Published online Mar 16, 2015. doi: 10.12998/wjcc.v3.i3.322
Peer-review started: September 18, 2014
First decision: October 14, 2014
Revised: December 25, 2014
Accepted: January 9, 2015
Article in press: January 12, 2015
Published online: March 16, 2015
Processing time: 177 Days and 16.7 Hours
Facial nerve schwannoma occurring within the parotid gland is a rare tumour. We report a case of schwannoma within the parotid gland in a young female patient, who underwent ultrasound and magnetic resonance imaging (MRI) and subsequent surgical excision of the lesion. The lesion showed hyperintensity on T2-weighted and diffusion-weighted MRI. There was no adjacent lymphadenopathy. Although hyperintensity on diffusion-weighted MRI could suggest malignant tumours, the characteristic “string sign” provided the clue for the diagnosis of schwannoma.
Core tip: There is a difference in an approach to surgery for benign and malignant parotid masses. For benign lesions, superficial parotidectomy is done; whereas in a case of malignant tumour total parotidectomy is performed with or without excision of the facial nerve. Clinically, it is very difficult to differentiate them because even malignant tumours have slow growth. Hence, here comes the role of imaging which could suggest the nature of the mass and narrow the differentials.
- Citation: Jaiswal A, Mridha AR, Nath D, Bhalla AS, Thakkar A. Intraparotid facial nerve schwannoma: A case report. World J Clin Cases 2015; 3(3): 322-326
- URL: https://www.wjgnet.com/2307-8960/full/v3/i3/322.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i3.322
Schwannomas of the Facial nerve (FN) are rare benign encapsulated neurogenic lesions. These can arise anywhere along its course[1,2]. Majority of these schwannomas are seen in the intratemporal course of the nerve whereas only 9% are seen in the extratemporal course[3]. In a case series of parotid tumours, schwannomas were found to be very rare accounting for only 2 out of 142 lesions[4]. As presentation is often nonspecific, preoperative diagnosis of these tumours is difficult[4].
Clinically these patients do not have any facial nerve dysfunction whereas postoperatively features of facial nerve paresis are common. Hence, it becomes extremely necessary for the surgeon to warn the patient regarding this complication beforehand.
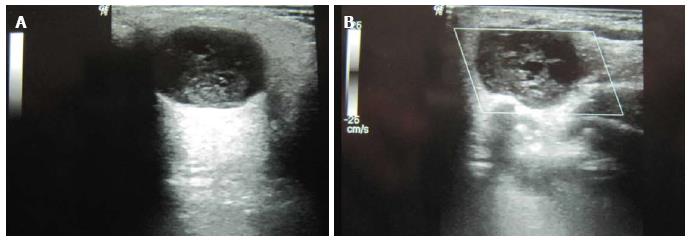
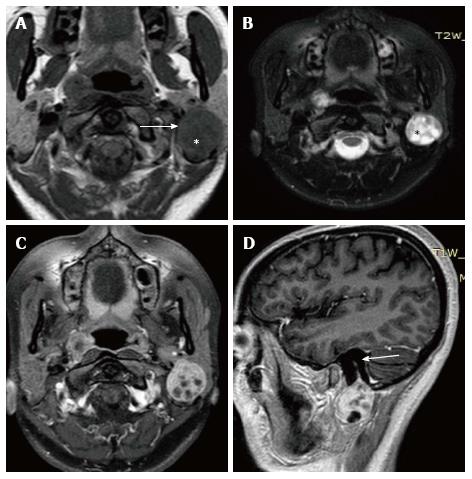
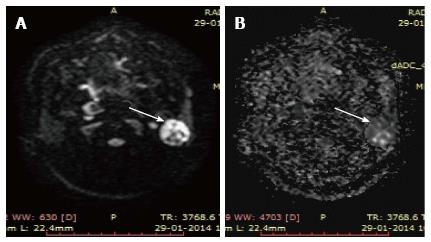
A 27-year-old healthy female presented in the surgical clinic with a slow growing painless swelling in the left retromandibular region for the last one year. There was no history of fever or any other constitutional symptoms. Physical examination revealed a soft, non-tender lump measuring approximately 3 cm × 2 cm. Laboratory tests such as complete haemogram, ESR, CRP were found to be within normal limits. Ultrasound examination showed the presence of a well defined, hypoechoic mass in the superficial lobe of left parotid which measured approximately 1.8 cm × 2.3 cm (Figure 1A). The mass showed anechoic areas within it with posterior acoustic enhancement suggestive of cystic component. No calcification or adjacent lymphadenopathy was seen. Color Doppler examination (Figure 1B) did not show any internal vascularity. The differential diagnoses were benign pathologies such as pleomorphic adenoma or less likely an intraparotid lymph node. For further characterisation of the lesion, MR examination of the parotid was performed. MR imaging (Figure 2) revealed a well-circumscribed mass lesion in the left parotid gland. The mass was located just below the stylomastoid foramen with a beak like protrusion into it representing the classic “string sign”. T1-weighted image (Figure 2A) showed the tumour to be of intermediate signal intensity compared to adjacent muscle, and T2-weighted image (Figure 2B) showed high signal intensity with interspersed areas of lower signal intensity. DWI (Figure 3) showed hyperintensity at b = 1000 s/mm2 suggestive of restricted diffusion in the solid part of the lesion with facilitated diffusion in the cystic part. On surgical exploration, the mass was found to be in close relationship with the main trunk of facial nerve just below stylomastoid foramen. Postoperatively, the patient developed mild facial paresis. The tumour was histopathologically confirmed to be schwannoma. The spindle cells were immunopositive with S-100 (Figure 4).
Schwannomas are benign nerve sheath tumours, composed entirely of differentiated neoplastic Schwann cells. Intraparotid FN schwannoma was first reported by Ibarz in 1927. Since then, fewer than 100 cases of FN schwannomas have been reported. In a study by Fortan et al[3], majority of the lesions were found within the intratemporal course, whereas about 9% of the tumours were found in the parotid gland[3]. The frequency of intraparotid schwannomas range from 0.2% to 1.5%[5]. Because of its low prevalence and very few typical clinical and radiological signs associated with it, preoperative diagnosis of intraparotid FN schwannoma is generally difficult.
In a case series of FN schwannomas, the most common clinical manifestation in intratemporal involvement of the nerve was facial nerve dysfunction, whereas in extratemporal course, it was a parotid mass without facial paresis[6].
In patients with a parotid mass, associated facial nerve palsy generally indicates malignancy. But it can also be seen in benign parotid masses such as pleomorphic adenoma and Warthin’s tumour. However, none has been reported in intraparotid schwannoma[7].
Similarly in our case, the patient presented with a parotid mass without facial nerve dysfunction, it thus became very difficult to clinically diagnose the schwannoma without the aid of imaging modalities. Ultrasound evaluation in our case showed a well-defined mass with cystic areas within it. Ultrasound when coupled with newer techniques like elastography can help in differentiating benign from malignant parotid masses[8].
MRI images showed that the mass was situated just below the stylomastoid foramen with beaking into the foramen producing the characteristic “string sign”. The string sign is due to the vertical orientation of soft tissue on either ends of the mass. The string represents the normal entering or exiting nerve that is in continuity with the nerve sheath tumour.
MRI features described in four cases of facial nerve schwannomas showed heterogeneous lesions that were isointense to brain on both T1- and T2-weighted images[9]. In the present case, the tumour was well defined, isointense and heterogeneously hyperintense to muscle on T1 and T2 weighted images respectively.
Schwannomas may exhibit “target” sign which is characterized by hyperintensity in the periphery while hypointensity in the centre on T2-weighted images. “Target sign” of neurofibroma is almost pathognomonic[10]. This feature is suggestive of neurogenic neoplasm[11]. In schwannomas, the target sign is due to compactly packed cellular Antoni A regions which is located centrally and loose myxomatous Antoni B regions in the peripheral part[11]. In our case, classical target sign was not observed.
Diffusion weighted imaging features of parotid schwannoma have not been previously described. Restricted diffusion in our case reflects high cellularity of the tumour, supporting the observation that restricted diffusion can be seen in both malignant and benign lesions[12].
Pleomorphic adenomas are the most common tumours of the parotid gland, and a close differential of intraparotid schwannoma due to it being well circumscribed, heterogeneous and hyperintense on T2W sequences[13]. But the presence of “string sign” reasonably excluded the possibility of pleomorphic adenoma in our case.
Adenoid cystic carcinoma, another close differential, is a malignant tumour that has the potential to spread along the nerve sheath[14]. Malignant tumours are hypointense on T2-weighted images and show ill-defined margins on post contrast images[15]. However, T2 hyperintensity and smooth enlargement of the facial nerve canal excludes this diagnosis[14].
In cases of painless swellings of the parotid gland without any neurological involvement, possibility of intraparotid schwannoma should be considered under differentials and the imaging modalities especially MRI revealing characteristic “string sign” further confirms the diagnosis.
The patient presented with a slow growing painless swelling in the retromandibular region on left side for the last 1 year.
The patient’s symptoms were nonspecific and presence of painless progressive swelling over a period of 1 year pointed to its benign nature.
Pleomorphic adenoma was ruled out as there was “string sign” showing extension along the facial nerve into the stylomastoid foramen. Adenoid cystic carcinoma was ruled out as the mass showed T2 hyperintensity and well defined margins. Malignant tumours are T2 hypointense with ill defined margins. Even extension into stylomastoid foramen was accompanied by smooth enlargement of the foramen without any irregular erosion.
Blood tests were non contributory.
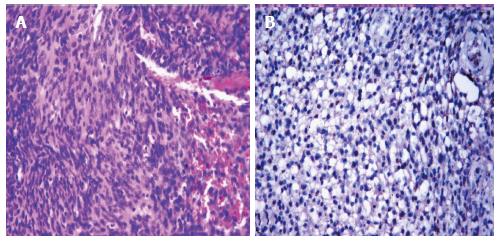
The excised tumour measured 2.5 cm × 2 cm. Cut surface was fleshy with focal haemorrhage. Microscopic examination showed cellular spindle cells arranged in fascicles. Tumour cells exhibited oval to elongated hyperchromatic nuclei, inconspicuous nucleolus, and fibrillary eosinophilic cytoplasm. Few thick walled blood vessels were seen. No mitosis or necrosis was seen. The tumour cells were immunopositive with S-100; while negative for smooth muscle actin and estrogen receptor. MIB-1 labelling index was < 2%. A diagnosis of schwannoma was given.
Under general anaesthesia, excision of the tumour mass was done and sent for histopathological examination.
Chung SY et al article Facial nerve schwannomas: Computed tomography and magnetic resonance findings published in 1998 in Yonsei Med J provide a brief but cumulative overview on the case topic.
Facial nerve schwannoma is a rare neurogenic tumour that arises from the schwann cells of the neurons.
One lesson that the authors learnt from this case was to consider facial nerve schwannoma in the differential diagnosis of parotid mass when a patient presents with painless progressive swelling and imaging shows characteristic “string sign”. Restricted diffusion reflects its high cellularity, supporting the observation that restricted diffusion can be seen in both malignant and benign lesions.
Good paper.
P- Reviewer: Mazzocchi M, Tsytsarev V S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | O’Donoghue GM, Brackmann DE, House JW, Jackler RK. Neuromas of the facial nerve. Am J Otol. 1989;10:49-54. [PubMed] |
| 2. | Symon L, Cheesman AD, Kawauchi M, Bordi L. Neuromas of the facial nerve: a report of 12 cases. Br J Neurosurg. 1993;7:13-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 73] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Forton GE, Moeneclaey LL, Offeciers FE. Facial nerve neuroma. Report of two cases including histological and radiological imaging studies. Eur Arch Otorhinolaryngol. 1994;251:17-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Balle VH, Greisen O. Neurilemmomas of the facial nerve presenting as parotid tumors. Ann Otol Rhinol Laryngol. 1984;93:70-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 5. | Chiang CW, Chang YL, Lou PJ. Multicentricity of intraparotid facial nerve schwannomas. Ann Otol Rhinol Laryngol. 2001;110:871-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Chung SY, Kim DI, Lee BH, Yoon PH, Jeon P, Chung TS. Facial nerve schwannomas: CT and MR findings. Yonsei Med J. 1998;39:148-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Nader ME, Bell D, Sturgis EM, Ginsberg LE, Gidley PW. Facial Nerve Paralysis due to a Pleomorphic Adenoma with the Imaging Characteristics of a Facial Nerve Schwannoma. J Neurol Surg Rep. 2014;75:e84-e88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Klintworth N, Mantsopoulos K, Zenk J, Psychogios G, Iro H, Bozzato A. Sonoelastography of parotid gland tumours: initial experience and identification of characteristic patterns. Eur Radiol. 2012;22:947-956. [RCA] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 53] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 9. | Martin N, Sterkers O, Mompoint D, Nahum H. Facial nerve neuromas: MR imaging: Report of four cases. Neuroradiology. 1992;34:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Suh JS, Abenoza P, Galloway HR, Everson LI, Griffiths HJ. Peripheral (extracranial) nerve tumors: correlation of MR imaging and histologic findings. Radiology. 1992;183:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 157] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Murphey MD, Smith WS, Smith SE, Kransdorf MJ, Temple HT. From the archives of the AFIP. Imaging of musculoskeletal neurogenic tumors: radiologic-pathologic correlation. Radiographics. 1999;19:1253-1280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 359] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 12. | Qayyum A. Diffusion-weighted imaging in the abdomen and pelvis: concepts and applications. Radiographics. 2009;29:1797-1810. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 262] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 13. | Ikeda K, Katoh T, Ha-Kawa SK, Iwai H, Yamashita T, Tanaka Y. The usefulness of MR in establishing the diagnosis of parotid pleomorphic adenoma. AJNR Am J Neuroradiol. 1996;17:555-559. [PubMed] |
| 14. | Teresi LM, Lufkin RB, Wortham DG, Abemayor E, Hanafee WN. Parotid masses: MR imaging. Radiology. 1987;163:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 70] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Christe A, Waldherr C, Hallett R, Zbaeren P, Thoeny H. MR imaging of parotid tumors: typical lesion characteristics in MR imaging improve discrimination between benign and malignant disease. AJNR Am J Neuroradiol. 2011;32:1202-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 157] [Article Influence: 11.2] [Reference Citation Analysis (0)] |