Published online Sep 16, 2015. doi: 10.12998/wjcc.v3.i9.823
Peer-review started: November 29, 2014
First decision: December 26, 2014
Revised: April 2, 2015
Accepted: July 7, 2015
Article in press: July 8, 2015
Published online: September 16, 2015
Processing time: 290 Days and 11.4 Hours
AIM: To investigate the association between sports hernias and femoroacetabular impingement (FAI) in athletes.
METHODS: PubMed, MEDLINE, CINAHL, Embase, Cochrane Controlled Trials Register, and Google Scholar databases were electronically searched for articles relating to sports hernia, athletic pubalgia, groin pain, long-standing adductor-related groin pain, Gilmore groin, adductor pain syndrome, and FAI. The initial search identified 196 studies, of which only articles reporting on the association of sports hernia and FAI or laparoscopic treatment of sports hernia were selected for systematic review. Finally, 24 studies were reviewed to evaluate the prevalence of FAI in cases of sports hernia and examine treatment outcomes and evidence for a common underlying pathogenic mechanism.
RESULTS: FAI has been reported in as few as 12% to as high as 94% of patients with sports hernias, athletic pubalgia or adductor-related groin pain. Cam-type impingement is proposed to lead to increased symphyseal motion with overload on the surrounding extra-articular structures and muscle, which can result in the development of sports hernia and athletic pubalgia. Laparoscopic repair of sports hernias, via either the transabdominal preperitoneal or extraperitoneal approach, has a high success rate and earlier recovery of full sports activity compared to open surgery or conservative treatment. For patients with FAI and sports hernia, the surgical management of both pathologies is more effective than sports pubalgia treatment or hip arthroscopy alone (89% vs 33% of cases). As sports hernias and FAI are typically treated by general and orthopedic surgeons, respectively, a multidisciplinary approach for diagnosis and treatment is recommended for optimal treatment of patients with these injuries.
CONCLUSION: The restriction in range of motion due to FAI likely contributes to sports hernias; therefore, surgical treatment of both pathologies represents an optimal therapy.
Core tip: Sports hernia and femoroacetabular impingement (FAI) are two pathologies frequently reported in athletes, which are independently treated by general surgeons and orthopedists, respectively. An association between these two entities has recently been recognized, and this review was conducted to define the prevalence of FAI in patients with sports hernia and evaluate the proposed pathogenic mechanism connecting them. Although the range of terms used to describe groin pain throughout the literature is varied, there is a high prevalence of FAI with sports hernias, for which the treatment of both pathologies is optimal.
- Citation: Munegato D, Bigoni M, Gridavilla G, Olmi S, Cesana G, Zatti G. Sports hernia and femoroacetabular impingement in athletes: A systematic review. World J Clin Cases 2015; 3(9): 823-830
- URL: https://www.wjgnet.com/2307-8960/full/v3/i9/823.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i9.823
Groin injuries are a common occurrence in elite-level athletes, representing up to 6% of all athletic injuries[1-5]. These injuries occur as a result of running, kicking, cutting movements, or explosive turns and changes in direction, and thus impact 10%-28% of male soccer players[6-8]. One type of groin injury, called sports hernia, has been reported in 50% of athletes with groin pain lasting longer than 8 wk[9]. The most common operative finding in sports hernia is deficiency of the posterior wall of the inguinal canal[10-12], which is a consequence of underlying conjoint tendon dysfunction. Thus, demonstration of a dynamic bulge of the posterior wall on abdominal straining is a criterion for diagnosis of sports hernia. Real-time ultrasound for dynamic evaluation of the inguinal canal is currently the preferred diagnostic technique and provides good assessment of the conjoint tendon[13-15]. A bulging inguinal wall can also be imaged by dynamic computed tomography[16], though magnetic resonance imaging is more useful for detecting musculotendinous disease, osteitis pubis, and hip pathologies.
Risk factors for sports hernia include muscle imbalance[17,18] and significant limb length discrepancy (> 5 mm)[19]. In addition, labral tears, as well as decreased external and internal rotation of the hip joint may be related[20], which have been detected in pre-season soccer players[21-24], Gaelic football athletes[25], professional Australian Football League players[24], and athletes with chronic groin injury or osteitis pubis[26]. Garvey et al[13] found that half of the cases of sports hernia were associated with other conditions, including rectus abdominis wasting, osteitis pubis, conjoint tendinopathy, osteoarthritis, and neuralgia. Indeed, multiple co-existing pathologies have been reported in 27%-95% of cases of sports hernia[9,27-29], including adductor tendinosis[30] and adductor pain associated with either lower abdominal or inguinal pain[13]. Feeley et al[31] described the sports hip triad (labral tear, adductor strain, and rectus strain) as a common injury pattern in the elite athlete.
Femoroacetabular impingement (FAI) is a hip pathology where the bones of the hip are abnormally shaped. FAI reportedly occurs in a very high percentage of elite-level athletes examined for chronic groin and/or hip pain[32-34]. This suggests that the presence of FAI may be a predisposing factor for developing groin-related sports injuries or indicate a common underlying pathogenic mechanism. To more comprehensively investigate this, a systematic review was performed. Specifically, the prevalence of the concomitant presentation of FAI and sports hernias and their treatments were assessed.
PubMed, MEDLINE, CINAHL, Embase, Cochrane Controlled Trials Register, and Google Scholar databases were electronically searched using the following search terms: sports hernia, athletic pubalgia, groin pain, long-standing adductor-related groin pain, Gilmore groin, adductor pain syndrome, and FAI. After reading the titles and abstracts, a total of 196 studies, published before August 2014, were identified as potentially relevant. No formal exclusion criteria were applied but, from these studies, only articles concerning the association of sports hernia and FAI or laparoscopic treatment of sports hernia were selected. Finally, 24 studies were included in this review. The terms athletic pubalgia, long-standing adductor-related groin pain, adductor strain, and adductor pain syndrome were considered synonymous with sports hernia because conjoint and adductor tendinopathies and nerve entrapment are frequently associated with sports hernias and similarly result from pelvic instability; this pattern is frequently identified as “groin disruption injury”[14].
The results of the systematic review demonstrate that the prevalence of FAI and the associated restricted internal rotation varies widely among cases of athletic-related groin pain (Table 1)[13,32,34-38]. Whereas Meyers et al[35] found an overlap of athletic pubalgia and hip pathology in 27% of hockey players, Larson et al[39] reported that 90% of collegiate football players with hip and groin pain participating in a National Football League combine showed radiologic signs of cam- or pincer-type FAI. FAI was also found in patients with adductor tendinopathies, and Sansone et al[37] reported that, although most (75%) patients were satisfied with the results of tenotomy, the prevalence of FAI was greater in patients who were not satisfied when assessed after a median follow-up of six years.
| Ref. | Primary pathology | Prevalence (%) |
| Garvey et al[13] | Sports hernia | 121 |
| Meyers et al[35] | Athletic pubalgia | 27 |
| Schilders et al[36] | Chronic adductor-related groin pain | 34.1 |
| Weir et al[32] | Long-standing adductor-related groin pain | 94.1 |
| Nepple et al[34] | Groin strain, sports hernia, hip flexor or hamstring strain | 94.3 |
| Sansone et al[37] | Adductor tenotomy for chronic groin pain | 43.8 |
| Economopoulos et al[38] | Athletic pubalgia | 86 |
Verrall et al[24] postulated that chronic groin injuries result from increased loading and mechanical stress on the pubis symphysis and surrounding structures caused by reduced hip range of motion. Furthermore, Larson et al[39,40] hypothesized that the decreased hip range of motion from an underlying FAI promotes compensatory extra-articular patterns, which subsequently lead to osteitis pubis and athletic pubalgia. Birmingham et al[41] analyzed the three-dimensional motion of the pubic symphysis in six fresh-frozen human cadaveric pelvises to compare native and simulated cam lesion hips. They found that rotational motion was significantly increased by cam-type lesions due to the repetitive loading of the symphysis, which is one possible precursor to athletic pubalgia.
Laparoscopic mesh repair for the treatment of sports hernias can be performed using either a transabdominal preperitoneal or total extraperitoneal approach. Most studies demonstrate a > 90% success rate with these treatments, with return to full activities within 1-3 mo (Table 2)[4,10,42-50].
| Ref. | Treatment | Results | Recurrence |
| Diaco et al[42] | Preperitoneal approach (n = 96) | Return to active participation within 3-6 wk in 92/96 patients | - |
| Edelman et al[43] | Preperitoneal approach (n = 10) | Return to full activity within 4 wk in 9/10 patients | None |
| Ingoldby[44] | Laparoscopic vs conventional (n = 14 each) | Laparoscopic treatment superior: return to training in 4 wk (13/14 vs 9/14), resume full contact (3 wk vs 5 wk; P < 0.05) | Conventional: hernia, n = 1 after 22 mo; laparoscopic: pain, n = 1 after 5 mo |
| Susmallian et al[10] | Preperitoneal approach (n = 35) | Return to full activity in 34/35 patients | - |
| Srinivasan et al[45] | Extraperitoneal approach (n = 15) | Return to full activity within 4 wk in 13/15 patients | None |
| Genitsaris et al[46] | Transabdominal preperitoneal approach (n = 131) | 100% of patients returned to full activity within 2-3 wk | Pain, n = 4; hernia, n = 1 after 7 yr |
| Paajanen et al[47] | Extraperitoneal approach vs conventional treatment (n = 30 each) | Laparoscopic treatment superior: return to full activity within 3 mo (27/30 vs 8/30) | - |
| Paajanen et al[48] | Extraperitoneal approach (n = 41) | Return to full activity within 4 wk in 39/41 patients | - |
| van Veen et al[49] | Extraperitoneal approach (n = 55) | 100% of patients returned to full activity within 3 mo | - |
| Kluin et al[4] | Preperitoneal approach (n = 17) | Return to full activity within 3 mo in 13/17 patients | Minor symptoms, n = 2 after 1 yr |
| Ziprin et al[50] | Transabdominal preperitoneal approach (n = 17) | Return to full activity in 16/17 patients within a median of 42 d | Mild pain, n = 5 |
Only one case report and one retrospective case series reported on combined treatment of FAI and sports hernia. Matsuda[51] reported a case report regarding an endoscopic pubic symphysectomy in a case with bilateral FAI and recalcitrant osteitis pubis with high patient satisfaction, decreased pain, improved function, and resolution of the classic waddling gait at the 12-mo follow-up. In a retrospective study of 31 patients, Larson et al[40] found that surgical management of both pathologies leads to a greater rate of return to full sporting activities compared with sports pubalgia surgery or hip arthroscopy alone after a mean follow-up of 29 mo (89% vs 33%). In this study, whether the surgeries were performed concurrently, hip arthroscopy was performed first to avoid excessive stress placed on the pubalgia repair during positioning and traction for arthroscopy. There were no differences for return to sports or outcomes scoring for concurrent vs separate setting hip arthroscopy and sports hernia surgery. However, hip arthroscopy alone was sufficient to resolve sports pubalgia symptoms in four patients. It was postulated that the improved hip range of motion and function after FAI correction reduced the stress on extra-articular pelvic structures, thus alleviating the symptoms.
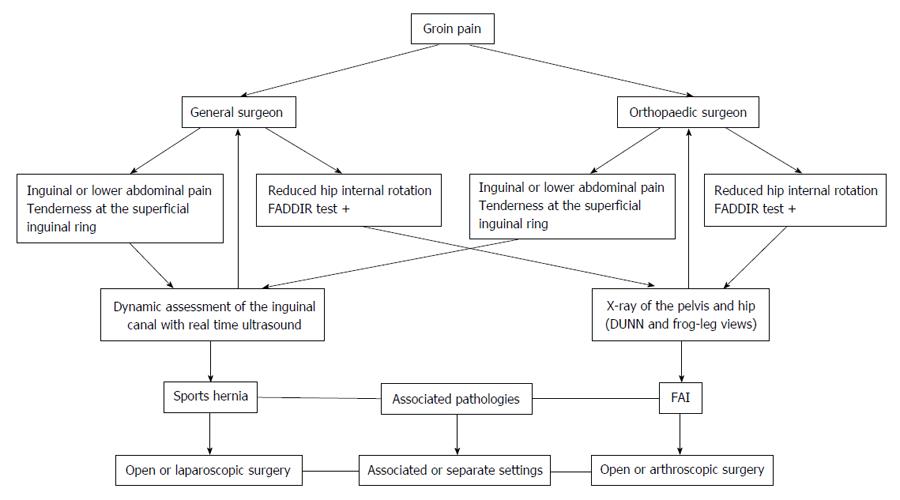
The presence of multiple pathologies does not dictate treatment outcome. The importance of treating both pathologies to obtain good and stable results during time is confirmed in a study of Hölmich et al[52], which found that active treatment of adductor-related groin pain can be effective even in the presence of morphologic changes to the hip joint. However, clinical outcome decreased over time in patients with angles > 55. A multidisciplinary approach is recommended, such as one involving orthopedic and general surgeons, to detect the presence of both pathologies in order to provide optimal treatment (Figure 1).
A wide variety of terms are used throughout the literature to describe groin pain or pubalgia, making it difficult to obtain an accurate assessment of the association between sports hernia and FAI. However, the results of this review indicate that the conditions commonly co-occur, and treatment of the underlying morphologic abnormalities can impact the sports-related symptoms.
The majority of the patients with sports hernias complain of unilateral inguinal pain or lower abdominal pain, often radiating to the pubic tubercle and the inner thigh or across the midline. Although the pain can occur after a specific event, more often the onset is insidious with exacerbation of the symptoms by activity that persists for a day or two and is temporarily relived with rest[14,53,54]. There may be pain and tenderness at the superficial inguinal ring, but without a visible or palpable lump indicative of a classical inguinal hernia. In patients with FAI, the groin pain is accompanied with pain at the greater trochanter, deep posterior buttock, and sacroiliac joint[55]. Whereas 50% of these patients reported an insidious onset, approximately 26% reported acute development of symptoms in the absence of a traumatic event. In the early stage, the pain is exacerbated with prolonged sitting or walking or with athletic activity; however, the pain becomes more constant with the progression of articular damage and osteoarthritic changes.
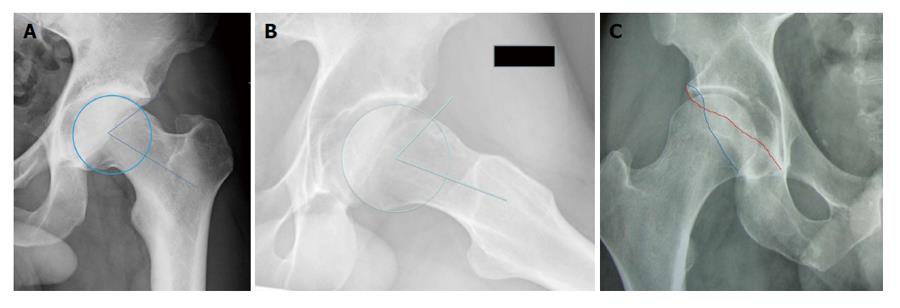
Upon physical examination, patients with FAI demonstrate pain with combined flexion, adduction, and internal rotation of the hip during the anterior impingement test[55-57], as well as during other tests of joint rotation[58]. These patients typically show restricted internal rotation and/or flexion in the hip range of motion, and restricted abduction or external rotation is also sometimes observed. Diagnosis of FAI is confirmed from radiographic exams showing an increased alpha-angle and/or signs of overcoverage or retroversion of the acetabulum (Figure 2)[56].
The additional stress from restricted rotation can lead to weakening or tearing of the transversalis fascia and surrounding tissues over time, resulting in tendon enthesitis of the adductor longus and/or abdominal muscles and groin pain[1,59,60]. This injury affects the external oblique aponeurosis, which can cause irritation of ilioinguinal or iliohypogastric nerves, as well as the conjoint tendon and inguinal ligament, resulting in weakness (deficiency) of the lower abdominal wall and occult hernias. Athletes performing rapid acceleration and deceleration movements and repetitive, high-speed twisting and cutting motions are especially vulnerable to these injuries[1,61].
Conservative treatment of sports hernias or FAI can be effective in a variable percentage of patients[62]. However, surgical treatment results in higher success rates, as demonstrated by Paajanen et al[48]. Moreover, Polglase et al[63] conducted a randomized clinical trial and found that appropriate repair of the posterior wall of the inguinal canal is superior to nonoperative management in athletes, effectively curing 60% of patients and providing improvement to an additional 20%. In a randomized study by Ekstrand et al[64], surgical treatment significantly reduced symptoms at six months compared to conservative treatment. For patients with FAI and sports hernias, surgical treatment of both pathologies appears to be the best option[40].
The surgical techniques performed to treat sports hernias are classified into three categories: open sutured repair, open mesh repair, and laparoscopic mesh repair by either transabdominal preperitoneal or extraperitoneal approaches. Sutured repairs are the most commonly performed operations for athletic pubalgia[65-68], with successful return to sport activities in 68%-100% of cases[3,5,30,60,67,69-74] and a recovery time ranging from to four weeks to three months[67,69,71,73,74]. The open anterior mesh repair technique is analogous to the Lichtenstein method of inguinal repair and is designed to reconstruct the posterior inguinal floor in a tension-free fashion. The reported success rate with this method is 77%-100%[75-79], allowing for a return to full activities within 3-4 mo[76,79]. Open or arthroscopic treatment has also been successful for treatment of FAI in athletic patients[80-83]. In addition, Dojčinović et al[30] used a shouldice technique and an ilioinguinal nerve neurolysis and resection of the genital branch of the genitofemoral nerve in a patient with untreated FAI.
The results of the present review indicate that newer laparoscopic techniques are as effective or better for successfully treating sports injuries and allowing patients to return to full activities more quickly. Compared to open surgeries, the recovery time was on the order of weeks, rather than months, and with rare incidences of recurrence. The results also suggest that athletes undergoing extraperitoneal repair do well in the postoperative period, even when a macroscopic abnormality is not detected, which is in keeping with the idea that strengthening the posterior wall relieves symptoms. There were few instances of recurrence with these techniques, however, most reports did not include a long-term follow-up.
The wide variety of terms used throughout the literature to describe groin pain and injuries complicates evaluation of the association between sports hernias and FAI. For the purposes of the present review, the terms sports hernia, athletic pubalgia, long-standing adductor-related groin pain, adductor strain, and adductor pain syndrome were considered as synonymous. However, groin pain is a common complaint of athletes with sports hernias and FAI, indicating that they may share an underlying pathogenic mechanism, such as the placement of excessive rotational stress on the pubic symphysis. Thus, surgical repair of both pathologies, likely provides the optimal treatment for elite-level athletes with these injuries.
Pubalgia and groin pain are common in athletes, and can be caused by sports hernias and femoroacetabular impingement (FAI). In the past, these were considered isolated pathologies and treated by a general or orthopedic surgeon. However, osteoarthritis and reduced hip range of movement have increasingly been observed in athletes with sports hernias, indicating that these pathologies are related.
Recently, alterations in the pelvic biomechanics due to a FAI have been described. In addition, a case series concerning the combined treatment of sports hernia and FAI was published. However, the association between FAI and sports-related groin injuries is not well defined. Therefore, the objective of this study was to systematically review articles reporting on the incidence, pathophysiology, and treatment of these two pathologies.
Recent studies report a variable association between sports hernia and FAI, ranging from 12% to 94%. To explain the association, it was proposed that increased rotational stress on the symphysis pubis and the surrounding structures from FAI leads to weakness of the posterior inguinal wall, which can result in sports hernia. The optimal treatment of athletes with sports hernias may rely on a multidisciplinary approach, involving repair of both underlying pathologies to ensure a rapid and complete return to sport activities.
This review highlights the relationship between sports hernias and FAI in athletes with groin pain, and will be useful to promote the knowledge of these pathologies for both orthopedic and general surgeons. A multidisciplinary approach is proposed to optimize the diagnosis and treatment of affected patients.
A sports hernia is defined as a dynamic bulge of the posterior wall upon abdominal straining that results from conjoint tendon dysfunction and posterior wall weakness. FAI is a hip pathology where the bones of the hip are abnormally shaped resulting in restricted rang of motion. The asphericity of the femoral head with a bump in the head-neck junction defines the cam-type impingement, whereas a deepened or retroverted acetabulum defines the pincer-type impingement. These bone abnormalities result in repetitive collision between the femoral neck and the acetabular rim, which damages the labrum and surrounding cartilage.
This review describes recent reports concerning FAI in cases of sports hernia. The co-occurrence of the two conditions indicates a common underlying pathology. This article provides a review of studies using laparoscopic techniques to repair sports hernias and indicates that concurrent treatment of FAI is optimal for earlier recovery and return to full activity.
P- Reviewer: Anazawa R, Tan XR S- Editor: Tian YL L- Editor: A E- Editor: Liu SQ
| 1. | Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med. 2001;29:521-533. [PubMed] |
| 2. | Fon LJ, Spence RA. Sportsman’s hernia. Br J Surg. 2000;87:545-552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 77] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Gilmore J. Groin pain in the soccer athlete: fact, fiction, and treatment. Clin Sports Med. 1998;17:787-793, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 155] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 4. | Kluin J, den Hoed PT, van Linschoten R, IJzerman JC, van Steensel CJ. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med. 2004;32:944-949. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 5. | Malycha P, Lovell G. Inguinal surgery in athletes with chronic groin pain: the ‘sportsman’s’ hernia. Aust N Z J Surg. 1992;62:123-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Ekstrand J, Hilding J. The incidence and differential diagnosis of acute groin injuries in male soccer players. Scand J Med Sci Sports. 1999;9:98-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 81] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Hölmich P, Uhrskou P, Ulnits L, Kanstrup IL, Nielsen MB, Bjerg AM, Krogsgaard K. Effectiveness of active physical training as treatment for long-standing adductor-related groin pain in athletes: randomised trial. Lancet. 1999;353:439-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 322] [Cited by in RCA: 245] [Article Influence: 9.4] [Reference Citation Analysis (2)] |
| 8. | Morelli V, Weaver V. Groin injuries and groin pain in athletes: part 1. Prim Care. 2005;32:163-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Aust J Sci Med Sport. 1995;27:76-79. [PubMed] |
| 10. | Susmallian S, Ezri T, Elis M, Warters R, Charuzi I, Muggia-Sullam M. Laparoscopic repair of “sportsman’s hernia” in soccer players as treatment of chronic inguinal pain. Med Sci Monit. 2004;10:CR52-CR54. [PubMed] |
| 11. | Kesek P, Ekberg O, Westlin N. Herniographic findings in athletes with unclear groin pain. Acta Radiol. 2002;43:603-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Schuricht A, Haut E, Wetzler M. Surgical options in the treatment of sports hernia. Oper Tech Spots Med. 2002;10:224-227. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Garvey JF, Hazard H. Sports hernia or groin disruption injury? Chronic athletic groin pain: a retrospective study of 100 patients with long-term follow-up. Hernia. 2014;18:815-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Garvey JF, Read JW, Turner A. Sportsman hernia: what can we do? Hernia. 2010;14:17-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 57] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Orchard JW, Read JW, Neophyton J, Garlick D. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. Br J Sports Med. 1998;32:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 97] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Garvey JF. Computed tomography scan diagnosis of occult groin hernia. Hernia. 2012;16:307-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Tyler TF, Nicholas SJ, Campbell RJ, McHugh MP. The association of hip strength and flexibility with the incidence of adductor muscle strains in professional ice hockey players. Am J Sports Med. 2001;29:124-128. [PubMed] |
| 18. | Cowan SM, Schache AG, Brukner P, Bennell KL, Hodges PW, Coburn P, Crossley KM. Delayed onset of transversus abdominus in long-standing groin pain. Med Sci Sports Exerc. 2004;36:2040-2045. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 92] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Pereira CS, de Camargo Neves Sacco I. Is structural and mild leg length discrepancy enough to cause a kinetic change in runners’ gait? ActaOrthop Bras. 2008;16:28-31. |
| 20. | Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 837] [Cited by in RCA: 819] [Article Influence: 48.2] [Reference Citation Analysis (0)] |
| 21. | Verrall GM, Slavotinek JP, Barnes PG, Fon GT. Description of pain provocation tests used for the diagnosis of sports-related chronic groin pain: relationship of tests to defined clinical (pain and tenderness) and MRI (pubic bone marrow oedema) criteria. Scand J Med Sci Sports. 2005;15:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Ibrahim A, Murrell GA, Knapman P. Adductor strain and hip range of movement in male professional soccer players. J Orthop Surg (Hong Kong). 2007;15:46-49. [PubMed] |
| 23. | Verrall GM, Hamilton IA, Slavotinek JP, Oakeshott RD, Spriggins AJ, Barnes PG, Fon GT. Hip joint range of motion reduction in sports-related chronic groin injury diagnosed as pubic bone stress injury. J Sci Med Sport. 2005;8:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 78] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 24. | Verrall GM, Slavotinek JP, Barnes PG, Esterman A, Oakeshott RD, Spriggins AJ. Hip joint range of motion restriction precedes athletic chronic groin injury. J Sci Med Sport. 2007;10:463-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 113] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 25. | Nevin F, Delahunt E. Adductor squeeze test values and hip joint range of motion in Gaelic football athletes with longstanding groin pain. J Sci Med Sport. 2014;17:155-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 68] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 26. | Williams JG. Limitation of hip joint movement as a factor in traumatic osteitis pubis. Br J Sports Med. 1978;12:129-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 64] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Ekberg O, Persson NH, Abrahamsson PA, Westlin NE, Lilja B. Longstanding groin pain in athletes. A multidisciplinary approach. Sports Med. 1988;6:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 135] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 28. | Rochcongar P, Le Gall F, Jan J. Pubalgie du sportif: mise au point a propos d’une etude retrospectivede 214 patients (Pubic pain in athletes: a review and a retrospective study of 214 patients). Sci Sports (Paris). 1996;11:135-139. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Ekberg O, Blomquist P, Fritzdorf J. Herniography in patients with clinically suggested recurrence of inguinal hernia. Acta Radiol Diagn (Stockh). 1984;25:225-229. [PubMed] |
| 30. | Dojčinović B, Sebečić B, Starešinić M, Janković S, Japjec M, Čuljak V. Surgical treatment of chronic groin pain in athletes. Int Orthop. 2012;36:2361-2365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 31. | Feeley BT, Powell JW, Muller MS, Barnes RP, Warren RF, Kelly BT. Hip injuries and labral tears in the national football league. Am J Sports Med. 2008;36:2187-2195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 131] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 32. | Weir A, de Vos RJ, Moen M, Hölmich P, Tol JL. Prevalence of radiological signs of femoroacetabular impingement in patients presenting with long-standing adductor-related groin pain. Br J Sports Med. 2011;45:6-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 33. | Kapron AL, Anderson AE, Aoki SK, Phillips LG, Petron DJ, Toth R, Peters CL. Radiographic prevalence of femoroacetabular impingement in collegiate football players: AAOS Exhibit Selection. J Bone Joint Surg Am. 2011;93:e111(1-e1110). [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 170] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 34. | Nepple JJ, Brophy RH, Matava MJ, Wright RW, Clohisy JC. Radiographic findings of femoroacetabular impingement in National Football League Combine athletes undergoing radiographs for previous hip or groin pain. Arthroscopy. 2012;28:1396-1403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 35. | Meyers WC, Yoo E, Devon ON, Jain N, Horner M, Lauencin C, Zoga A. Understanding “Sports hernia” (Athletic Pubalgia): The Anatomic and Pathophysiologic Basis for Abdominal and Groin Pain in Athletes. Oper Tech Sports Med. 2007;15:165-177. [RCA] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 36. | Schilders E, Dimitrakopoulou A, Cooke M, Bismil Q, Cooke C. Effectiveness of a selective partial adductor release for chronic adductor-related groin pain in professional athletes. Am J Sports Med. 2013;41:603-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 41] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 37. | Sansone M, Ahldén M, Jonasson P, Thomeé R, Falk A, Swärd L, Karlsson J. Can hip impingement be mistaken for tendon pain in the groin? A long-term follow-up of tenotomy for groin pain in athletes. Knee Surg Sports Traumatol Arthrosc. 2014;22:786-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Economopoulos KJ, Milewski MD, Hanks JB, Hart JM, Diduch DR. Radiographic evidence of femoroacetabular impingement in athletes with athletic pubalgia. Sports Health. 2014;6:171-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 39. | Larson CM, Sikka RS, Sardelli MC, Byrd JW, Kelly BT, Jain RK, Giveans MR. Increasing alpha angle is predictive of athletic-related “hip” and “groin” pain in collegiate National Football League prospects. Arthroscopy. 2013;29:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 108] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 40. | Larson CM, Pierce BR, Giveans MR. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/sports hernia: a case series. Arthroscopy. 2011;27:768-775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 135] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 41. | Birmingham PM, Kelly BT, Jacobs R, McGrady L, Wang M. The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. Am J Sports Med. 2012;40:1113-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 79] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 42. | Diaco JF, Diaco DS, Lockhart L. Sports hernia. Oper Tech Sports Med. 2005;13:68-70. [RCA] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 43. | Edelman DS, Selesnick H. “Sports” hernia: treatment with biologic mesh (Surgisis): a preliminary study. Surg Endosc. 2006;20:971-973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 44. | Ingoldby CJ. Laparoscopic and conventional repair of groin disruption in sportsmen. Br J Surg. 1997;84:213-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 78] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 45. | Srinivasan A, Schuricht A. Long-term follow-up of laparoscopic preperitoneal hernia repair in professional athletes. J Laparoendosc Adv Surg Tech A. 2002;12:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 46. | Genitsaris M, Goulimaris I, Sikas N. Laparoscopic repair of groin pain in athletes. Am J Sports Med. 2004;32:1238-1242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 47. | Paajanen H, Brinck T, Hermunen H, Airo I. Laparoscopic surgery for chronic groin pain in athletes is more effective than nonoperative treatment: a randomized clinical trial with magnetic resonance imaging of 60 patients with sportsman’s hernia (athletic pubalgia). Surgery. 2011;150:99-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 106] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 48. | Paajanen H, Syvähuoko I, Airo I. Totally extraperitoneal endoscopic (TEP) treatment of sportsman’s hernia. Surg Laparosc Endosc Percutan Tech. 2004;14:215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 49. | van Veen RN, de Baat P, Heijboer MP, Kazemier G, Punt BJ, Dwarkasing RS, Bonjer HJ, van Eijck CH. Successful endoscopic treatment of chronic groin pain in athletes. Surg Endosc. 2007;21:189-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 50. | Ziprin P, Prabhudesai SG, Abrahams S, Chadwick SJ. Transabdominal preperitoneal laparoscopic approach for the treatment of sportsman’s hernia. J Laparoendosc Adv Surg Tech A. 2008;18:669-672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 51. | Matsuda DK. Endoscopic pubic symphysectomy for reclacitrant osteitis pubis associated with bilateral femoroacetabular impingement. Orthopedics. 2010;33:Epub 2010 Mar 10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 52. | Hölmich P, Thorborg K, Nyvold P, Klit J, Nielsen MB, Troelsen A. Does bony hip morphology affect the outcome of treatment for patients with adductor-related groin pain? Outcome 10 years after baseline assessment. Br J Sports Med. 2014;48:1240-1244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 53. | Moeller JL. Sportsman’s hernia. Curr Sports Med Rep. 2007;6:111-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 54. | Swan KG, Wolcott M. The athletic hernia: a systematic review. Clin Orthop Relat Res. 2007;455:78-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 55. | Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041-1047. [PubMed] |
| 56. | Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;112-120. [PubMed] |
| 57. | Sink EL, Gralla J, Ryba A, Dayton M. Clinical presentation of femoroacetabular impingement in adolescents. J Pediatr Orthop. 2008;28:806-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 58. | Martin HD, Kelly BT, Leunig M, Philippon MJ, Clohisy JC, Martin RL, Sekiya JK, Pietrobon R, Mohtadi NG, Sampson TG. The pattern and technique in the clinical evaluation of the adult hip: the common physical examination tests of hip specialists. Arthroscopy. 2010;26:161-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 148] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 59. | Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med. 1993;27:58-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 147] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 60. | Morales-Conde S, Socas M, Barranco A. Sportsmen hernia: what do we know? Hernia. 2010;14:5-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 61. | LeBlanc KE, LeBlanc KA. Groin pain in athletes. Hernia. 2003;7:68-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 82] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 62. | Wall PD, Fernandez M, Griffin DR, Foster NE. Nonoperative treatment for femoroacetabular impingement: a systematic review of the literature. PM R. 2013;5:418-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 128] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 63. | Polglase AL, Frydman GM, Farmer KC. Inguinal surgery for debilitating chronic groin pain in athletes. Med J Aust. 1991;155:674-677. [PubMed] |
| 64. | Ekstrand J, Ringborg S. Surgery versus conservative treatment in soccer players with chronic groin pain: a prospective randomized study in soccer players. Eur J TraumatolRel Res. 2001;23:141-145. |
| 65. | Nam A, Brody F. Management and therapy for sports hernia. J Am Coll Surg. 2008;206:154-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 66. | Muschaweck U, Berger L. Minimal Repair technique of sportsmen’s groin: an innovative open-suture repair to treat chronic inguinal pain. Hernia. 2010;14:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 67. | Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28:2-8. [PubMed] |
| 68. | Caudill P, Nyland J, Smith C, Yerasimides J, Lach J. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 69. | Meyers WC, McKechnie A, Philippon MJ, Horner MA, Zoga AC, Devon ON. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;248:656-665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 105] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 70. | Messaoudi N, Jans C, Pauli S, Van Riet R, Declercq G, Van Cleemput M. Surgical management of sportsman’s hernia in professional soccer players. Orthopedics. 2012;35:e1371-e1375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 71. | Taylor DC. Abdominal musculature abnormalities as a cause of groin pain in athletes. Am J Sports Med. 1991;19:421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 147] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 72. | Brannigan AE, Kerin MJ, McEntee GP. Gilmore’s groin repair in athletes. J Orthop Sports Phys Ther. 2000;30:329-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 73. | Muschaweck U, Berger LM. Sportsmen’s Groin-Diagnostic Approach and Treatment With the Minimal Repair Technique: A Single-Center Uncontrolled Clinical Review. Sports Health. 2010;2:216-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 74. | Williams P, Foster ME. ‘Gilmore’s groin’--or is it? Br J Sports Med. 1995;29:206-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 75. | Brown RA, Mascia A, Kinnear DG, Lacroix V, Feldman L, Mulder DS. An 18-year review of sports groin injuries in the elite hockey player: clinical presentation, new diagnostic imaging, treatment, and results. Clin J Sport Med. 2008;18:221-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 76. | Preskitt JT. Sports hernia: the experience of Baylor University Medical Center at Dallas. Proc (Bayl Univ Med Cent). 2011;24:89-91. [PubMed] |
| 77. | Joesting DR. Diagnosis and treatment of sportsman’s hernia. Curr Sports Med Rep. 2002;1:121-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 78. | Irshad K, Feldman LS, Lavoie C, Lacroix VJ, Mulder DS, Brown RA. Operative management of “hockey groin syndrome”: 12 years of experience in National Hockey League players. Surgery. 2001;130:759-764; discussion 764-766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 100] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 79. | Steele P, Annear P, Grove JR. Surgery for posterior inguinal wall deficiency in athletes. J Sci Med Sport. 2004;7:415-421; discussion 422-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 80. | Papalia R, Del Buono A, Franceschi F, Marinozzi A, Maffulli N, Denaro V. Femoroacetabular impingement syndrome management: arthroscopy or open surgery? Int Orthop. 2012;36:903-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 81. | Byrd JW, Jones KS. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med. 2009;37:2140-2143. [PubMed] |
| 82. | Philippon MJ, Yen YM, Briggs KK, Kuppersmith DA, Maxwell RB. Early outcomes after hip arthroscopy for femoroacetabular impingement in the athletic adolescent patient: a preliminary report. J Pediatr Orthop. 2008;28:705-710. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 140] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 83. | Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39 Suppl:14S-19S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 198] [Article Influence: 14.1] [Reference Citation Analysis (0)] |