Published online Sep 16, 2015. doi: 10.12998/wjcc.v3.i9.848
Peer-review started: December 6, 2014
First decision: February 13, 2015
Revised: June 17, 2015
Accepted: July 3, 2015
Article in press: July 6, 2015
Published online: September 16, 2015
Processing time: 283 Days and 3.8 Hours
Tuberculosis (TB) is still a major health problem worldwide. We present a rare case of an immuno-competent patient with perianal TB. A 38-year-old man visited a clinic with pain, swelling, and redness in the perineum. He had been persistently coughing for the past 6 mo. The abscess had formed a fistula to the perianal region, indicating perianal abscess. Mycobacterium tuberculosis was found in sputum and perianal abscess. Surgical drainage was performed, and oral anti-tuberculous drugs were administered for 6 mo. The patient’s clinical course was favorable. On review of the literature on 58 cases of perianal TB, we found that the duration of persistent perianal lesion was much longer in patients without active pulmonary TB (APTB) than in those with APTB (66.4 mo vs 8.3 mo; confidence interval, 0.0760-0.9620, P = 0.0380). Thus, in cases of non-healing or recurrent perianal lesions, TB should be considered.
Core tip: We present a case of an immuno-competent patient with perianal tuberculosis (TB) and active pulmonary TB (APTB). In our literature review of 58 cases of perianal TB, we found that the duration of persistent perianal lesions was much longer in patients without APTB than in those with APTB (66.4 mo vs 8.3 mo; confidence interval, 0.0760-0.9620; P = 0.0380). In cases of non-healing or recurrent perianal lesions, the diagnosis of TB should be considered and culture for Mycobacterium tuberculosis and histologic examination should be conducted.
- Citation: Tago S, Hirai Y, Ainoda Y, Fujita T, Takamori M, Kikuchi K. Perianal tuberculosis: A case report and review of the literature. World J Clin Cases 2015; 3(9): 848-852
- URL: https://www.wjgnet.com/2307-8960/full/v3/i9/848.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i9.848
Tuberculosis (TB) is still a major health problem worldwide and is more prevalent in Asia. In Japan, in which TB prevalence is decreasing, estimated new TB cases per 100000 population per year is 10-19, which is in the same range with some European countries[1]. Extra-pulmonary TB occupied 3%-46% of all types of TB[2]. Perianal TB is an extremely rare type of extra-pulmonary TB (0.7%)[3]; however, its prevalence might be underestimated, as it can be misidentified as Crohn’s disease or other granulomatous diseases[4]. Here, we report a rare case of perianal abscess caused by Mycobacterium tuberculosis (MTB).
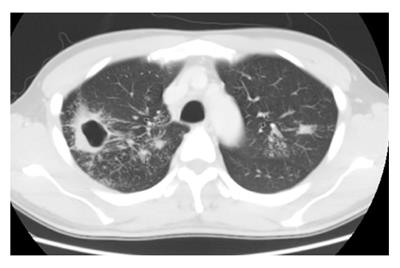
A 38-year-old Japanese man visited a clinic with chief complaints of pain in the perineum, which had developed 4 d earlier. He also had been persistently coughing for the past 6 mo. Chest radiography revealed a cavity in the right upper lung field, and acid-fast bacilli (AFB) were detected in his sputum. These findings indicated pulmonary TB, and the patient was subsequently admitted to the hospital. His past history was unremarkable: He smoked 20 pieces/d. He installed Japanese pinball machines (pachinko) for a living. He had visited North Korea 20 years ago and South Korea 3 years ago. He had no family history of TB. His blood pressure was 126/76 mmHg, pulse rate was 100 beats/min, temperature was normal at 37.3 °C, and with clear respiratory sounds. Redness, swelling, and tenderness were noted in the right perineum (Figure 1). Thoracic computed tomography confirmed the cavity in the right upper lung field and infiltration in the right upper and left middle lung fields (Figure 2). MTB DNA was amplified using polymerase chain reaction (PCR) (Kobasu TapMan® MTB, Switzerland), and sputum culture revealed MTB. A large amount of creamy white pus was drained from the incisional perianal abscess. The abscess had formed a fistula to the perianal region, indicating a perianal abscess. AFB were also detected in the wound pus and PCR and culture analysis confirmed MTB. Further, Escherichia coli was concomitantly isolated from the abscess. Oral administration of isoniazid, rifampicin, ethambutol, and pyrazinamide was initiated, and the clinical course was favorable. After completing the 6-mo oral administration of anti-TB drugs, the patient was operated upon for the anal fistula. His human immunodeficiency virus (HIV) test was negative. No apparent underlying disease was detected at the 3-mo follow-up examination.
We reviewed 58 cases of perianal TB (abscess, fistula, and ulceration) reported from 1970 to 2014 worldwide (Japan, 17 cases; Taiwan, 17 cases; South Korea, 4 cases; Hong Kong, 3 cases; United States, 3 cases; United Kingdom, 2 cases; Brazil, 2 cases; Spain, 2 cases; Turkey, 2 cases; Morocco, 1 case; Iran, 1 case; India, 1 case; France, 1 case; Bulgaria, 1 case), whereas 70.7% were from Asia[5-31]. The mean age (± SD) of the patients was 45.3 (± 10.6) years, and the male-to-female ratio [52 (89.7%) men and 6 (10.3%) women] was higher than that reported previously (4:1)[4,32]. Eighteen point six percent of the patients had underlying diseases related to immunodeficiency (respiratory diseases 3, diabetes mellitus 2, hepatitis 1, hepatitis + HIV 1, chronic kidney disease 1, malignancy 1, autoimmune disease 1, cardiovascular disease 1).
We researched duration of disease, that is the time from beginning of symptoms until diagnosed with perianal TB. Among 29 patients with complete data available on the duration of perianal lesion, the mean duration of disease was 34.6 mo. Of these, 15.3% of the patients had a surgical history of perianal lesions before the diagnosis of TB.
APTB was noted in 34 (57.6%) cases; history of TB, in 12 (20.3%) cases; and no history of pulmonary TB in 12 (20.3%) cases. The existence or non-existence of pulmonary TB was not reported in 1 (1.7%) case. We compared the characteristics of patients with APTB (n = 34) with those of patients without APTB (n = 24) (Table 1). The duration of disease in patients without APTB (66.4 mo) was significantly longer than that in patients with APTB (8.3 mo), as noted in a two-sample t-test (CI: 0.0760-0.9620; P < 0.05).
| Active pulmonary TB | Without APTB | |
| (n = 34) | (n = 24) | |
| Age (mean yr) | 41.2 | 51.1 |
| Sex (male) | 30 (88.2) | 22 (91.7) |
| Underling diseases | 6 (17.6) | 5 (20.8) |
| Previous anal surgery | 4 (11.8) | 5 (20.8) |
| TB complications | 2 (5.9) | 2 (8.3) |
| Intestinal TB | 0 | 2 (8.3) |
| Anal carcinoma | 2 (5.9) | 1 (4.2) |
| Duration of anal lesion (mo) | 6.8 | 66.5 |
Gastrointestinal TB accounts for less than 1% of all TB cases, and perianal disease is exceedingly rare, comprising 1% of digestive tract incidence[5].
In our literature review, only 18.6% of the patients had underlying diseases related to immunodeficiency. Therefore, not only immuno-compromised but also immuno-competent patients should be carefully evaluated, because TB can also occur in immuno-competent individuals, as noted in our case.
The mean duration of perianal TB was 34.6 mo, and 15.3% of the patients had a surgical history of perianal lesions before the diagnosis of TB. Perianal TB may have gone un-diagnosed for a long period.
APTB was noted in 34 (57.6%) cases; Since in cases of perianal TB, APTB is often concomitant with, it is important to conduct chest radiography and a detailed interview, especially to record chronic cough, fever, night sweats, or weight loss, which suggest APTB, in order to diagnose perianal TB.
We compared the characteristics of patients with APTB (n = 34) with those of patients without APTB (n = 24). We found that the occurrence of intestinal TB and TB complications (miliary TB, peritoneal TB, and iliopsoas muscle abscess by TB) were similar in both patient groups. This raises a question regarding the infectious routes in patients without APTB, since TB rarely, if ever, occurs as a primary infection in a perianal region. Two possible explanations are as follows: first, hematogeneous spread after reactivation of latent lung TB could be responsible[7], and second, other foci may have not been sufficiently investigated, as seen in our cases wherein only 37 (62.7%) cases included data on intestinal examination.
The duration of disease in patients without APTB (66.4 mo) was significantly longer than that in patients with APTB (8.3 mo), as noted in a two-sample t-test (CI: 0.0760-0.9620; P < 0.05). Since perianal TB does not have any specific clinical characteristics[5,10], its occurrence without APTB may be underestimated. In cases of chronic or recurrent fistula, the diagnosis of TB should be considered, and culture for MTB and histologic examination should be performed.
The patient in our case installed Japanese pinball machines (pachinko) for a living. In Tokyo patients developed TB without any apparent contact with TB patients most frequently spent their time and maybe acquired the infection at pachinko parlors (24%) and amusement parks (24%), followed by saunas (16%)[33]. In the United States, residents and employees of congregate settings such as hospitals, correctional facilities, nursing homes, and homeless shelters are at a high risk for TB exposure[34-36]. Thus, an interview to collect information on the places that the patient stayed at or visited and employment situation often could be helpful in making a diagnosis of TB.
In conclusion, we report the case of an immuno-competent man with perianal TB and APTB. In cases of non-healing or recurrent perianal fistula, TB should be considered as a causative agent.
A 38-year-old male patient presented with pain in the perineum, which had developed 4 d earlier and persistently coughing for the past 6 mo.
The patient had redness, swelling, and tenderness in the right perineum.
Testicular torsion, epididymitis, abscess, Fournier’s gangrene, torsion of the appendix testis, trauma, testicular cancer, inguinal hernia, Henoch-Schönlein purpura (IgA vasculitis), mumps and Crohn’s disease.
Acid-fast bacilli were detected in the sputum and wound pus and PCR and culture analysis confirmed Mycobacterium tuberculosis.
Computed tomography scan showed a cavity in the right upper lung field.
Histological examination of the abscess showed epithelioid granulomas and Langhans’ type multinucleated giant cells.
Surgical drainage was performed, and oral anti-tuberculous drugs were administered for 6 mo.
The authors reviewed 58 cases of perianal tuberculosis (TB) reported from 1970 to 2014 worldwide. And they found that the duration of persistent perianal lesion was much longer in patients without active pulmonary TB (APTB) than in those with APTB (66.4 mo vs 8.3 mo; CI: 0.0760-0.9620; P = 0.0380).
This case report presents an immuno-competent patient with perianal TB and APTB. On literature on cases of perianal TB, the authors found that the duration of persistent perianal lesions was much longer in patients without APTB than in those with APTB. In cases of non-healing or recurrent perianal lesions, the diagnosis of TB should be considered.
The description of a case with perianal tuberculosis is per se of interest since this form of tuberculosis is very rare and diagnosis is delayed. The manuscript contains a complete and comprehensible description of clinical and microbiological finding.
P- Reviewer: Hofmann-Thiel S, Viney K, van der Werf TS S- Editor: Yu J L- Editor: A E- Editor: Liu SQ
| 1. | Global tuberculosis report 2014, Figure 2.5. 2013;18 Available from: http://www.who.int/tb/publications/global_report/en/. [Cited in This Article: ] |
| 2. | EuroTB, National Coordinators for Tuberculosis Surveillance in the WHO European Region. Surveillance of tuberculosis in Europe. Report on tuberculosis cases notified in 2006. 2008; Available from: http://www.ecdc.europa.eu/en/publications/Publications/SUR_TB_EuroTB_Annual_report_2006.pdf. [Cited in This Article: ] |
| 3. | Alvarez Conde JL, Gutiérrez Alonso VM, Del Riego Tomás J, García Martínez I, Arizcun Sánchez-Morate A, Vaquero Puerta C. [Perianal ulcers of tubercular origin. A report of 3 new cases]. Rev Esp Enferm Dig. 1992;81:46-48. [PubMed] [Cited in This Article: ] |
| 4. | Yaghoobi R, Khazanee A, Bagherani N, Tajalli M. Gastrointestinal tuberculosis with anal and perianal involvement misdiagnosed as Crohn’s disease for 15 years. Acta Derm Venereol. 2011;91:348-349. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Sultan S, Azria F, Bauer P, Abdelnour M, Atienza P. Anoperineal tuberculosis: diagnostic and management considerations in seven cases. Dis Colon Rectum. 2002;45:407-410. [PubMed] [Cited in This Article: ] |
| 6. | Tanemura H, Goto T, Takatuka J, Nakazaki H, Teramoto R. The case of anal fistula in which Mycobaterium tuberculosis was identified. Nippon Daicho Koonbyo Gakkaishi. 2006;59:91-95. [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Ibn Majdoub Hassani K, Ait Laalim S, Toughrai I, Mazaz K. Perianal tuberculosis: a case report and a review of the literature. Case Rep Infect Dis. 2012;2012:852763. [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Adhami S, Duthie G, Greenstone M. A tuberculous anal fistula. J R Soc Med. 1999;92:467-468. [PubMed] [Cited in This Article: ] |
| 9. | Yano K, Okazaki Y, Etoh R, Nagata T. A case of the anal carcinoma coexisting with Tuberculotic anal fistula. Jpn Gastroenterol Surg. 1997;30:1819-1822. [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Ohse H, Ishii Y, Saito T, Watanabe S, Fukai S, Yanai N, Tamai N, Monma Y, Hasegawa S. [A case of pulmonary tuberculosis associated with tuberculous fistula of anus]. Kekkaku. 1995;70:385-388. [PubMed] [Cited in This Article: ] |
| 11. | Harland RW, Varkey B. Anal tuberculosis: report of two cases and literature review. Am J Gastroenterol. 1992;87:1488-1491. [PubMed] [Cited in This Article: ] |
| 12. | Candela F, Serrano P, Arriero JM, Teruel A, Reyes D, Calpena R. Perianal disease of tuberculous origin: report of a case and review of the literature. Dis Colon Rectum. 1999;42:110-112. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 13. | Favuzza J, Brotman S, Doyle DM, Counihan TC. Tuberculous fistulae in ano: a case report and literature review. J Surg Educ. 2008;65:225-228. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 14. | Monsel G, Martinez V, Izzedine H, Mory B, Bricaire F, Caumes E. Anal tuberculosis complicated by secondary amyloidosis. Med Mal Infect. 2011;41:264-266. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Tai WC, Hu TH, Lee CH, Chen HH, Huang CC, Chuah SK. Ano-perianal tuberculosis: 15 years of clinical experiences in Southern Taiwan. Colorectal Dis. 2010;12:e114-e120. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Isaac José Felippe Corrêa Neto, Otávio Nunes Siá, Eduardo Augusto Lopes, Rodrigo Luiz Macacari, Hugo Henriques Watté, Rogério Freitas Lino Souza, Alexander Sá Rolim, Laércio Robles. Perianal tuberculosis: A rare disease of late diagnosis. Coloproctology. 2014;34:124-127. [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Onizuka O, Kawano M, Aso S. [A case of tuberculous anal fistulae complicated by pulmonary tuberculous]. Kekkaku. 1994;69:689-692. [PubMed] [Cited in This Article: ] |
| 18. | Akgun E, Tekin F, Ersin S, Osmanoglu H. Isolated perianal tuberculosis. Neth J Med. 2005;63:115-117. [PubMed] [Cited in This Article: ] |
| 19. | Maruyama R, Nakano G, Noguchi T, Uchida Y. A case of Tuberculous anal ulcer. JCO. 2000;53:269-272. [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 20. | Gupta PJ. A case of multiple (eight external openings) tubercular anal fistulae. Case report. Eur Rev Med Pharmacol Sci. 2007;11:359-361. [PubMed] [Cited in This Article: ] |
| 21. | Kraemer M, Gill SS, Seow-Choen F. Tuberculous anal sepsis: report of clinical features in 20 cases. Dis Colon Rectum. 2000;43:1589-1591. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 22. | Antonello VS, Hoff LS, Kaercher Jr D, Santos BR. Anoperineal tuberculosis in an HIV patient. Braz J Infect Dis. 2009;13:246-247. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Miteva L, Bardarov E. Perianal tuberculosis: a rare case of skin ulceration? Acta Derm Venereol. 2002;82:481-482. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Ozarmagan G, Keles S, Yazganoglu KD, Sokucu N. Delayed diagnosis in a case of perianal tuberculosis: differential diagnosis in perianal ulceration. Indian J Dermatol. 2010;55:309-310. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Bokhari I, Shah SS, Inamullah Z, Ali SU, Khan A. Tubercular fistula-in-ano. J Coll Physicians Surg Pak. 2008;18:401-403. [PubMed] [Cited in This Article: ] |
| 26. | Choi SR, Kim JK, Kim DH, Yoon MS. A case of tuberculosis cutis orificialis with perianal involvement. Ann Dermatol. 2009;21:443-446. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 27. | Leon-Mateos A, Sánchez-Aguilar D, Lado F, Toribio J. Perianal ulceration: a case of tuberculosis cutis orificialis. J Eur Acad Dermatol Venereol. 2005;19:364-366. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Menezes N, Waingankar VS. Solitary rectal ulcer of tuberculous origin (a case report). J Postgrad Med. 1989;35:118-119. [PubMed] [Cited in This Article: ] |
| 29. | Chung CC, Choi CL, Kwok SP, Leung KL, Lau WY, Li AK. Anal and perianal tuberculosis: a report of three cases in 10 years. J R Coll Surg Edinb. 1997;42:189-190. [PubMed] [Cited in This Article: ] |
| 30. | Hideura S, Neki I, Sawada H, Kudo A. A case of anal carcinoma coexisting with prolonged Tuberculotic Anal Fistula in Japanse. Shujyutsu. 1985;39:1443-1446. [Cited in This Article: ] |
| 31. | Flint FB, Passaro E. Carcinoma associated with tuberculous anorectal fistula. Am J Surg. 1970;120:397-399. [PubMed] [Cited in This Article: ] |
| 32. | Nadal SR, Manzione CR. Diagnostico e tratamento da tuberculoseanoperianal. Rev Assoc Med Bras. 2002;48:93-117. [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 33. | Available from: http://www.fukushihoken.metro.tokyo.jp/iryo/kansen/toushin.files/k_keikaku02.pdf. [Cited in This Article: ] |
| 34. | McLaughlin SI, Spradling P, Drociuk D, Ridzon R, Pozsik CJ, Onorato I. Extensive transmission of Mycobacterium tuberculosis among congregated, HIV-infected prison inmates in South Carolina, United States. Int J Tuberc Lung Dis. 2003;7:665-672. [PubMed] [Cited in This Article: ] |
| 35. | Centers for Disease Control and Prevention (CDC). Tuberculosis outbreak associated with a homeless shelter - Kane County, Illinois, 2007-2011. MMWR Morb Mortal Wkly Rep. 2012;61:186-189. [PubMed] [Cited in This Article: ] |
| 36. | Blumberg HM, Watkins DL, Berschling JD, Antle A, Moore P, White N, Hunter M, Green B, Ray SM, McGowan JE. Preventing the nosocomial transmission of tuberculosis. Ann Intern Med. 1995;122:658-663. [PubMed] [DOI] [Full Text] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in RCA: 113] [Article Influence: 3.8] [Reference Citation Analysis (0)] |