Published online May 16, 2015. doi: 10.12998/wjcc.v3.i5.442
Peer-review started: October 21, 2014
First decision: December 12, 2014
Revised: January 19, 2015
Accepted: March 18, 2015
Article in press: March 20, 2015
Published online: May 16, 2015
Processing time: 199 Days and 12.6 Hours
This article reviews the imaging anatomy of temporomandibular joint (TMJ), describes the technique of multi-detector computed tomography (MDCT) of the TMJ, and describes in detail various osseous pathologic afflictions affecting the joint. Traumatic injuries affecting the mandibular condyle are most common, followed by joint ankylosis as a sequel to arthritis. The congenital anomalies are less frequent, hemifacial microsomia being the most commonly encountered anomaly involving the TMJ. Neoplastic afflictions of TMJ are distinctly uncommon, osteochondroma being one of the most common lesions. MDCT enables comprehensive evaluation of osseous afflictions of TMJ, and is a valuable tool for surgical planning. Sagittal, coronal and 3D reformatted images well depict osseous TMJ lesions, and their relationship to adjacent structures.
Core tip: This pictorial review describes the common as well as uncommon bony afflictions of the temporomandibular joint (TMJ) with classical images. Bony afflictions of the TMJ constitute a significant bulk of lesions around this joint. However, very little literature is available on imaging evaluation of non-articular disc, osseous disorders. Computed tomography (CT) is the workhorse for evaluation of osseous lesions around the joint and this article focuses on the CT evaluation of these lesions, and also on optimal imaging strategy, which is essential for surgical planning.
- Citation: Pahwa S, Bhalla AS, Roychaudhary A, Bhutia O. Multidetector computed tomography of temporomandibular joint: A road less travelled. World J Clin Cases 2015; 3(5): 442-449
- URL: https://www.wjgnet.com/2307-8960/full/v3/i5/442.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i5.442
Temporomandibular joint (TMJ) is a complex joint essential for the uniquely human -function of speech[1], and the functions of mastication and swallowing. A number of congenital, traumatic, inflammatory, and rarely neoplastic disorders can affect the TMJ causing symptoms like pain, trismus, malocclusion and facial asymmetry. It is crucial to distinguish between different TMJ disorders as the etiology of the disorder determines the clinical course, management and prognosis.
It has been difficult to evaluate the TMJ on conventional radiographs because of overlap by bones of skull base and face. With the advent of multidetector row computed tomography (CT) technology, it has become possible to acquire thin slices, do multiplanar reformatted reconstructions, and hence image the joint in exquisite detail.
The TMJ is composed of osseous and soft tissue components[2,3]. The osseous component is formed by the temporal bone superiorly that forms the glenoid fossa and the articular tubercle, and by the mandibular condyle inferiorly. The joint capsule and the articular disc are the soft tissue components of the joint. The articular disc has a thin central part and thick anterior and posterior bands[3,4].
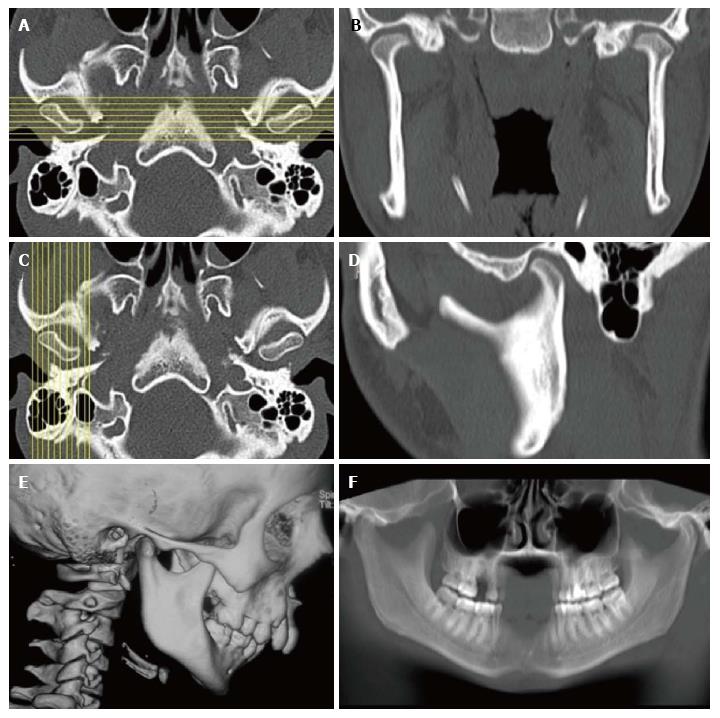
The patient lies supine on the CT table and is instructed not to move or swallow during the scanning process. The scan should start at the level of inferior orbital margin and end at the level of tip of the chin. The scan area must include the external auditory canals. Slice thickness and slice interval for acquisition should be 0.5-1 mm. Sagittal images are reconstructed from the raw data perpendicular to the plane of mandibular condyles as seen on axial plane, and coronal images are reconstructed parallel to the condyles as seen on axial plane (Figure 1), with a slice thickness and inter-slice gap of 2-3 mm[5].
The term “Temporomandibular disorders” encompasses a variety of lesions which involve the TMJ, muscles of mastication, and the adjacent musculoskeletal structures of the head and neck[6]. Most patients with Temporomandibular disorders are children and young adults (less than 20 years of age in our experience). The articular disc, the masticatory muscles and other soft tissues around the TMJ are best evaluated by MRI, and are beyond the scope of discussion of the present article. The other groups of disorders affect the glenoid fossa and the mandibular condyle and include a spectrum of congenital, traumatic, inflammatory and neoplastic diseases, and these are discussed in detail here.
Embryology: The TMJ develops between 7 and 11 wk of gestation. The mandibular condyle and the squamous temporal bone are formed by intramembranous ossification and the articular disc is formed by condensation of mesenchyme in the region of TMJ[7]. Hypoplastic mandibles are seen in Turner syndrome, hemifacial atrophy, and Silver Russell syndrome (a syndrome of intrauterine and post natal growth retardation, facial dysmorphism and clinodactyly) and whereas hyperplastic mandibles are seen in Marfaan’s syndrome and Proteus syndrome (a syndrome characterized by highly variable, asymmetric overgrowth of tissues that may include macrodactyly, vertebral anomalies, connective tissue nevi and vascular malformations).
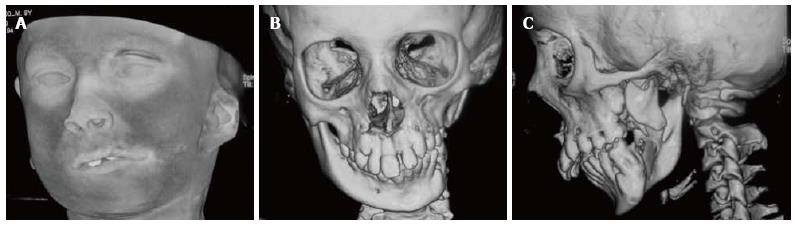
Hemifacial Microsomia (Goldenhaar syndrome-Oculo-Auriculo-Vertebral syndrome): Hemifacial microsomia is a developmental anomaly that affects 1 in every 5600 live births[8]. It is the second most common developmental anomaly of the face and cranium after cleft lip and cleft palate[8]. It arises due to aberrant development of the first branchial membrane and the first and second branchial arches. Abnormal development of the mandible, nose, ear, lip and soft palate are the hallmarks of this condition (Figure 2); associated anomalies include upper limb defects, tetralogy of Fallot, CNS malformations, renal agenesis or malposition, and speech and hearing disorders[8,9]. Asymmetric development of the mandible is the sine qua non for the diagnosis of hemifacial microsomia Association with chromosomal anomalies as deletions of 5p, 6q, duplications of 22q, and trisomies 7, 9, 18, 22, and maternal use of drugs as thalidomide and retinoic acid have been described[8,9].
An accurate pre-operative assessment of the mandible is mandatory for good surgical outcomes and multi-detector computed tomography (MDCT) plays a valuable role here by depicting the anatomy of the mandible and the glenoid fossa in exquisite detail. The OMENS classification system (Orbital asymmetry, mandibular hypoplasia, ear deformity, nerve involvement, soft tissue abnormality)[10,11] is used to describe the mandible in patients with hemifacial microsomia-the degree of dysmorphism increases from grade 1 to grade 5. Grade 1 is a normally shaped but small mandible; Grade 2 is a small mandible with abnormal shape, with Grade 2A assigned to a condyle in normal position and Grade 2B assigned to an infero-medially and anteriorly displaced condyle; Grade 3 is complete aplasia of the ramus and condyle, glenoid fossa and TMJ.
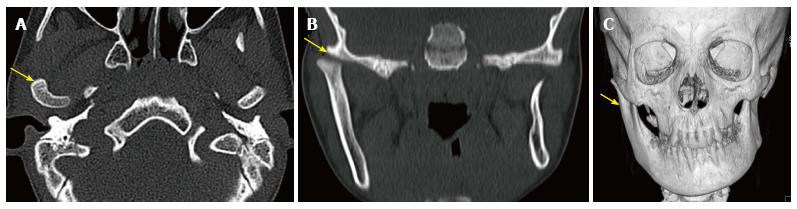
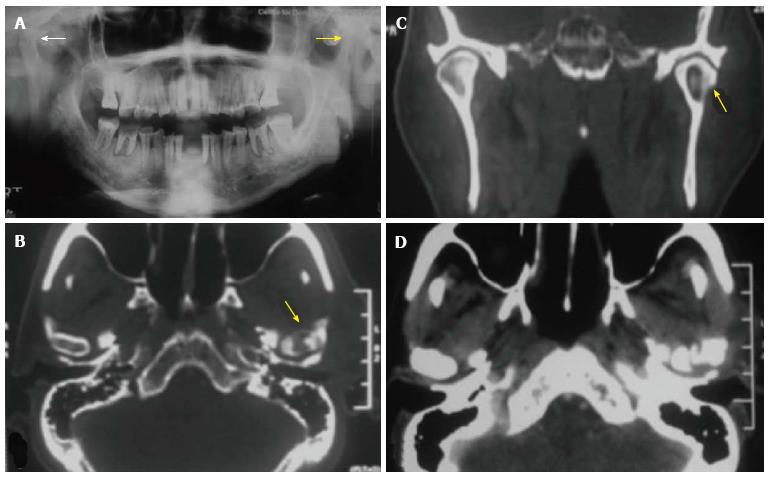
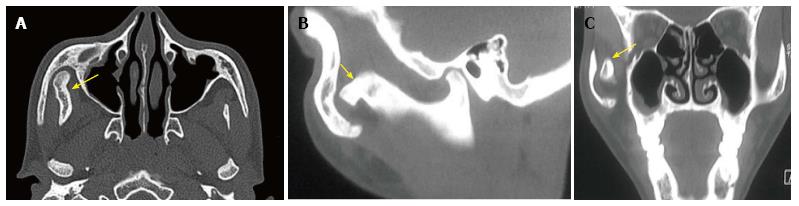
Non syndromic congenital mandibular hypoplasia: Mandibular hypoplasia is a common craniofacial anomaly and can be congenital, developmental, or acquired in origin, and may be unilateral or bilateral (Figure 3). Acquired causes of hypoplasia include oncologic defects, radiation damage, trauma, and hemifacial atrophy. Treatment consists of initial surgical moving of mandibular components into predetermined optimum followed by orthodontic treatment to correct dental malocclusion. MDCT provides the road map for surgical planning.
Condylar hyperplasia: Condylar hyperplasia is a disorder of uncertain etiology seen in patients between the ages of 11 and 30 years[12]. The mandibular condyle continues to grow relentlessly even though the normal growth period has ended (Figure 4). The condition can be treated by condylectomy during the period of active growth; and surgical mandibular repositioning for persisting symptoms after growth has stopped. MDCT defines the size of the condyle, and its relationship to adjacent structures.
Osteochondroma may cause similar symptoms and signs as condylar hyperplasia and must be distinguished. Osteochondromas are seen as localized to a part of the condyle on CT, whereas diffuse enlargement of the condyle is seen in condylar hyperplasia.
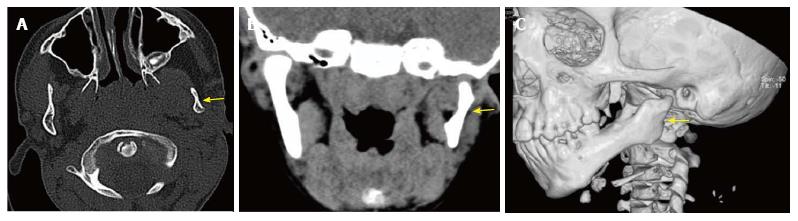
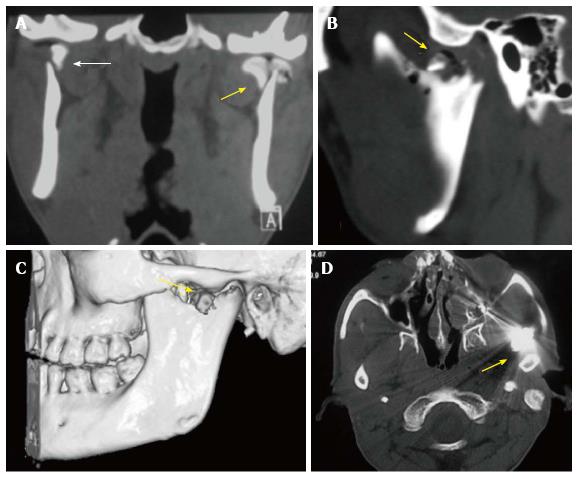
MDCT with axial and coronal reformatted images is the modality of choice for evaluation of acute trauma to TMJ[3,13]. The temporomandibular joints, the mandible, the maxilla, and the paranasal sinuses can be evaluated in a single scan. The Strasbourg Osteosynthesis Research Group classification defines 3 main types of condylar fractures: diacapitular fracture through the condylar head (DF), fracture of the neck of the condyle, and fracture of the base of the condyle (CBF)[14]. Fractures of the condylar head are further classified as-extracapsular or intracapsular; undisplaced or displaced (Figure 5). On imaging, the radiologist should describe the type of fracture, relationship of the fractured fragment to the mandible as well as glenoid fossa, angulation, presence of vertical compression, and damage to the soft tissues, i.e., the articular disc and the joint capsule.
Condylar fractures lead to anterior and medial displacement of the condylar process due to unbalanced action of the lateral pterygoid muscle which inserts into the condylar process, articular disc and capsule of TM joint. On clinical examination, the mandible is seen deviated towards the side of fracture with anterior open bite and malocclusion. If a condylar fracture is diagnosed, one must carefully look for associated fractures of skull base that can lead to CSF otorrhea and complications as meningitis.
Most of the fractures of condylar head are managed by closed reduction. The indications for open reduction are: displacement of the condyle into the external auditory canal or middle cranial fossa, lateral displacement of the condyle, inability to occlude, open wound with gross contamination or foreign body within the joint[14,15].
The most common arthritides affecting the TMJ are degenerative and traumatic arthritis; rheumatoid, metabolic, infectious arthritis, and spondyloarthropathies are less seen frequently[3,16,17]. Degenerative arthritis is secondary to internal derangement of the joint due to articular disc abnormalities. Arthritis after trauma is seen in untreated, ignored fractures of the condyle and these frequently progress to ankylosis.
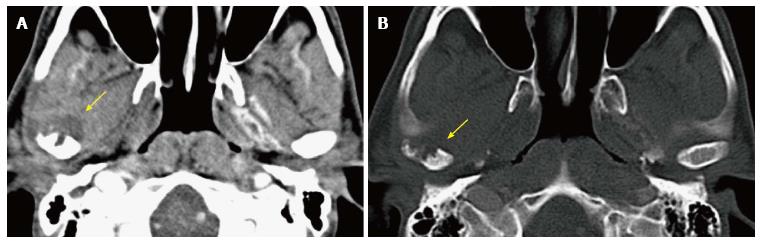
Infective arthritis is seen secondary to other infections of the head and neck (Figure 6). Patients present with an acutely painful and swollen joint with malaise, and CT reveals erosions of the articular surface of condyle and/or glenoid fossa, and inflammatory changes in surrounding muscles. Rarely, a sequestrum may form within the joint (Figure 7). If untreated, it may progress to fibrous or bony ankylosis.
Rheumatoid involvement of the TMJ is characterized by synovial proliferation and secondary erosive changes of the bone, with destruction of the condyle and articular eminence[17]. Eventually, bony ankylosis ensues with destruction of the intervening soft-tissue structures.
The term “ankylosis” is defined as joint fixation or fusion leading to chronic, painless restriction of joint movements. It may also cause facial asymmetry and deviation. Trauma and infection are the most common causes of TMJ ankylosis[18]. The initial traumatic insult may not be apparent and intra-articular hematoma leads to scarring and excessive bone formation, eventually causing fusion of the joint. TM joint infection is mostly due to contiguous spread from otitis media and mastoiditis, hematogenous spread is less common. Other rare causes include inflammatory arthritis (juvenile rheumatoid arthritis[19], psoriatic arthritis[20], ankylosing spondylitis[21]), or iatrogenic after surgery.
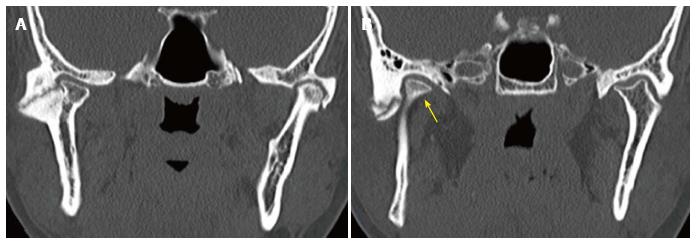
TMJ ankylosis can be classified into two categories: type I, medially angulated condyle with deformed articular fossa and a mild-to-moderate amount of new bone formation; and type II, no recognizable condyle or fossa but instead a large mass of new bone[22]. Type I is etiology-specific and seen after antecedent trauma. TMJ ankylosis is surgically treated by excision of the ankylosis, with or without autogenic, allogeneic or alloplastic graft replacement. MDCT provides a detailed three-dimensional image of the condylar mass and its relationship to adjacent structures of the skull base, which is essential for surgical planning (Figure 8).
Neoplastic lesions rarely involve the TMJ. Osteochondroma, osteoma, eosinophilic granuloma, chondrosarcoma and bone cysts have been described in the literature[3,23]. Synovial chondromatosis, pigmented villonodular synovitis (PVNS), pseudogout, fibrous dysplasia, hyperparathyroidism and giant cell reparative granuloma are some tumor like conditions which may involve the TMJ[23]. Contiguous tumors of external ear and parotid, and metastases from carcinoma breast, kidney, lung, colon and rectum and lymphoma may also involve TMJ[3].
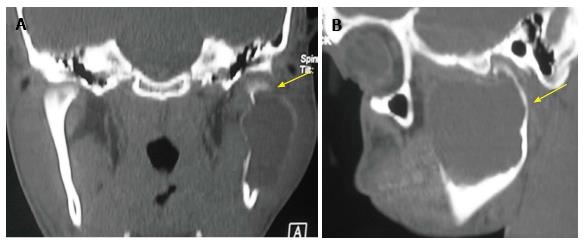
Of the above tumors, osteochondroma of the mandible deserves a special mention (Figure 9). It is an indolent tumor that is seen at the condyle or the coronoid process tip. It may become large enough to present as a facial mass or it may cause trismus. An MRI should be performed if there is a rapid change in the size of mass or pain develops in a previously asymptomatic mass. A cartilaginous cap that exceeds 2 cm in thickness on MRI is suspicious for a malignant transformation to chondrosarcoma, although such a transformation is quite rare.
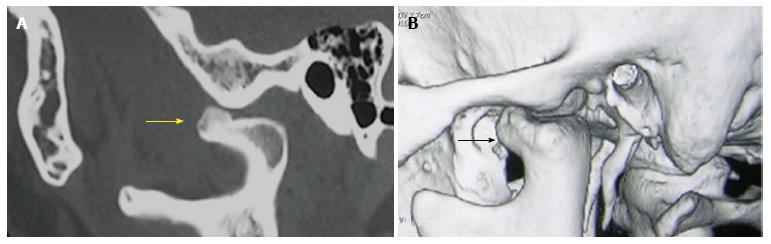
Jacob’s disease (first described by Jacob in 1899), is a rare entity in which a pseudo-joint develops between a sessile coronoid process osteochondroma or a hyperplastic coronoid process, and the zygomatic process of maxilla causing severe restriction of jaw movement[24]. The length of the coronoid processes can be accurately measured on MDCT and changes in the zygomatic arch are also well depicted (Figure 10).
Aneurysmal bone cyst of the TMJ is another uncommon, tumor-like non-neoplastic affliction of the Temporomandibular joint (Figure 11). It usually affects children and young adults less than 20 years of age. The patients present with slowly increasing swelling in the cheek and preauricular region. The lesion may be unilocular or multilocular on imaging and has a non-specific imaging appearance. It is characterized by presence of well defined blood spaces lined by endothelium on histology. MDCT evaluates the lesion and defines its extent of (involvement of condyle, mandibular ramus, temporal bone, presence of breach of cortex) and is necessary for deciding surgical management (curettage vs block resection).
Trauma, internal derangement with possible sequelae (osteoarthritis), and inflammation are the most common of pathologic conditions involving the TMJ. MDCT enables comprehensive evaluation of osseous afflictions of TM joint, and is a valuable tool for surgical planning.
P- Reviewer: Ramirez Aristeguieta LM, Rothschild BM S- Editor: Song XX L- Editor: A E- Editor: Lu YJ
| 1. | Giannakopoulos HE, Quinn PD, Granquist E, Chou JC. Posttraumatic temporomandibular joint disorders. Craniomaxillofac Trauma Reconstr. 2009;2:91-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Piette E. Anatomy of the human temporomandibular joint. An updated comprehensive review. Acta Stomatol Belg. 1993;90:103-127. [PubMed] |
| 3. | Som PM, Curtin HD. Head and Neck Imaging. 4th ed. St Louis: Mosby 2003; . |
| 4. | Tomas X, Pomes J, Berenguer J, Quinto L, Nicolau C, Mercader JM, Castro V. MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics. 2006;26:765-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 5. | Walter E, Hüls A, Schmelzle R, Klose U, Küper K, Kalender WA. CT and MR imaging of the temporomandibular joint. Radiographics. 1988;8:327-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Scrivani SJ, Keith DA, Kaban LB. Temporomandibular disorders. N Engl J Med. 2008;359:2693-2705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 450] [Article Influence: 26.5] [Reference Citation Analysis (0)] |
| 7. | Mérida-Velasco JR, Rodríguez-Vázquez JF, Mérida-Velasco JA, Sánchez-Montesinos I, Espín-Ferra J, Jiménez-Collado J. Development of the human temporomandibular joint. Anat Rec. 1999;255:20-33. [PubMed] |
| 8. | Sze RW, Paladin AM, Lee S, Cunningham ML. Hemifacial microsomia in pediatric patients: asymmetric abnormal development of the first and second branchial arches. AJR Am J Roentgenol. 2002;178:1523-1530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Pirttiniemi P, Peltomäki T, Müller L, Luder HU. Abnormal mandibular growth and the condylar cartilage. Eur J Orthod. 2009;31:1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 10. | Vento AR, LaBrie RA, Mulliken JB. The O.M.E.N.S. classification of hemifacial microsomia. Cleft Palate Craniofac J. 1991;28:68-76; discussion 77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Rahbar R, Robson CD, Mulliken JB, Schwartz L, Dicanzio J, Kenna MA, McGill TJ, Healy GB. Craniofacial, temporal bone, and audiologic abnormalities in the spectrum of hemifacial microsomia. Arch Otolaryngol Head Neck Surg. 2001;127:265-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Nah KS. Hyperplastic conditions of the mandibular condyles. Korean J Oral Maxillofac Radiol. 2003;33:207-209. |
| 13. | Huang G, Zheng J, Zhang S, Yang C. [The value of panoramic radiograph, CT and MRI for the diagnosis of condylar fracture]. Zhonghua Kouqiangyixue Zazhi. 2014;49:434-439. [PubMed] |
| 14. | Cenzi R, Burlini D, Arduin L, Zollino I, Guidi R, Carinci F. Mandibular condyle fractures: evaluation of the Strasbourg Osteosynthesis Research Group classification. J Craniofac Surg. 2009;20:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Eckelt U, Schneider M, Erasmus F, Gerlach KL, Kuhlisch E, Loukota R, Rasse M, Schubert J, Terheyden H. Open versus closed treatment of fractures of the mandibular condylar process-a prospective randomized multi-centre study. J Craniomaxillofac Surg. 2006;34:306-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 229] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 16. | Scutellari PN, Orzincolo C, Ceruti S. [The temporo-mandibular joint in pathologic conditions: rheumatoid arthritis and seronegative spondyloarthritis]. Radiol Med. 1993;86:456-466. [PubMed] |
| 17. | Atsü SS, Ayhan-Ardic F. Temporomandibular disorders seen in rheumatology practices: A review. Rheumatol Int. 2006;26:781-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Rowe NL. Ankylosis of the temporomandibular joint. Part 3. J R Coll Surg Edinb. 1982;27:209-218. [PubMed] |
| 19. | Fanaras N, Parry NS, Matthews NS. Multidisciplinary approach in the management of absolute trismus with bilateral temporomandibular joint replacements for a patient with juvenile idiopathic arthritis. J Oral Maxillofac Surg. 2014;72:2262-2272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Koorbusch GF, Zeitler DL, Fotos PG, Doss JB. Psoriatic arthritis of the temporomandibular joints with ankylosis. Literature review and case reports. Oral Surg Oral Med Oral Pathol. 1991;71:267-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Li JM, Zhang XW, Zhang Y, Li YH, An JG, Xiao E, Yan YB. Ankylosing spondylitis associated with bilateral ankylosis of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e478-e484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Aggarwal S, Mukhopadhyay S, Berry M, Bhargava S. Bony ankylosis of the temporomandibular joint: a computed tomography study. Oral Surg Oral Med Oral Pathol. 1990;69:128-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Mostafapour SP, Futran ND. Tumors and tumorous masses presenting as temporomandibular joint syndrome. Otolaryngol Head Neck Surg. 2000;123:459-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 45] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Akan H, Mehreliyeva N. The value of three-dimensional computed tomography in diagnosis and management of Jacob’s disease. Dentomaxillofac Radiol. 2006;35:55-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |