Published online Sep 16, 2015. doi: 10.12998/wjcc.v3.i9.835
Peer-review started: March 12, 2015
First decision: April 27, 2015
Revised: May 15, 2015
Accepted: June 15, 2015
Article in press: June 16, 2015
Published online: September 16, 2015
Processing time: 189 Days and 7.5 Hours
The end-stage renal disease population poses a challenge for obtaining venous access required for life-saving invasive cardiac procedures. In this case report, we describe an adult patient with end-stage renal disease in whom the hepatic vein was the only available access to implant a single-lead permanent cardiac pacemaker. A 63-year-old male with end-stage renal disease on maintenance hemodialysis and permanent atrial fibrillation/atrial flutter presented with symptomatic bradycardia. Imaging studies revealed all traditional central venous access sites to be occluded/non-accessible. With the assistance of vascular interventional radiology, a trans-hepatic venous catheter was placed. This was then used to place a right ventricular pacing lead with close attention to numerous technical aspects. The procedure was completed successfully with placement of a single-lead permanent cardiac pacemaker.
Core tip: End-stage renal disease patients pose a great challenge to establish central venous access. In situations when life-saving cardiac procedures are required in such patients, the clinician must use non-traditional venous access sites to perform these procedures. In our case report, we illustrate the novel use of the trans-hepatic venous access route to implant a single-lead permanent cardiac pacemaker in a patient with bradycardia and hypotension. Additionally, we describe the technical challenges associated with this procedure.
- Citation: Siddiqui AM, Harris GS, Movahed A, Chiang KS, Chelu MG, Nekkanti R. Transhepatic venous approach to permanent pacemaker placement in a patient with limited central venous access. World J Clin Cases 2015; 3(9): 835-837
- URL: https://www.wjgnet.com/2307-8960/full/v3/i9/835.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i9.835
The end-stage renal disease population poses a challenge for obtaining venous access required for invasive cardiac procedures due to placement of multiple arteriovenous fistulas for hemodialysis access or venous thrombus formation. The left subclavian vein is the preferred venous access for implantation of a pacing lead, but in patients with limited access alternative approaches include the right subclavian vein[1] and iliac veins[2]. In this case report, we describe an adult patient with end-stage renal disease in whom the hepatic vein was the only available access to implant a single-lead permanent cardiac pacemaker.
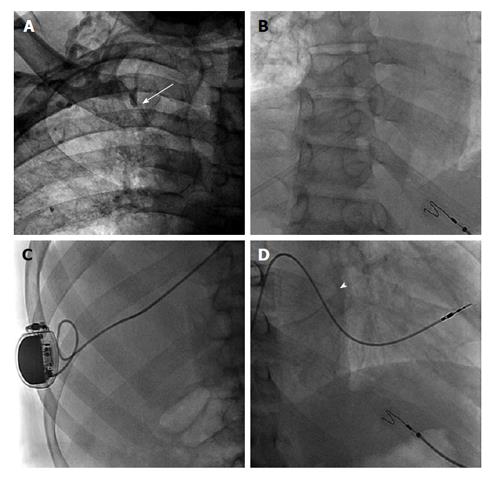
A 63-year-old African American male with end-stage renal disease on maintenance hemodialysis for 10 years and permanent atrial fibrillation/atrial flutter presented with symptoms of bradycardia including lightheadedness and dizziness. Ventricular rate was between 30 to 40 beats per minute. Hypotension was noted during dialysis sessions with a lack of positive dromotropic response due to atrioventricular node dysfunction. Non-functioning arteriovenous fistulas were present in the left upper and left lower extremities. A right lower extremity arteriovenous fistula was being used for hemodialysis access. Contrast venography of the right chest revealed an occluded right innominate vein (Figure 1A). Vascular interventional radiology placed a 6 French/45 cm Berenstein catheter (Boston Scientific, Inc., Marlborough, MA, United States) via the right peripheral hepatic vein terminating in the right atrium (RA). In the cardiac electrophysiology lab this catheter was exchanged over a 0.81 mm wire with placement of a 7 French/25 cm peel away introducer sheath into the RA, Figure 1B. The right ventricular pacing electrode with a soft curved (hockey stick curve) stylet was advanced through the sheath into the right ventricular apex. The stylet was withdrawn and the lead was advanced to provide redundancy in the RA. Sensing and pacing threshold parameters were optimal. The suture sleeve was advanced and 2 sutures were applied around the suture sleeve incorporating the indwelling muscle tissue. A subcutaneous pocket was made at the insertion point of the pacing lead. The procedure was successfully completed with no complications. A final fluoroscopic image is shown in Figure 1C.
Our main challenge was to implant a pacing lead in a symptomatic patient with no central venous access in the right and left upper extremities or right and left lower extremities. The trans-hepatic approach has been used in a variety of clinical situations where traditional central access was not possible, such as exhausted hemodialysis options[3]. Current literature states complication rates are < 5% and include line sepsis, catheter migration, thrombosis, and bleeding[4]. However, as the patient population described is so unique, the incidence rate of patients with no central venous access requiring trans-hepatic access is unknown.
One limitation of this approach is the technical aspect of inserting the lead into the right ventricle via the inferior vena cava. Additionally, the pacing lead traverses the substance of the liver, and therefore is subject to respirophasic diaphragmatic excursions potentially leading to loss of redundancy and dislodgement. Consequently, it is important to provide more than the usual redundancy in the RA to minimize dislodgement of the lead (Figure 1D).
The trans-hepatic venous approach is feasible for a single-lead permanent pacemaker implantation when all other central venous access options are exhausted.
A 63-year-old African American male with a history of end-stage renal disease on renal replacement therapy and permanent atrial fibrillation/flutter.
Symptomatic bradycardia with hypotension.
Lack of positive dromotropic response due to atrioventricular node dysfunction.
Contrast venography of the right chest revealed an occluded right innominate vein.
A single-lead permanent cardiac pacemaker was placed into the right ventricle.
The percentage of patients with end-stage renal disease with limited central venous access requiring trans-hepatic access is unknown.
This case represents demonstrates the challenge of establishing central venous access via the trans-hepatic route in a patient with no other access sites. Additionally, the authors highlight the technical challenges associated with undertaking this procedure.
The authors have performed a good study, the manuscript is interesting.
P- Reviewer: Kim ST, Rehman HU, Virk JS S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
| 1. | Jović Z, Mijailović Z, Obradović S, Tavciovski D, Matunović R, Rusović S, Djurić P. Successful implantation of a permanent pacemaker through a persistent left superior vena cava by using a right subclavian approach. Vojnosanit Pregl. 2011;68:792-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Erdogan O, Augostini R, Saliba W, Juratli N, Wilkoff BL. Transiliac permanent pacemaker implantation after extraction of infected pectoral pacemaker systems. Am J Cardiol. 1999;84:474-475, A9-A10. [PubMed] |
| 3. | Po CL, Koolpe HA, Allen S, Alvez LD, Raja RM. Transhepatic PermCath for hemodialysis. Am J Kidney Dis. 1994;24:590-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 42] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Stavropoulos SW, Pan JJ, Clark TW, Soulen MC, Shlansky-Goldberg RD, Itkin M, Trerotola SO. Percutaneous transhepatic venous access for hemodialysis. J Vasc Interv Radiol. 2003;14:1187-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 68] [Article Influence: 3.2] [Reference Citation Analysis (0)] |