton ID, Andrews JC, Kamath PS. Management of ectopic varices. Hepatology. 1998;28:1154-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 239] [Cited by in RCA: 254] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 2. | Lashley DB, Saxon RR, Fuchs EF, Chin DH, Lowe BA. Bleeding ileal conduit stomal varices: diagnosis and management using transjugular transhepatic angiography and embolization. Urology. 1997;50:612-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Naidu SG, Castle EP, Kriegshauser JS, Huettl EA. Direct percutaneous embolization of bleeding stomal varices. Cardiovasc Intervent Radiol. 2010;33:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Ryu RK, Nemcek AA, Chrisman HB, Saker MB, Blei A, Omary RA, Vogelzang RL. Treatment of stomal variceal hemorrhage with TIPS: case report and review of the literature. Cardiovasc Intervent Radiol. 2000;23:301-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 28] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Toumeh KK, Girardot JD, Choo IW, Andrews JC, Cho KJ. Percutaneous transhepatic embolization as treatment for bleeding ileostomy varices. Cardiovasc Intervent Radiol. 1995;18:179-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Kishimoto K, Hara A, Arita T, Tsukamoto K, Matsui N, Kaneyuki T, Matsunaga N. Stomal varices: treatment by percutaneous transhepatic coil embolization. Cardiovasc Intervent Radiol. 1999;22:523-525. [PubMed] |
| 7. | Yao DH, Luo XF, Zhou B, Li X. Ileal conduit stomal variceal bleeding managed by endovascular embolization. World J Gastroenterol. 2013;19:8156-8159. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Spier BJ, Fayyad AA, Lucey MR, Johnson EA, Wojtowycz M, Rikkers L, Harms BA, Reichelderfer M. Bleeding stomal varices: case series and systematic review of the literature. Clin Gastroenterol Hepatol. 2008;6:346-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Rubbia-Brandt L, Audard V, Sartoretti P, Roth AD, Brezault C, Le Charpentier M, Dousset B, Morel P, Soubrane O, Chaussade S. Severe hepatic sinusoidal obstruction associated with oxaliplatin-based chemotherapy in patients with metastatic colorectal cancer. Ann Oncol. 2004;15:460-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 752] [Cited by in RCA: 763] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 10. | Arulraj R, Mangat KS, Tripathi D. Embolization of bleeding stomal varices by direct percutaneous approach. Cardiovasc Intervent Radiol. 2011;34 Suppl 2:S210-S213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Thouveny F, Aubé C, Konaté A, Lebigot J, Bouvier A, Oberti F. Direct percutaneous approach for endoluminal glue embolization of stomal varices. J Vasc Interv Radiol. 2008;19:774-777. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Kwok AC, Wang F, Maher R, Harrington T, Gananadha S, Hugh TJ, Samra JS. The role of minimally invasive percutaneous embolisation technique in the management of bleeding stomal varices. J Gastrointest Surg. 2013;17:1327-1330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Deipolyi AR, Kalva SP, Oklu R, Walker TG, Wicky S, Ganguli S. Reduction in portal venous pressure by transjugular intrahepatic portosystemic shunt for treatment of hemorrhagic stomal varices. AJR Am J Roentgenol. 2014;203:668-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 14. | Saad WE, Madoff DC. Percutaneous portal vein access and transhepatic tract hemostasis. Semin Intervent Radiol. 2012;29:71-80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 15. | Krajina A, Hulek P, Fejfar T, Valek V. Quality improvement guidelines for Transjugular Intrahepatic Portosystemic Shunt (TIPS). Cardiovasc Intervent Radiol. 2012;35:1295-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |