Published online Apr 16, 2015. doi: 10.12998/wjcc.v3.i4.353
Peer-review started: July 8, 2014
First decision: August 14, 2014
Revised: November 24, 2014
Accepted: February 9, 2015
Article in press: February 11, 2015
Published online: April 16, 2015
Processing time: 280 Days and 1.4 Hours
AIM: To investigate whether endoscopic papillary large balloon dilation (EPLBD) can be safety and effectively performed in patients aged ≥ 80 years.
METHODS: Lithotomy by EPLBD was conducted in 106 patients with bile duct stones ≥ 13 mm in size or with three or more bile duct stones ≥ 10 mm. The patients were divided into group A (< 80 years) and group B (≥ 80 years). Procedure success rate, number of endoscopic retrograde cholangiopancreatographies (ERCP), and incidence of complications were examined in both groups.
RESULTS: Group B tended to include significantly more patients with peripapillary diverticulum, hypertension, hyperlipemia, cerebrovascular disease/dementia, respiratory disease/cardiac disease, and patients administered an anticoagulant or antiplatelet agent (P < 0.05). The success rate of the initial lithotomy was 88.7 (94/106)%. The final lithotomy rate was 100 (106/106)%. Complications due to treatment procedure occurred in 4.72 (5/106)% of the patients. There was no significant difference in procedure success rate, number of ERCP, or incidence of complications between group A and group B.
CONCLUSION: EPLBD can be safely performed in elderly patients, the same as in younger patients.
Core tip: Endoscopic treatment by papillary large balloon dilation for large stones can be safely performed in elderly patients, the same as in younger patients.
- Citation: Sakai Y, Tsuyuguchi T, Sugiyama H, Sasaki R, Sakamoto D, Nakamura M, Watanabe Y, Nishikawa T, Yasui S, Mikata R, Yokosuka O. Endoscopic papillary large balloon dilation for bile duct stones in elderly patients. World J Clin Cases 2015; 3(4): 353-359
- URL: https://www.wjgnet.com/2307-8960/full/v3/i4/353.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i4.353
The number of elderly patients with common bile duct stones has been increasing associated with the global prolongation of life expectancy[1]. Endoscopic retrograde cholangiopancreatography (ERCP) has been recognized as a treatment with less risk and lower mortality than surgery[2]. Endoscopic treatment for choledocholithiasis should be attempted as the first choice of treatment because of its high success rate in addition to its low invasiveness and low incidence of complications[3]. Although a report indicated that ERCP related procedures may be hazardous for patients with common bile duct stones as well as in elderly patients aged ≥ 80 years[4], it is often reported that this procedure can be useful and safely performed even in elderly patients[5-20]. The usefulness of endoscopic treatment using endoscopic papillary large balloon dilation (EPLBD) which is a new papillary treatment using a balloon of large diameter for large bile duct stones or multiple bile duct stones has been recently reported. Most of the reports described the procedure as safe and useful[20-34]. However, there have been some cases of death[35]. Since elderly patients often have an underlying disease, they may follow a fatal course, thus they require special attention[4]. There are few reports on the usefulness of this procedure in elderly patients[20], and it has not been examined sufficiently. This report examined usefulness of EPLBD in patients aged ≥ 80 years.
The study involved 106 patients (A) with bile duct stones ≥ 13 mm in their short diameter, or (B) multiple (≥ 3) bile duct stones with the smallest more than 10 mm in the shortest diameter, but without confluence stones. These patients were selected from among those with bile duct stones visiting our hospital or our affiliated hospitals from November 2009 to June 2014. Inclusion criteria were patients who could undergo endoscopic sphincterotomy (EST), and who gave their informed consent to the procedure. Exclusion criteria were coagulopathy (international normalized ratio > 1.5), marked thrombocytopenia (platelet count < 50000/mL), patients who could not discontinue the administration of an anticoagulant or antiplatelet agent, patients for whom endoscopic biliary drainage was difficult (Billroth-II or Roux-en-Y), patients with the papilla within the diverticulum, patients with stenosis of the intrapancreatic bile duct, stone diameter > 30 mm (shortest diameter), and patients who do not give their informed consent.
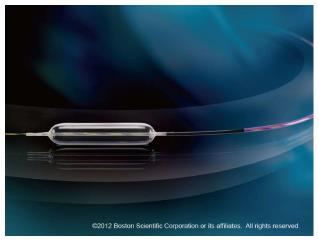
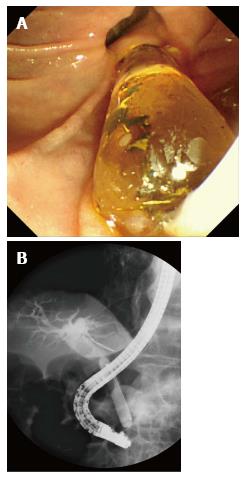
We selected 79 patients with new bile duct stones and 27 with recurrent stones. All cases of recurrent stones were those after EST. We performed EST in 65 patients and it had been already performed in 41 patients. Fourteen patients whose stones were not recurrent and EST had been already performed were difficult cases referred to our hospital for a lithotomy. The average diameter of the stones was 14.29 (10-28) mm, the number of stones was 5.73 (1-30) and the diameter of the bile duct was 16.97 (10-28) mm. As for the gall bladder, 77 patients were calculous, one was acalculous and 28 had undergone cholecystectomy. Parapapillary diverticulum was noted in 50 patients. The patients were divided into group A (< 80 years) and group B (≥ 80 years). The clinical background of patients in these 2 groups is shown in Table 1. Patients in group B tended to have significantly more frequently peripapillary diverticulum, hypertension, hyperlipemia, cerebrovascular disease/dementia, respiratory/cardiac disease, or were taking an anticoagulant or antiplatelet agent. There was no significant difference in other factors between group A and group B. One session of treatment lasted up to 60 min after inserting the endoscope. The condition of the patients was observed, and if the patient showed much discomfort, the procedure was completed after inserting the drainage, even while in the process of treatment. Before ERCP, all patients were given a standard premedication consisting of intravenous administration of midazolam (3 to 10 mg), and the dose depended on age and tolerance. Scopolamine butylbromide or glucagon was used for duodenal relaxation. During ERCP, arterial oxygen saturation was continuously monitored using a pulse oximeter. Patients were kept fasting after the procedure for at least 24 h with drip infusion of 2000 mL and remained hospitalized for at least 72 h. For cannulation, catheters PR-104Q, R110Q-1 and PR233Q were used. A 0.025-inch or 0.035-inch guidewire (Jagwire: Microvasive, Boston Scientific Corp., Natick, MA; Revo Wave: PIOLAX, or VisiGlide: Olympus Corp.) was used. The endoscopes used were JF240, JF260V, TJF260V (Olympus Corp.), backward side-viewing endoscope, for patients with no history of gastric resection and patients of Billroth-I. After cholangiography, a guidewire was placed in the bile duct to conduct EST. Clever-Cut3V (Olympus Corp.) was used as the knife for EST. EST was conducted using a single electrosurgical current generator (PSD-20, Olympus Corp.) at a power of 25 watts. For those in which an incision had been already made, a guidewire was placed in the bile duct after cholangiography to perform EPLBD. In performing EPLBD, CRE 12-20 mm (Fixed wire type 8 cm or Wire-guided type 5.5 cm: Boston Scientific Corp.) was used depending on the diameter of the bile duct (Figure 1). For balloon dilation, a contrast agent mixed with saline solution at a volume ratio of 1:1 was used to slowly inflate it. Inflation was performed until the notch on the balloon disappeared (Figure 2). However, regardless of the disappearance of the notch, balloon dilation was completed when the papilla was dilated enough for stone removal. The balloon was dilated in a position where it was possible to confirm the tip of the balloon in the papillary side on the endoscopic image, and the position was maintained. After the notch on the balloon disappeared, the balloon was promptly deflated. When we considered it necessary to perform lithotripsy of the stone, we did it without hesitation. The basket catheter used for lithotripsy was LBGT-7245S (ZEON Medical) or BML-V237QR-30 (Olympus Corp.). Peroral cholangioscopy (POCSL) was performed by mother-baby system using CHF-B260 (Olympus Corp.) as the cholangioscope and Autholith (Northgate) as the electrohydraulic lithotripsy probe. The basket catheter used for collecting stones was FG-22Q or FG-V416Q (Olympus Corp.), LBGT-7245S (ZEON Medical) or BML-V237QR-30 (Olympus Corp.) The balloon catheter used was EXP718200 (ZEON Medical) or FS-QEB-XL-B (COOK). No drainage tube was inserted when lithotomy was successful, while it was inserted when we thought a stone still remained.
| < 80 yr old (Group A) | ≥80 yr old (Group B) | P-value | |
| Number of patients | 59 | 47 | |
| Male | 36 | 20 | NS |
| Female | 23 | 27 | NS |
| Choledocholith | |||
| Number of stones | 5.24 ± 5.52 (1-30) | 6.44 ± 6.98 (1-25) | NS |
| Stone diameter (mm) | 14.03 ± 3.00 (10-28) | 14.52 ± 4.48 (10-25) | NS |
| Common bile duct diameter (mm) | 16.62 ± 3.52 (10-28) | 17.44 ± 3.93 (10-25) | NS |
| Gallbladder | |||
| Calculous | 43 | 34 | NS |
| Acalculous | 0 | 1 | NS |
| Cholecystectomy | 15 | 13 | NS |
| Primary case | 43 | 36 | NS |
| Recurrence | 17 | 10 | NS |
| Endoscopic sphincterotomy | 36 | 29 | NS |
| Post endoscopic sphincterotomy | 23 | 18 | NS |
| Diverticulum | 15 | 35 | < 0.05 |
| Hypertension | 23 | 37 | < 0.05 |
| Hyperlipidemia | 9 | 21 | < 0.05 |
| Diabetes mellitus | 10 | 8 | NS |
| Chronic respiratory disease | 0 | 5 | < 0.05 |
| Cardiac disease | 8 | 18 | < 0.05 |
| Chronic liver disease | 1 | 0 | NS |
| Chronic kidney disease | 2 | 3 | < 0.05 |
| Anticoagulant/antiplatelet | 9 | 23 | < 0.05 |
Iatrogenic morbidity was assessed according to the criteria of Cotton et al[36]. The observation period was 30 d after the procedure and any coincidental event noted during the period was considered as an early coincidental event. All the treatment procedures were performed after obtaining the informed consent from the patients in writing. This study was conducted after the study protocol was approved by the ethics committee of Chiba University.
Pearson χ2 test with Yates correction and Fisher’s exact test, when appropriate, were used for statistical analysis of categorical variables. Data were analyzed using SPSS software version 11 (SPSS, Chicago, IL). Differences with a P value of < 0.05 were considered statistically significant.
The success rate of lithotomy in the initial treatment was 88.7 (94/106)%. The final lithotomy rate was 100 (106/106)%. The time necessary to perform lithotomy was 39.4 (10-128) min and the mean treatment frequency was 1.21 (1-4) times. Lithotripsy was needed in 11.3 (12/106)% of the patients. Among the patients requiring lithotripsy, 6 had a highly tortuous bile duct and 6 had significantly large bile duct stones. For lithotripsy, endoscopic mechanical lithotripsy was performed in 10 patients and POCSL in 2. Complications due to the treatment procedure were observed in 4.7 (5/106)% of the patients, including bleeding in 1.9 (2/106)%, perforation in 0.9 (1/106)%, pneumonia in 0.9 (1/106)%, and acute cholangitis in 0.9 (1/106)%. Patients were classified into group A or group B for the analysis of data (Tables 2 and 3). The lithotomy success rate was 88.1 (52/59)% in group A, and 89.4 (42/47)% in group B and that for final lithotomy was 100%, both in group A (59/59)% and in group B (47/47). The lithotripsy rate was 10.2 (6/59)% in group A, and 12.8 (6/47)% in group B. Operation time was 37.59 ± 26.94 (12-125) min in group A, and 42.02 ± 27.12 (10-128) min in group B. The number of ERCP was 1.24 ± 0.683 (1-4) in group A, and 1.17 ± 0.529 (1-4) in group B. The incidence of complications was 6.8 (4/59)% in group A and 2.1 (1/47)% in group B, and there was no significant difference between group A and group B, regarding other parameters.
| ERCP procedures | < 80 yr old (Group A; n = 59) | ≥80 yr old (Group B; n = 47) | P-value |
| Lithotomy success rate | |||
| Initial | 52 (88.1%) | 42 (89.4%) | NS |
| Final | 59 (100%) | 47 (100%) | NS |
| Lithotripsy | 6 (10.2%) | 6 (12.8%) | NS |
| Procedure time: min | 37.59 ± 26.94 (12-125) | 42.02 ± 27.12 (10-128) | NS |
| Number of ERCP | 1.24 ± 0.683 (1-4) | 1.17 ± 0.529 (1-4) | NS |
| Related complications | < 80 yr old (Group A; n = 59) | ≥80 yr old (Group B; n = 47) | P-value |
| Pancreatitis | 0 | 0 | |
| Perforation | 1 (mild) | 0 | NS |
| Bleeding | 2 (mild) | 0 | NS |
| Cholangitis | 0 | 1 (mild) | NS |
| Cholecystitis | 0 | 0 | |
| Others | 1 | 0 | NS |
| Total | 4 | 1 | NS |
This study showed that elderly patients aged ≥ 80 years often have underlying diseases, however, results of treatment for large bile duct stones or multiple bile duct stones using EPLBD lithotomy were equivalent to those aged < 80 years in terms of success rate, lithotripsy rate, procedure time, number of ERCP, and complications caused by the procedure. EPLBD is the endoscopic treatment for bile duct stones reported by Ersoz et al[21] in 2003. Recently, the reports on the results of treatment for choledocholithiasis using EPLBD have been increasing[20-35]. Ordinary endoscopic papillary balloon dilation (EPBD) employs a balloon 4-10 mm in diameter for papillary dilation, whereas EPLBD is performed using a balloon 12-20 mm in diameter. Before this procedure was reported, lithotomy of large bile duct stones or multiple bile duct stones was difficult without lithotripsy of the stone. This procedure has the advantage that compared with EPBD or EST a larger papillary aperture can be obtained. It is reported in randomized controlled trials and meta-analyses that the larger papillary aperture enables easy insertion of the device as well as lithotomy of stones the same size as that of the dilated balloon without lithotripsy of the stones in many patients[34,37,38], which may be advantageous because the duration of the procedure would be shortened[26]. In this study many patients were cured after one session of treatment. There are many reports describing that in the nature of things, elderly patients have many underlying diseases, whereas the comparison of patients aged 80 years or greater with those aged less than 80 years showed the similar tendency[11,19]. Shorter treatment time is naturally an advantage even in young patients, and this study confirmed that a shorter treatment time was desirable for elderly patients because many of them have underlying diseases such as respiratory disease. Shorter treatment time is beneficial for elderly patients. There was no difference in the success rate of the procedure itself, however, many patients aged ≥ 80 years have peripapillary diverticulum according to a past report[19], and this study also showed elderly patients tended to develop it, thus when performing the procedure, it may be necessary to pay attention to perforation. The presence of peripapillary diverticulum may cause deviation of the course of the bile duct leading to difficulty in cannulation[39]. However, this study revealed that there was no difference in the success rate of the procedure between the two groups. The reason may be due to recent advancement of the endoscope and its related treatment instruments. In this study, EPLBD was performed after EST. There are past reports describing that it is possible to safely perform EPLBD without performing EST[35]. According to this study many elderly patients not only have peripapillary diverticulum but also are taking an anticoagulant or antiplatelet agent, thus if it were possible to safely perform EPLBD without performing EST, the procedure time would be shortened even further and the risk of perforation or bleeding would also be reduced.
Although a shorter procedure time and success of the procedure are very important for elderly patients, a low rate of complications derived from the procedure is also required. Past reports showed that complications caused by this procedure occurred at a low rate[20-35]. In the present study, complications occurred at a low rate and there was no difference between the two groups, suggesting it is possible to safely perform EPLBD even in elderly patients. The most problematic complications among ERCP related procedures is pancreatitis. Although it is reported that pancreatitis is less likely to occur in elderly patients because of their reduced pancreatic function[40], this study revealed there were no such results at all, suggesting that safety of the procedure is not only ensured for elderly patients but also that of the procedure itself is ensured. Reports describing usefulness and safety of EPLBD in elderly patients are currently limited to retrospective studies, thus a prospective study is necessary to confirm our findings.
EPLBD can be safely performed in elderly patients the same as in younger patients.
The usefulness of endoscopic treatment using endoscopic papillary large balloon dilation (EPLBD), which is a new papillary treatment using a large diameter balloon for large bile duct stones or multiple bile duct stones has been recently reported. Most of the reports have described this procedure is safe and useful. However, there are some cases of death. Since elderly patients are often complicated with underlying diseases, they may follow a fatal course after EPLBD, thus they require special attention. There are only a few reports on the usefulness of this procedure in elderly patients, and sufficient examination has not been conducted. This report examined the usefulness of EPLBD in patients aged ≥ 80 years.
The results of EPLBD in patients with bile duct stones ≥ 13 mm in their short diameter or patients with three or more bile duct stones ≥ 10 mm in their short diameter were examined.
EPLBD for bile duct stones was reported by Ersoz et al in 2003. Recently, its indication has widened. The reports describing the usefulness and safety of EPLBD in elderly patients are currently limited to retrospective studies. A prospective study is necessary to confirm our findings.
In patients with large common bile duct stones, endoscopic sphincterotomy (EST) + EPLBD is a good alternative to conventional EST. Before this procedure was reported, lithotomy of large stones or multiple stones was difficult without lithotripsy of the stones. Endoscopic treatment by papillary large balloon dilation can be safely performed in elderly patients the same as in younger patients.
Treatment by EPLBD, which is lithotomy without lithotripsy for large stones by dilating the papilla using a large balloon, after performing EST has been reported. Endoscopic treatment by papillary large balloon dilation can be safely performed in elderly patients the same as in younger patients.
This is a retrospective study evaluating whether EPLBD can be safely and effectively performed in elderly patients. This study may be of interest to the readers.
P- Reviewer: Harada R S- Editor: Gong XM L- Editor: A E- Editor: Lu YJ
| 1. | Hacker KA, Schultz CC, Helling TS. Choledochotomy for calculous disease in the elderly. Am J Surg. 1990;160:610-612; discussion 613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Siegel JH, Kasmin FE. Biliary tract diseases in the elderly: management and outcomes. Gut. 1997;41:433-435. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 105] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 3. | Sakai Y, Tsuyuguchi T, Sugiyama H, Nishikawa T, Tawada K, Saito M, Kurosawa J, Mikata R, Tada M, Ishihara T. Current situation of endoscopic treatment for common bile duct stones. Hepatogastroenterology. 2012;59:1712-1716. [PubMed] |
| 4. | Deenitchin GP, Konomi H, Kimura H, Ogawa Y, Naritomi G, Chijiiwa K, Tanaka M, Ikeda S. Reappraisal of safety of endoscopic sphincterotomy for common bile duct stones in the elderly. Am J Surg. 1995;170:51-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Ito Y, Tsujino T, Togawa O, Yamamoto N, Isayama H, Nakata R, Kawabe T, Omata M. Endoscopic papillary balloon dilation for the management of bile duct stones in patients 85 years of age and older. Gastrointest Endosc. 2008;68:477-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Sugiyama M, Atomi Y. Endoscopic sphincterotomy for bile duct stones in patients 90 years of age and older. Gastrointest Endosc. 2000;52:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 81] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Katsinelos P, Paroutoglou G, Kountouras J, Zavos C, Beltsis A, Tzovaras G. Efficacy and safety of therapeutic ERCP in patients 90 years of age and older. Gastrointest Endosc. 2006;63:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 89] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Fritz E, Kirchgatterer A, Hubner D, Aschl G, Hinterreiter M, Stadler B, Knoflach P. ERCP is safe and effective in patients 80 years of age and older compared with younger patients. Gastrointest Endosc. 2006;64:899-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Mitchell RM, O’Connor F, Dickey W. Endoscopic retrograde cholangiopancreatography is safe and effective in patients 90 years of age and older. J Clin Gastroenterol. 2003;36:72-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 10. | Rodríguez-González FJ, Naranjo-Rodríguez A, Mata-Tapia I, Chicano-Gallardo M, Puente-Gutierrez JJ, López-Vallejos P, Hervás-Molina AJ, de Dios-Vega JF. ERCP in patients 90 years of age and older. Gastrointest Endosc. 2003;58:220-225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Obana T, Fujita N, Noda Y, Kobayashi G, Ito K, Horaguchi J, Koshita S, Kanno Y, Yamashita Y, Kato Y. Efficacy and safety of therapeutic ERCP for the elderly with choledocholithiasis: comparison with younger patients. Intern Med. 2010;49:1935-1941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 12. | Tsujino T, Yoshida H, Isayama H, Ito Y, Yashima Y, Yagioka H, Kogure H, Sasaki T, Arizumi T, Togawa O. Endoscopic papillary balloon dilation for bile duct stone removal in patients 60 years old or younger. J Gastroenterol. 2010;45:1072-1079. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 13. | Ashton CE, McNabb WR, Wilkinson ML, Lewis RR. Endoscopic retrograde cholangiopancreatography in elderly patients. Age Ageing. 1998;27:683-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Mohammad Alizadeh AH, Afzali ES, Shahnazi A, Sanati A, Mirsattari D, Zali MR. Utility and safety of ERCP in the elderly: a comparative study in iran. Diagn Ther Endosc. 2012;2012:439320. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Clarke GA, Jacobson BC, Hammett RJ, Carr-Locke DL. The indications, utilization and safety of gastrointestinal endoscopy in an extremely elderly patient cohort. Endoscopy. 2001;33:580-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 105] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | MacMahon M, Walsh TN, Brennan P, Osborne H, Courtney MG. Endoscopic retrograde cholangiopancreatography in the elderly: a single unit audit. Gerontology. 1993;39:28-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Köklü S, Parlak E, Yüksel O, Sahin B. Endoscopic retrograde cholangiopancreatography in the elderly: a prospective and comparative study. Age Ageing. 2005;34:572-577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 30] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Deans GT, Sedman P, Martin DF, Royston CM, Leow CK, Thomas WE, Brough WA. Are complications of endoscopic sphincterotomy age related? Gut. 1997;41:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Sakai Y, Tsuyuguchi T, Hirata N, Nakaji S, Shimura K, Fujimoto T, Tsuchiya S, Nishino T, Nishikawa T, Sugiyama H. Can endoscopic sphincterotomy be performed safely in elderly patients aged 80 years or older with pancreatic and biliary diseases? Hepatogastroenterology. 2013;60:1251-1256. [PubMed] |
| 20. | Tonozuka R, Itoi T, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Umeda J. Efficacy and safety of endoscopic papillary large balloon dilation for large bile duct stones in elderly patients. Dig Dis Sci. 2014;59:2299-2307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Ersoz G, Tekesin O, Ozutemiz AO, Gunsar F. Biliary sphincterotomy plus dilation with a large balloon for bile duct stones that are difficult to extract. Gastrointest Endosc. 2003;57:156-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 256] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 22. | Minami A, Hirose S, Nomoto T, Hayakawa S. Small sphincterotomy combined with papillary dilation with large balloon permits retrieval of large stones without mechanical lithotripsy. World J Gastroenterol. 2007;13:2179-2182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 111] [Cited by in RCA: 109] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 23. | Maydeo A, Bhandari S. Balloon sphincteroplasty for removing difficult bile duct stones. Endoscopy. 2007;39:958-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 24. | Heo JH, Kang DH, Jung HJ, Kwon DS, An JK, Kim BS, Suh KD, Lee SY, Lee JH, Kim GH. Endoscopic sphincterotomy plus large-balloon dilation versus endoscopic sphincterotomy for removal of bile-duct stones. Gastrointest Endosc. 2007;66:720-726; quiz 768, 771. [PubMed] |
| 25. | Attasaranya S, Cheon YK, Vittal H, Howell DA, Wakelin DE, Cunningham JT, Ajmere N, Ste Marie RW, Bhattacharya K, Gupta K. Large-diameter biliary orifice balloon dilation to aid in endoscopic bile duct stone removal: a multicenter series. Gastrointest Endosc. 2008;67:1046-1052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 125] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 26. | Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic sphincterotomy combined with large balloon dilation can reduce the procedure time and fluoroscopy time for removal of large bile duct stones. Am J Gastroenterol. 2009;104:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 108] [Article Influence: 6.8] [Reference Citation Analysis (1)] |
| 27. | Kim KO, Kim TN, Lee SH. Endoscopic papillary large balloon dilation for the treatment of recurrent bile duct stones in patients with prior sphincterotomy. J Gastroenterol. 2010;45:1283-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 28. | Kurita A, Maguchi H, Takahashi K, Katanuma A, Osanai M. Large balloon dilation for the treatment of recurrent bile duct stones in patients with previous endoscopic sphincterotomy: preliminary results. Scand J Gastroenterol. 2010;45:1242-1247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Kim TH, Oh HJ, Lee JY, Sohn YW. Can a small endoscopic sphincterotomy plus a large-balloon dilation reduce the use of mechanical lithotripsy in patients with large bile duct stones? Surg Endosc. 2011;25:3330-3337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 30. | Stefanidis G, Viazis N, Pleskow D, Manolakopoulos S, Theocharis L, Christodoulou C, Kotsikoros N, Giannousis J, Sgouros S, Rodias M. Large balloon dilation vs. mechanical lithotripsy for the management of large bile duct stones: a prospective randomized study. Am J Gastroenterol. 2011;106:278-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 111] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 31. | Kim HW, Kang DH, Choi CW, Park JH, Lee JH, Kim MD, Kim ID, Yoon KT, Cho M, Jeon UB. Limited endoscopic sphincterotomy plus large balloon dilation for choledocholithiasis with periampullary diverticula. World J Gastroenterol. 2010;16:4335-4340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 31] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 32. | Itoi T, Ishii K, Itokawa F, Kurihara T, Sofuni A. Large balloon papillary dilation for removal of bile duct stones in patients who have undergone a billroth ii gastrectomy. Dig Endosc. 2010;22 Suppl 1:S98-S102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Sakai Y, Tsuyuguchi T, Sugiyama H, Nishikawa T, Kurosawa J, Saito M, Tawada K, Mikata R, Tada M, Ishihara T. Endoscopic sphincterotomy combined with large balloon dilation for removal of large bile duct stones. Hepatogastroenterology. 2013;60:58-64. [PubMed] |
| 34. | Teoh AY, Cheung FK, Hu B, Pan YM, Lai LH, Chiu PW, Wong SK, Chan FK, Lau JY. Randomized trial of endoscopic sphincterotomy with balloon dilation versus endoscopic sphincterotomy alone for removal of bile duct stones. Gastroenterology. 2013;144:341-345.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 35. | Park SJ, Kim JH, Hwang JC, Kim HG, Lee DH, Jeong S, Cha SW, Cho YD, Kim HJ, Kim JH. Factors predictive of adverse events following endoscopic papillary large balloon dilation: results from a multicenter series. Dig Dis Sci. 2013;58:1100-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 36. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1890] [Cited by in RCA: 2037] [Article Influence: 59.9] [Reference Citation Analysis (1)] |
| 37. | Feng Y, Zhu H, Chen X, Xu S, Cheng W, Ni J, Shi R. Comparison of endoscopic papillary large balloon dilation and endoscopic sphincterotomy for retrieval of choledocholithiasis: a meta-analysis of randomized controlled trials. J Gastroenterol. 2012;47:655-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 38. | Liu Y, Su P, Lin Y, Lin S, Xiao K, Chen P, An S, Bai Y, Zhi F. Endoscopic sphincterotomy plus balloon dilation versus endoscopic sphincterotomy for choledocholithiasis: A meta-analysis. J Gastroenterol Hepatol. 2013;28:937-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Zoepf T, Zoepf DS, Arnold JC, Benz C, Riemann JF. The relationship between juxtapapillary duodenal diverticula and disorders of the biliopancreatic system: analysis of 350 patients. Gastrointest Endosc. 2001;54:56-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 90] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Laugier R, Bernard JP, Berthezene P, Dupuy P. Changes in pancreatic exocrine secretion with age: pancreatic exocrine secretion does decrease in the elderly. Digestion. 1991;50:202-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 109] [Article Influence: 3.2] [Reference Citation Analysis (0)] |