Published online Jul 16, 2015. doi: 10.12998/wjcc.v3.i7.655
Peer-review started: July 12, 2014
First decision: August 14, 2014
Revised: March 3, 2015
Accepted: April 10, 2015
Article in press: April 14, 2015
Published online: July 16, 2015
Processing time: 380 Days and 14.8 Hours
Postural orthostatic tachycardia syndrome (POTS) is a relatively rare syndrome recognised since 1940. It is a heterogenous condition with orthostatic intolerance due to dysautonomia and is characterised by rise in heart rate above 30 bpm from base line or to more than 120 bpm within 5-10 min of standing with or without change in blood pressure which returns to base line on resuming supine position. This condition present with various disabling symptoms such as light headedness, near syncope, fatigue, nausea, vomiting, tremor, palpitations and mental clouding, etc. However there are no identifiable signs on clinical examination and patients are often diagnosed to have anxiety disorder. The condition predominantly affects young female between the ages of 15-50 but is rarely described in older people. We describe an older patient who developed POTS which recovered over 12 mo. Recognising this condition is important as there are treatment options available to alleviate the disabling symptoms.
Core tip: This is a short report and literature review on postural orthostatic tachycardia syndrome (POTS). POTS commonly affects younger patients and is rarely reversible. Here we describe an older patient who presented with disabling POTS which was reversed. Although rare, it is now being recognised in older people and increasing awareness among geriatricians is important as early diagnosis and treatment may alleviate the disabling symptoms. Reviewing the literature we argue whether hypotension should be considered as a feature of POTS.
- Citation: Abdulla A, Rajeevan T. Reversible postural orthostatic tachycardia syndrome. World J Clin Cases 2015; 3(7): 655-660
- URL: https://www.wjgnet.com/2307-8960/full/v3/i7/655.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i7.655
Postural orthostatic tachycardia syndrome (POTS) is an orthostatic intolerance due to dysautonomia. This heterogeneous group of syndromes is characterised by rise in heart rate above 30 bpm from base line or to more than 120 bpm within 5-10 min of standing with or without change in blood pressure. This condition present with various disabling symptoms such as light headedness, near syncope, fatigue, nausea, vomiting, tremor, palpitations and mental clouding, etc. Various pathophysiological mechanisms have been recognised. It commonly affects younger patients and is rarely reversible. However it has been recognised in older people too. Recognising this condition is important as there are treatment options available to alleviate the disabling symptoms.
A 70-year-old woman presented with an 8 mo history of dizziness on standing and unsteadiness on her feet. More recently she experienced a fall and several near falls. She complained of nausea resistant to antiemetics and weight loss. She felt generally weak and had become dependent for all her activities of daily living. She had a brief hospital admission 10 mo prior to the current presentation and was investigated for the persistent nausea and vomiting. Upper gastrointestinal endoscopy, barium swallow and computed tomography scan of abdomen, pelvis and chest showed no identifiable pathology.
She had past medical history of polymyalgia rheumatica, hypertension and anxiety. She was on maintenance dose of prednisolone 1 mg, ramipril 2.5 mg and diazepam at night. She lived with her husband, previously independent for her activities of daily living, was a non smoker and consumed alcohol occasionally.
On assessment she appeared anxious and was lethargic. Her heart rate was 80 bpm regular. Blood pressure was 179/85 mmHg sitting and 119/73 mmHg on standing associated with rise in heart rate to120 bpm. She complained of dizziness on standing. Systemic examination including cardiovascular and neurological examinations was unremarkable.
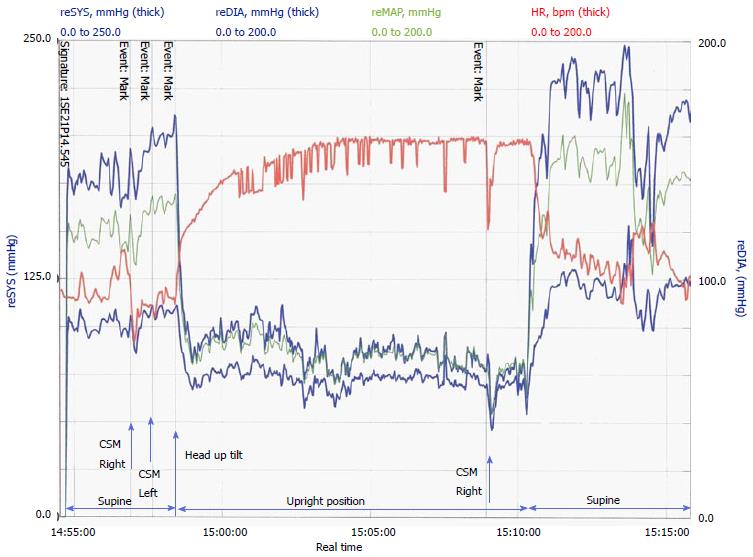
Routine blood tests including thyroid function tests and random cortisol were normal. Twenty-four hours urine collections on 4 consecutive days for 5-hydroxyindoleacetic acid (5HIAA), cortisol, dopamine, epinephrine, norepinephrine and sodium were sent. 5HIAA excretion was elevated on 2 occasions to 49 and 99 micromol/d (normal 10-42) as was excretion of epinephrine to 190 nmol/d (normal 0-144). Elevation of catecholamines was possibly related to hyperadrenergic condition and significance of 5HIAA elevation was unexplained as it returned to normal in subsequent assays. Twelve lead electrocardiogram (ECG) and 24 h tape showed sinus rhythm. An echocardiogram showed signs of left ventricular hypertrophy. She underwent tilt table test which showed a rise in heart rate above 30 bpm from baseline associated with fall in blood pressure (Figure 1).
She was commenced on propranolol 10 mg tds and fludrocortisone at a starting dose of 50 mcg daily which was increased to 150 mcg. She responded remarkably well; her postural tachycardia resolved with improvement in symptoms of dizziness and nausea. She gradually regained her mobility and was able to resume her personal activities.
All the endocrine tests were repeated after 2 mo of her recovery of symptoms. All her baseline endocrine tests were normal at this point.
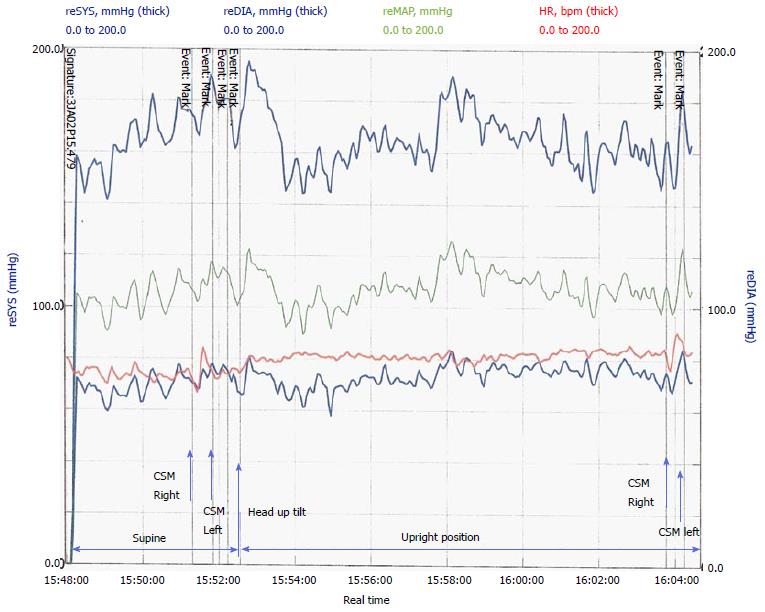
On follow up at 4 mo her blood pressure was 150/70 mmHg. She was slowly weaned off fludrocortisone with no recurrence of symptoms. Head up tilt test was repeated at 15 mo (Figure 2) which showed complete recovery and no change in heart rate or blood pressure with postural change.
POTS is a relatively rare syndrome recognised since 1940[1,2] . It is most often seen in women of child bearing age (between the ages of 15 and 50), nevertheless it may appear at any age. This is rarely described in older people and pathophysiology can be significantly different in older group of people. The mechanism depends on underlying pathology. It is not always easy to identify the mechanism therefore treatment can be difficult.
Standing results in approximately 0.5 to 1.0 L of blood pooling in the lower extremities and splanchnic circulation. A normal hemodynamic response to postural change requires normal function of the cardiovascular and autonomic nervous systems. An increase in sympathetic outflow, increases peripheral vascular resistance, venous return, and cardiac output, limiting the decrease in blood pressure. Normal compensatory mechanisms result in a decrease in systolic blood pressure (5 to 10 mmHg), an increase in diastolic blood pressure (5 to 10 mmHg), and an increase in pulse rate (10 to 25 beats per minute). Orthostatic hypotension is defined as a decrease in systolic blood pressure of 20 mmHg or a decrease in diastolic blood pressure of 10 mmHg within three minutes of standing compared with blood pressure from the sitting or supine position.
POTS is an orthostatic intolerance due to dysautonomia and is divided into primary and secondary types. It is important to identify the type to facilitate treatment. By definition the primary form occurs in the absence of an underlying condition. In contrast the secondary form of POTS is due to chronic conditions such as diabetes mellitus, sarcoidosis, connective tissue disorders, etc[3]. The condition runs a remitting and relapsing course.
This heterogeneous group of syndromes is characterised by rise in heart rate above 30 bpm from base line or to more than 120 bpm within 5-10 min of standing with or without change in blood pressure. In fact some authors require no change in blood pressure on standing as a pre-requisite for the diagnosis of POTS but this is controversial[2,4-7]. Many of the mechanisms described in POTS such as vasodilatation, blunted response to angiotensin II, low blood volume and red cell volume, abnormal vascular structure and venous capacitance can potentially drop the blood pressure. The drop in blood pressure due to above mechanisms may be compensated to a certain degree in POTS patients by disproportionately elevated heart rate though at times the compensation may be incomplete.
The various pathophysiological mechanisms involved in POTS are: (1) high level of standing norepinephrine level (due to reduced norepinephrine transporter expression resulting increased systemic norepinephrine spill over); (2) presence of ganglionic acetylcholine receptor antibodies; (3) alpha 1 adrenergic receptor denervation or hyposensitivity; (4) beta adrenergic super sensitivity; (5) peripheral autonomic denervation with preserved cardiac and cerebral innervations; (6) Partial renal sympathetic denervation leading to reduced renin/Aldosterone[8]; (7) increased angiotensin II level with blunted responsiveness of receptors to angiotensin II[9]; (8) Low blood volume and Red cell volume; (9) Abnormal vascular structure with impaired venous capacitance; and (10) Increased capillary permeability.
Not all of these mechanisms present in any one patient and treatment should be tailored accordingly. Symptoms are most likely due to cerebral hypoperfusion[10].
As mentioned earlier POTS patients present with varying clinical features depending on the underlying pathology. Unifying feature is orthostatic intolerance which improves on lying or sitting down. The primary form is not associated with or caused by other chronic disorders. Here the onset is usually abrupt particularly when it occurs following viral illness, immunisation, pregnancy or surgery. An exception is the developmental form which occurs following a period of rapid growth[3]. In this case it runs a slow progress to reach a peak within 2 years.
Two major types of primary forms are identified. They are partial dysautonomic and hyperadrenergic forms (Table 1). Partial dysautonomic form is due to peripheral autonomic neuropathy which results in excessive pooling of blood in blood vessels of lower limbs and mesenteric circulation with the reflex tachycardia. Antibodies to ganglionic acetylcholine receptors are often found in patients with post viral autonomic neuropathy[3,11]. In contrast the hyperadrenergic form is usually a familial condition where there is rise in norepinephrine level on standing which causes the orthostatic tachycardia and orthostatic intolerance[12]. The rise in norepinephrine is due to reduced clearance secondary to poorly functioning reuptake transporter protein[6]. These patients suffer from profuse sweating, anxiety, tremulousness, tachycardia and hypertension[12,13].
| Partial dysautonomia | Hyperadrenergic form | |
| Frequency | Most common primary form | Less common primary form |
| Mechanism | Inability of peripheral vessels to constrict | Tachycardia due to elevated catecholamine |
| Onset | Abrupt | Gradual |
| Pathophysiology | Autoimmune mediated | Familial–single point mutation |
| Investigation | Serum acetylcholine receptor antibodies | Standing catecholamine level |
Secondary forms are mainly due to chronic disorders such as diabetes mellitus, joint hyper mobility syndrome, sarcoidosis, systemic lupus syndrome, heavy metal poisoning and chemotherapies which affect the nervous system.
Various symptoms are described such as light headedness, near syncope, fatigue, nausea, vomiting, tremor, palpitations, mental clouding, etc. Symptoms can be brought on minimal exertion or activities such as eating, showering and walking short distance[2,5,14]. Both symptoms and tachycardia resolve with sitting or lying down. Patients are often diagnosed to have anxiety disorder[1,5].
Head up tilt (HUT) is the investigation of choice although some studies suggest that standing haemodynamics is more specific[2,15]. It is important to rule out other conditions which cause tachycardia such as phaeochromocytoma, carcinoid, thyrotoxicosis, cardiac arrhythmia, etc. Tachycardia in these conditions is not related to change in posture.
Important investigations are blood tests which should include full blood count, renal function, thyroid function, calcium level, glucose, catecholamines on standing from supine position. Twenty-four hours urine collection for 5HIAA, catecholamines, sodium level are relevant investigations in POTS to rule out other causes of tachycardia and aim treatment options[12]. Routinely an ECG should be performed and further investigations such as 24 h tape and echocardiogram are carried out if indicated. The fact that this syndrome is not often recognised by clinicians, it leads to unnecessary investigations before the diagnosis is made especially in older people.
Conservative: Review of medications which can aggravate POTS and appropriately stopping these medications; these include: (1) drugs that enhance vasodilatation-alpha adrenoreceptor blockers, angiotensin converting enzyme inhibitor (ACEI), calcium channel blockers and nitrates; (2) drugs that enhance tachycardia-beta adrenoreceptor stimulants, tricyclic antidepressants; and (3) drugs that worsens volume depletion-diuretics and ACEI.
Exercise - Aerobic exercise and lower limb resistance training will help pumping the blood. The intensity and duration of exercise should be built up gradually and also depend on patient’s age.
Avoid salt and fluid depletion - Increasing salt and fluid take have great impact on reducing severity of symptoms. Fluid intake of 2 L/d and salt intake of 3-5 g/d is recommended. Performing 24 h urinary collection for urinary sodium level would help to identify the patients who would benefit from salt supplements. Studies show that patients with urinary excretion < 124 mmol/d is an indicator of good response to salt treatment[16].
Pharmacological treatment: Vasoconstrictors: Fludrocortisone is the most commonly used drug in orthostatic intolerance. Its action is mediated by improving peripheral sensitivity of alpha adrenoceptors, fluid and salt retention. Midodrine is an alpha-1 adrenoreceptor agonist not only increases the peripheral vascular resistance but also helps orthostatic intolerance by having an effect on heart rate. Other vasoconstrictors used with variable results are: (1) methylphenidate - increases vasoconstriction by increasing catecholamine release and inhibiting monoamine oxidase; (2) erythropoietin: increases the sensitivity of angiotensin II; (3) clonidine is a central sympatholytic and increases peripheral vascular resistance; and (4) octreotide: somatostatin analogue is potent vasoconstrictor.
Heart rate limiting drugs: Beta blockers are the main group of drugs and among them propranolol is favoured by clinicians. There are limited studies with regards to the dosage at which it is effective in treating POTS. Moderate dose of propranolol (20 mg) not only reduces heart rate but also improves symptoms, whereas higher dose (80 mg) is effective in reducing heart rate but does not improve symptoms. In fact it has been reported to worsen symptoms[17]. Other drugs which can reduce heart rate and alleviate symptoms are selective serotonin reuptake inhibitors (SSRI) and selective noradrenalin reuptake inhibitors. SSRI have been used for cardiogenic syncope and orthostatic hypotension. Serotonin plays and important role in central control of heart rate.
Ivabradine has effect on reducing the heart rate and symptom control.
Volume expanders: As mentioned earlier fludrocortisone is a mineralocorticoid and enhances the fluid and salt retention. Erythropoietin stimulates red cell production and increase the red cell mass and blood volume. Treatment with Erythropoietin is reserved for people with refractory symptoms in spite of other medications. Cost and administration by subcutaneous injection are the limiting factors for its use. Desmopressin increases the reabsorption of fluid from kidney, but its use in POTS has not been adequately studied.
Other medications: Pyridostigmine is an acetylcholine esterase inhibitor and is a very promising drug particularly for POTS following viral illness and POTS secondary to autoimmune process and paraneoplastic syndrome.
In conclusion, POTS is a condition characterised by orthostatic intolerance with excessive increase in heart rate due to disturbances in autonomic control. Patients with this condition suffer from numerous disabling symptoms with no specific abnormalities on clinical examination. Head up tilt test is the choice of investigation. Identifying the subtypes is the key to achieve successful management.
Our patient is a rare case of POTS in older people with full recovery.
Her symptoms were severe enough to warrant hospital admission. Medications were commenced once diagnosis was established with HUT and she made good recovery with her mobility and other symptoms.
A 70-year-old woman presented with dizziness and unsteadiness on feet.
Heart rate increased to more than 30 bpm from baseline on standing associated with fall in blood pressure.
Postural hypotension and other conditions which causes tachycardia such as pheochromocytoma, thyrotoxicosis carcinoid syndrome and cardiac arrhythmia.
Head up tilt test showed rise in heart rate from 80 to 120 bpm on standing with drop in blood pressure.
Chest X-ray and computerised tomography of abdomen, pelvis and chest were normal.
The patient was treated with fludrocortisone and propranolol.
Postural orthostatic tachycardia syndrome (POTS) is described predominantly in young females and to our knowledge this is the first case reported in older person.
Head up tilt test is the tilt-table test involves placing a patient on a flat table with a foot support, then tilting the table upward for a period of time to observe changes in blood pressure and heart rate.
POTS is a rare disabling condition; but is treatable when diagnosis is established which needs high index of suspicion.
This is an interesting case report.
P- Reviewer: Trohman RG S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
| 1. | Soliman K, Sturman S, Sarkar PK, Michael A. Postural orthostatic tachycardia syndrome (POTS): A diagnostic dilemma. Br J Cardiol. 2010;17:36-39. |
| 2. | Abed H, Ball PA, Wang LX. Diagnosis and management of postural orthostatic tachycardia syndrome: A brief review. J Geriatr Cardiol. 2012;9:61-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Grubb BP, Kanjwal Y, Kosinski DJ. The postural tachycardia syndrome: a concise guide to diagnosis and management. J Cardiovasc Electrophysiol. 2006;17:108-112. [PubMed] |
| 4. | Carew S, Connor MO, Cooke J, Conway R, Sheehy C, Costelloe A, Lyons D. A review of postural orthostatic tachycardia syndrome. Europace. 2009;11:18-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Grubb BP. The postural tachycardia syndrome: A brief review of etiology, diagnosis and treatment. Hellenic J Cardiol. 2002;43:47-52. |
| 6. | Lambert E, Eikelis N, Esler M, Dawood T, Schlaich M, Bayles R, Socratous F, Agrotis A, Jennings G, Lambert G. Altered sympathetic nervous reactivity and norepinephrine transporter expression in patients with postural tachycardia syndrome. Circ Arrhythm Electrophysiol. 2008;1:103-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Thanavaro JL, Thanavaro KL. Postural orthostatic tachycardia syndrome: diagnosis and treatment. Heart Lung. 2011;40:554-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Kaufmann H, Freeman R. Postural tachycardia syndrome. Wolters Kluwer: UpToDate 2011; . |
| 9. | Mustafa HI, Garland EM, Biaggioni I, Black BK, Dupont WD, Robertson D, Raj SR. Abnormalities of angiotensin regulation in postural tachycardia syndrome. Heart Rhythm. 2011;8:422-428. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 10. | Ocon AJ, Medow MS, Taneja I, Clarke D, Stewart JM. Decreased upright cerebral blood flow and cerebral autoregulation in normocapnic postural tachycardia syndrome. Am J Physiol Heart Circ Physiol. 2009;297:H664-H673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 11. | Low PA, Sandroni P, Joyner M, Shen WK. Postural tachycardia syndrome (POTS). J Cardiovasc Electrophysiol. 2009;20:352-358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 281] [Cited by in RCA: 240] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 12. | Grubb BP. Postural tachycardia syndrome. Circulation. 2008;117:2814-2817. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Kanjwal K, Saeed B, Karabin B, Kanjwal Y, Grubb BP. Clinical presentation and management of patients with hyperadrenergic postural orthostatic tachycardia syndrome. A single center experience. Cardiol J. 2011;18:527-531. [PubMed] |
| 14. | Agarwal AK, Garg R, Ritch A, Sarkar P. Postural orthostatic tachycardia syndrome. Postgrad Med J. 2007;83:478-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 15. | Plash WB, Diedrich A, Biaggioni I, Garland EM, Paranjape SY, Black BK, Dupont WD, Raj SR. Diagnosing postural tachycardia syndrome: comparison of tilt testing compared with standing haemodynamics. Clin Sci (Lond). 2013;124:109-114. [PubMed] |
| 16. | Zhang Q, Liao Y, Tang C, Du J, Jin H. Twenty-four-hour urinary sodium excretion and postural orthostatic tachycardia syndrome. J Pediatr. 2012;161:281-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Raj SR, Black BK, Biaggioni I, Paranjape SY, Ramirez M, Dupont WD, Robertson D. Propranolol decreases tachycardia and improves symptoms in the postural tachycardia syndrome: less is more. Circulation. 2009;120:725-734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 142] [Article Influence: 8.9] [Reference Citation Analysis (0)] |